true0001541157false00015411572024-09-132024-09-130001541157dei:AdrMember2024-09-132024-09-130001541157aktx:OrdinarySharesParValue0.0001PerShareMember2024-09-132024-09-13
UNITED STATES
SECURITIES AND EXCHANGE COMMISSION
Washington, D.C. 20549
FORM 8-K
CURRENT REPORT
Pursuant to Section 13 or 15(d) of the
Securities Exchange Act of 1934
Date of Report (Date of earliest event reported): September 13, 2024
Akari Therapeutics, Plc
(Exact Name of Registrant as Specified in Charter)
|
|
|
|
|
England and Wales |
|
001-36288 |
|
98-1034922 |
(State or other jurisdiction
of incorporation) |
|
(Commission File Number) |
|
(I.R.S. Employer
Identification No.) |
22 Boston Wharf Road FL 7
Boston, MA 02210
(Address, including zip code, of Principal Executive Offices)
Registrant’s telephone number, including area code: (929) 274-7510
Check the appropriate box below if the Form 8-K filing is intended to simultaneously satisfy the filing obligation of the registrant under any of the following provisions:
|
|
¨ |
Written communications pursuant to Rule 425 under the Securities Act (17 CFR 230.425) |
¨ |
Soliciting material pursuant to Rule 14a-12 under the Exchange Act (17 CFR 240.14a-12) |
¨ |
Pre-commencement communications pursuant to Rule 14d-2(b) under the Exchange Act (17 CFR 240.14d-2(b)) |
¨ |
Pre-commencement communications pursuant to Rule 13e-4(c) under the Exchange Act (17 CFR 240.13e-4(c)) |
Securities registered pursuant to Section 12(b) of the Act:
|
|
|
|
|
Title of each class: |
|
Trading Symbol(s) |
|
Name of each exchange on which registered |
American Depositary Shares, each representing 2,000 Ordinary Shares |
|
AKTX |
|
The Nasdaq Capital Market |
Ordinary Shares, par value $0.0001 per share* |
|
|
|
|
*Trading, but only in connection with the American Depositary Shares.
Indicate by check mark whether the registrant is an emerging growth company as defined in Rule 405 of the Securities Act of 1933 (§230.405 of this chapter) or Rule 12b-2 of the Securities Exchange Act of 1934 (§240.12b-2 of this chapter).
Emerging growth company ¨
If an emerging growth company, indicate by check mark if the registrant has elected not to use the extended transition period for complying with any new or revised financial accounting standards provided pursuant to Section 13(a) of the Exchange Act. ¨
Item 5.02 Departure of Directors or Principal Officers; Election of Directors; Appointment of Principal Officers.
Appointment of Director
On September 13, 2024, the board of directors (the “Board”) of Akari Therapeutics, Plc (“Akari”) approved the expansion of the Board from five directors to six directors and the appointment of Robert Bazemore to serve as a director of the Board, effective as of September 17, 2024 (the “Effective Date”). Mr. Bazemore will serve as a Class A director with a term expiring at the Company’s 2025 Annual General Meeting of Shareholders or until his successor is duly elected and qualified or until his earlier resignation, death or removal.
The Board has determined that Mr. Bazemore is independent under the applicable Nasdaq listing rules. There are no arrangements or understandings between Mr. Bazemore and any other person pursuant to which he was selected as a director. There are no related party transactions between the Company and Mr. Bazemore (or any of his immediate family members) requiring disclosure under Item 404(a) of Regulation S-K. Mr. Bazemore does not have any family relationships with any of the Company’s directors or executive officers.
Mr. Bazemore will participate in the standard non-employee director compensation arrangements described under the heading “Director Compensation” contained in the Company’s proxy statement filed with Securities and Exchange Commission (the “SEC”) on June 3, 2024.
Amendment of Interim Chief Executive Officer Agreement
As previously disclosed, on April 25, 2024, the Board appointed Samir R. Patel, M.D., a member of the Board, as Interim President and Chief Executive Officer, effective May 1, 2024, to serve in such capacities until such time as determined by the Board. In connection with Dr. Patel’s appointment as Interim President and Chief Executive Officer, on May 31, 2024, the Company and Dr. Patel entered into an Interim Chief Executive Officer Agreement, effective as of May 1, 2024 (the “Interim CEO Agreement”).
On September 16, 2024, the Company entered into an amendment to the Interim CEO Agreement (the “Amendment”) to revise the compensation to be received by Dr. Patel in connection with the services as Interim President and Chief Executive Officer. Pursuant to the Amendment, in lieu of receiving his stated monthly compensation of $50,000 in the form of fully vested ordinary shares of the Company, par value $0.0001 per share (the “Ordinary Shares”), Dr. Patel shall be paid in the form of fully vested non-qualified stock options to purchase Ordinary Shares (“NQSOs”), with the number of American Depositary Shares (“ADSs”) underlying each such monthly NQSOs grant to be equal to two times the number determined by dividing (i) $50,000 by (ii) the closing price of the Company's ADSs on the Nasdaq Capital Market on the last day of each month (or partial month) Dr. Patel serves as the Company’s Interim President and Chief Executive Officer.
The foregoing description of the Amendment does not purport to be complete and is qualified in its entirety by reference to Amendment, which is filed as Exhibit 10.1 to this Form 8-K.
Item 8.01 Other Events.
As previously disclosed, on March 4, 2024, Akari entered into an Agreement and Plan of Merger, as amended by that certain side letter dated August 15, 2024 (the “Merger Agreement”) with Peak Bio, Inc. (“Peak Bio”) and Pegasus Merger Sub, Inc., a Delaware corporation and a wholly-owned subsidiary of Akari (“Merger Sub”), pursuant to which, upon the terms and subject to the conditions thereof, Merger Sub will be merged with and into Peak Bio (the “Merger”), with Peak Bio surviving the Merger as a wholly-owned subsidiary of Akari.
This Current Report on Form 8-K is being filed to provide updates to Akari’s business section.
Consummation of the Merger is subject to various conditions, including, among others, (i) approval of the Merger Agreement and Merger by Peak Bio stockholders, (ii) Akari’s shareholders authorizing Akari’s board of directors to allot all Akari ordinary shares to be issued in connection with the Merger (to be represented by ADSs), (iii) the absence of any law or order prohibiting consummation of the Merger, (iv) Akari’s Registration Statement on Form S-4 (filed
on September 13, 2024 in connection with the Merger) having been declared effective, (v) the Akari ADSs issuable to Peak Bio stockholders having been authorized for listing on the Nasdaq Stock Market LLC, (vi) accuracy of the other party’s representations and warranties (subject to certain materiality standards set forth in the Merger Agreement), (vii) compliance by the other party in all material respects with such other party’s obligations under the Merger Agreement; (viii) the absence of a material adverse effect on the other party, (ix) the other party’s net cash being greater than negative $13.5 million and (x) the PIPE Investment (as defined in the Merger Agreement) shall have been consummated simultaneously with, and conditioned only upon, the occurrence of the closing, and shall result in net proceeds to Akari of at least $10 million.
Forward-Looking Statements
This Current Report on Form 8-K contains forward-looking statements within the meaning of Section 27A of the Securities Act of 1933, as amended, and Section 21E of the Securities Exchange Act of 1934, as amended (the “Exchange Act”), about Akari and the Merger. Actual events or results may differ materially from these forward-looking statements. Words such as “will,” “could,” “would,” “should,” “expect,” “plan,” “anticipate,” “intend,” “believe,” “estimate,” “predict,” “project,” “potential,” “continue,” “future,” “opportunity” “will likely result,” “target,” variations of such words, and similar expressions or negatives of these words are intended to identify such forward-looking statements, although not all forward-looking statements contain these identifying words. These statements are based on Akari’s and Peak Bio’s current plans, estimates and projections. By their very nature, forward-looking statements involve inherent risks and uncertainties, both general and specific. A number of important factors, including those described in this communication, could cause actual results to differ materially from those contemplated in any forward-looking statements. Factors that may affect future results and may cause these forward-looking statements to be inaccurate include, without limitation: uncertainties as to the timing for completion of the Merger; uncertainties as to Peak Bio’s and/or Akari’s ability to obtain the approval of Akari’s shareholders or Peak Bio’s stockholders required to consummate the Merger; the possibility that competing offers will be made by third parties; the occurrence of events that may give rise to a right of one or both of Akari and Peak Bio to terminate the Merger Agreement; the possibility that various closing conditions for the proposed Merger may not be satisfied or waived on a timely basis or at all, including the possibility that a governmental entity may prohibit, delay, or refuse to grant approval, if required, for the consummation of the proposed Merger (or only grant approval subject to adverse conditions or limitations); the difficulty of predicting the timing or outcome of consents or regulatory approvals or actions, if any; the possibility that the proposed Merger may not be completed in the time frame expected by Akari and Peak Bio, or at all; the risk that Akari and Peak Bio may not realize the anticipated benefits of the proposed Merger in the time frame expected, or at all; the effects of the proposed Merger on relationships with Akari’s or Peak Bio’s employees, business or collaboration partners or governmental entities; the ability to retain and hire key personnel; potential adverse reactions or changes to business relationships resulting from the announcement or completion of the proposed Merger; significant or unexpected costs, charges or expenses resulting from the proposed Merger; the potential impact of unforeseen liabilities, future capital expenditures, revenues, costs, expenses, earnings, synergies, economic performance, indebtedness, financial condition and losses on the future prospects, business and management strategies for the management, expansion and growth of the combined business after the consummation of the proposed Merger; potential negative effects related to this announcement or the consummation of the proposed Merger on the market price of Akari’s American Depositary Shares or Peak Bio’s common stock and/or Akari’s or Peak Bio’s operating or financial results; uncertainties as to the long-term value of Akari’s American Depositary Shares (and the ordinary shares represented thereby), including the dilution caused by Akari’s issuance of additional American Depositary Shares (and the ordinary shares represented thereby) in connection with the proposed Merger; unknown liabilities related to Akari or Peak Bio; the nature, cost and outcome of any litigation and other legal proceedings involving Akari, Peak Bio or their respective directors, including any legal proceedings related to the proposed Merger; risks related to global as well as local political and economic conditions, including interest rate and currency exchange rate fluctuations; potential delays or failures related to research and/or development of Akari’s or Peak Bio’s programs or product candidates; risks related to any loss of Akari’s or Peak Bio’s patents or other intellectual property rights; any interruptions of the supply chain for raw materials or manufacturing for Akari or Peak Bio’s product candidates, the nature, timing, cost and possible success and therapeutic applications of product candidates being developed by Akari, Peak Bio and/or their respective collaborators or licensees; the extent to which the results from the research and development programs conducted by Akari, Peak Bio, and/or their respective collaborators or licensees may be replicated in other studies and/or lead to advancement of product candidates to clinical trials, therapeutic applications, or regulatory approval; uncertainty of the utilization, market acceptance, and commercial success of Akari’s or Peak Bio’s product candidates, and the impact of studies (whether conducted by
Akari, Peak Bio or others and whether mandated or voluntary) on any of the foregoing; unexpected breaches or terminations with respect to Akari’s or Peak Bio’s material contracts or arrangements; risks related to competition for Akari’s or Peak Bio’s product candidates; Akari’s or Peak Bio’s ability to successfully develop or commercialize Akari’s or Peak Bio’s product candidates; Akari’s, Peak Bio’s, and their collaborators’ abilities to continue to conduct current and future developmental, preclinical and clinical programs; potential exposure to legal proceedings and investigations; risks related to changes in governmental laws and related interpretation thereof, including on reimbursement, intellectual property protection and regulatory controls on testing, approval, manufacturing, development or commercialization of any of Akari’s or Peak Bio’s product candidates; unexpected increase in costs and expenses with respect to the potential transaction or Akari’s or Peak Bio’s business or operations; and risks and uncertainties related to epidemics, pandemics or other public health crises and their impact on Akari’s and Peak Bio’s respective businesses, operations, supply chain, patient enrollment and retention, preclinical and clinical trials, strategy, goals and anticipated milestones and other risks described in our reports filed from time to time with the SEC.
Additional Information and Where to Find It
In connection with the proposed Merger, on September 13, 2024, Akari and Peak Bio filed with the SEC a Registration Statement on Form S-4. The Registration Statement on Form S-4 includes a prospectus of Akari and a joint proxy statement of Akari and Peak Bio. INVESTORS AND SECURITY HOLDERS ARE URGED TO READ CAREFULLY THE REGISTRATION STATEMENT ON FORM S-4, JOINT PROXY STATEMENT/PROSPECTUS AND OTHER RELEVANT DOCUMENTS FILED OR WILL BE FILED WITH THE SEC, AS WELL AS ANY AMENDMENTS OR SUPPLEMENTS THERETO AND ANY DOCUMENTS INCORPORATED BY REFERENCE THEREIN, IN THEIR ENTIRETY IF AND WHEN THEY BECOME AVAILABLE BECAUSE THEY CONTAIN OR WILL CONTAIN IMPORTANT INFORMATION ABOUT THE PROPOSED MERGER, RELATED MATTERS AND THE PARTIES TO THE PROPOSED MERGER.
You may obtain a free copy of the Registration Statement on Form S-4, joint proxy statement/prospectus and other relevant documents (if and when they become available) that are or will be filed with the SEC for free at the SEC’s website at www.sec.gov. Copies of the documents filed with the SEC by Akari will be available free of charge on Akari’s website at http://investor.akaritx.com/ or by contacting Akari’s Investor Relations Department at http://investor.akaritx.com/investor-resources/contact-us. Copies of the documents filed with the SEC by Peak Bio will be available free of charge on Peak Bio’s website at https://peak-bio.com/investors or by contacting Peak Bio’s Investor Relations Department at https://peak-bio.com/contact.
Participants in the Solicitation
Akari, Peak Bio and their respective directors and executive officers and other members of management and employees may be deemed to be participants in the solicitation of proxies in respect of the proposed Merger. Information about the directors and executive officers of Akari, including a description of their direct or indirect interests, by security holdings or otherwise, is set forth in Akari’s Annual Report on Form 10-K for the year ended December 31, 2023 filed with the SEC on March 29, 2024, subsequent quarterly and current reports on Form 10-Q and 8-K, respectively, and other documents that may be filed from time to time with the SEC. Information about the directors and executive officers of Peak Bio, including a description of their direct or indirect interests, by security holdings or otherwise, is set forth in Peak Bio’s proxy statement for its 2022 Special Meeting of Stockholders, which was filed with the SEC on October 19, 2022, the Annual Report on Form 10-K for the year ended December 31, 2023 filed with the SEC on August 6, 2024, subsequent quarterly and current reports on Form 10-Q and Form 8-K, respectively, and other documents that may be filed from time to time with the SEC. Other information regarding the participants in the proxy solicitations and a description of their direct and indirect interests, by security holdings or otherwise, is contained in the joint proxy statement/prospectus included in the Registration Statement on Form S-4 and other relevant materials filed and to be filed with the SEC regarding the proposed Merger when such materials become available. Security holders, potential investors and other readers should read the joint proxy statement/prospectus, included in the Registration Statement on Form S-4 carefully before making any voting or investment decision. You may obtain free copies of these documents from Akari or Peak Bio using the sources indicated above.
Item 9.01. Financial Statements and Exhibits.
(d) Exhibits
SIGNATURES
Pursuant to the requirements of the Securities Exchange Act of 1934, the registrant has duly caused this report to be signed on its behalf by the undersigned hereunto duly authorized.
|
|
|
|
Akari Therapeutics, Plc |
|
|
Date: September 18, 2024 |
By: |
/s/ Samir R. Patel, M.D. |
|
|
Samir R. Patel, M.D. |
|
|
Interim President and Chief Executive Officer |
AMENDMENT TO
INTERIM CHIEF EXECUTIVE OFFICER AGREEMENT
This Amendment (this “Amendment”) to the Interim Chief Executive Officer Agreement (the “Interim CEO Agreement”), effective May 1, 2024, between Samir R. Patel, M.D. (“Interim CEO”) and Akari Therapeutics, Plc (the “Company”) is effective as of July 1, 2024. All capitalized terms used herein but not otherwise defined shall have the meaning given to such terms in the Interim CEO Agreement.
WHEREAS, the Company and Interim CEO desire to modify the compensation provisions of the Interim CEO Agreement as set forth below.
NOW, THEREFORE, the Interim CEO Agreement is modified as set forth below:
1. Exhibit A to the Interim CEO Agreement is hereby amended and restated as set forth on Exhibit A to this Amendment.
2. Except as modified by this Amendment, the Interim CEO Agreement is in all other respects hereby in full force and effect and is hereby confirmed.
3. This Amendment, together with the Interim CEO Agreement, constitutes the entire understanding and agreement of the parties with respect to the transactions contemplated herein and supersedes all prior and contemporaneous understandings and agreements, whether written or oral, with respect to such transactions, except that this Amendment does not supersede any confidentiality, intellectual property assignment, non-solicitation or other restrictive covenant between Interim CEO and the Company.
4. This Amendment may be executed in any number of counterparts, each of which shall be an original, but all of which together constitute one instrument. Counterparts of this Addendum (or applicable signature pages hereof) that are manually or electronically signed and delivered by email transmission shall be deemed to constitute signed original counterparts hereof and shall bind the parties signing and delivering in such manner.
[Remainder of Page Intentionally Left Blank]
|
|
AKARI THERAPEUTICS, PLC |
|
|
|
|
By: |
/s/ Raymond Prudo |
|
|
Name: |
Raymond Prudo |
|
|
Title: |
Chairman |
|
|
|
|
SAMIR R. PATEL, M.D. |
|
|
|
|
By: |
/s/ Samir R. Patel, M.D. |
|
Name: |
Samir R. Patel, M.D. |
|
|
EXHIBIT A
SERVICES
Interim CEO’s “Services” under the Interim Chief Executive Officer Agreement shall be providing such services appropriate for the Chief Executive Officer of Akari as prescribed by Akari’s Board of Directors of from time to time. Interim CEO will report to the Akari’s Board of Directors.
COMPENSATION
As exclusive compensation for the Services and the rights granted to the Company in this Agreement, during the Term, the Company will compensate Interim CEO as follows:
1.$50,000 per month. Such compensation will be paid in in the form of fully vested non- qualified options to purchase Ordinary Shares, $0.0001 par value per share, of Akari (“NQSOs”), which NQSOs will be issued within a reasonable period of time following the end of each quarter (or partial quarter) worked and the number of American Depositary Shares (“ADSs”) underlying each monthly NQSO grant will be equal to two times the number determined by dividing $50,000 (pro-rated for any partial month worked as Interim Chief Executive Officer of the Company) by the closing price of the ADSs on the Nasdaq Capital Market on the last day of each month (or partial month) worked; and
2.Reasonable travel expenses incurred by Interim CEO in completing the Services and that are documented and submitted to the Company in accordance with the Company’s standard policies and procedures regarding reimbursement will be reimbursed by the Company as soon as reasonably practicable. Interim CEO will not be eligible for reimbursement for any other expenses incurred by Interim CEO in connection with the Services.
For the avoidance of doubt, Interim CEO will not be entitled to any other compensation from the Company for the Services, including without limitation, any bonuses or severance payments or benefits.
BUSINESS OF AKARI
Overview
Akari is a biotechnology company focused on developing advanced therapies for autoimmune and inflammatory diseases involving the complement component 5 (“C5”) and leukotriene B4 (“LTB4”) pathways. Each of these pathways has scientifically well-supported causative roles in the diseases we are targeting. Akari believes that blocking these two early mediators of inflammation will prevent initiation and continual amplification of the processes that cause certain diseases. Akari’s activities since inception have consisted of performing non-clinical and clinical research and development activities and raising capital.
Akari’s lead asset, nomacopan, is a recombinant small protein (16,769 Da) derived from a protein originally discovered in the saliva of the Ornithodoros moubata tick, which modulates the host immune system to allow the parasite to feed without alerting the host to its presence or provoking an immune response. Nomacopan is a second-generation complement inhibitor which has been shown to act on complement C5, preventing release of C5a and formation of C5b-9 (also known as the membrane attack complex (“MAC”)). Nomacopan also specifically sequesters and inhibits LTB4. Complement C5 and LTB4 activation and their proinflammatory actions are typically co-localised during an immune reaction. With its unique bispecific mode of action and biophysical properties, Akari believes nomacopan may be able to prevent inflammatory and prothrombotic activities of these two important pathways and also and has the potential to be formulated for administration by a variety of routes including subcutaneous, intravenous, topical to eye, inhaled and intravitreous.
Akari is investigating PAS-nomacopan, a long-acting form of nomacopan that is a bispecific inhibitor of C5 and LTB4, for the intravitreal treatment of geographic atrophy (“GA”) secondary to dry age-related macular degeneration (“AMD”) in preclinical studies. Following a positive and constructive Pre-Investigational New Drug application meeting with FDA in August 2024, Akari is completing final non-clinical studies and Good Manufacturing Practices (“GMP”) manufacturing and expects to file an Investigational New Drug Application (“IND”) with the FDA in 2025 for PAS-nomacopan in GA. Akari believes PAS-nomacopan has the potential for longer dose intervals between intravitreous injections than currently approved complement only inhibitors, as well as potential reduction of the choroidal neovascularization (“CNV”) risk that is associated with approved inhibitors. CNV is a sight-threatening over development of blood vessels within the retina, which is typically treated with anti-vascular endothelial growth factor (“VEGF”) intravitreal injections. As a bispecific inhibitor of complement C5 and LTB4 we believe PAS-nomacopan may be more efficacious than marketed treatments for GA that only inhibit complement.
Until May 2024, Akari was conducting a clinical trial of subcutaneous nomacopan for the treatment of hematopoietic stem cell transplantation-associated thrombotic microangiopathy (“HSCT-TMA”) in pediatrics. Following completion of a portfolio prioritization review, Akari announced that Akari’s HSCT-TMA program will be suspended, as more fully described below.
Pipeline Prioritization of the Merged Companies
In May 2024, Akari announced the completion of a joint portfolio prioritization review pursuant to which the anticipated combined entity, following completion of the proposed Merger, will focus on Peak Bio’s antibody drug conjugates (“ADC”) platform technology and Akari’s PAS-nomacopan GA program. As a result, Akari’s HSCT-TMA program was suspended, with enrollment in its pediatric clinical study discontinued due to cost and timeline. Following the anticipated Closing of the proposed Merger in the fourth quarter of 2024, Akari expects to have an expanded pipeline of assets spanning early and late development stages with the addition of Peak Bio’s ADC toolkit with novel payload and linker technologies as well as the Peak Bio PHP-303 small molecule selective and reversible neutrophil elastase inhibitor. The ADC program includes a novel pre-clinical ADC candidate targeting TROP-2. By combining chemotherapy with immunotherapy strategies, Akari aims to develop cutting-edge solutions for cancer patients. Further, related to PHP-303, Akari expects to emphasize partnering/collaboration and licensing opportunities with broad potential impact on patients. Further, Akari plans to work closely with the FDA to define the best path for this platform and will pursue opportunities for external partnering/collaboration and licensing for nomacopan, including as a potential treatment for pediatric HSCT-TMA.
Research and Development
Current Akari Pipeline
Akari is currently developing potentially life-transforming treatments for autoinflammatory diseases involving the complement C5 and LTB4 pathways. Akari’s current pipeline prior to closing the Merger includes its pre-clinical ophthalmology program investigating PAS-nomacopan for treatment of GA secondary to dry AMD and Akari expects to file an IND application with the FDA in 2025.
Development of PAS-nomacopan for Geographic Atrophy
Nomacopan administered by daily subcutaneous injection appears to be a well tolerated drug in Phase 1, 2 and 3 clinical trials in a total of 76 subjects. Furthermore, it appears to significantly reduce the need for blood transfusions in paroxysmal nocturnal hemoglobinuria (“PNH”) patients who were transfusion dependent before starting treatment with nomacopan. In all, 19 PNH patients have received nomacopan for a cumulative total daily exposure of 32 years. Preclinical and clinical studies have demonstrated that once daily subcutaneous nomacopan may also ameliorate the symptoms of bullous pemphigoid.
To improve the pharmacokinetic and pharmacodynamic properties of nomacopan, Akari developed PAS-nomacopan to enable a less frequent dose interval. Initial work focused on PAS-nomacopans potential systemic use via either intravenous or subcutaneous administration and demonstrated that the half-life of PAS-nomacopan in mice is extended by approximately 52-fold compared to the half-life of nomacopan.
In 2019 Akari realized that PAS-nomacopan administered intravitreously might be well suited for treatment of diseases of the back of the eye due to its expected long half-life within the eye because of its large hydrodynamic radius (9.32nm compared to 2.45nm for nomacopan) and mounting evidence of roles for both C5 and LTB4 activation in. the pathology of eye diseases.
During 2020 and 2021, Akari announced preclinical data comparing the therapeutic efficacy of nomacopan, long acting PAS-nomacopan, and a monoclonal anti-VEGF antibody all administered intravitreally. PAS-nomacopan was found to reduce intraocular VEGF levels by as much as the anti-VEGF antibody with 74% (p=0.04) and 68% (p=0.05) reductions respectively, compared to saline control. Furthermore, based on a score assessing disease severity, inflammation increased in both the control and anti-VEGF groups by 49% and 33%, respectively, whereas PAS-nomacopan treatment showed a 9% reduction in inflammation assessed by retinal fundoscopy (p=0.02). This therapeutic activity across multiple pathogenic pathways (VEGF, inflammation and complement) supports the potential for nomacopan as a new mode of action for the treatment of back of the eye diseases.
During the fourth quarter of 2020, Akari announced the publication of the results of a two-year research collaboration with the UCL Institute of Ophthalmology. The results showed that the therapeutic intravitreal (“IVT”) administration of long-acting PAS-nomacopan mitigated both the severity and progress of retinal damage in two retinal tissue models of autoimmune uveitis, a severe inflammatory eye disease where steroids are the primary treatment option. In addition, results showed the presence of inflammatory cells expressing both complement C5 and LTB4 receptors in retinal tissue from donor patients with uveitis as compared to healthy donor eyes and that PAS-nomacopan likely primarily via inhibition of LTB4 decreases Th17 T cells and IL17, that are present at elevated levels in GA and other retinal diseases.
During the second quarter of 2022, Akari announced positive results from two preclinical studies of PAS-nomacopan administered intravitreally. These preclinical studies confirmed the bioavailability of PAS-nomacopan in the retina and suggested that a clinical dose interval of three months or more may be possible. The preclinical study in a laser induced mouse model of CNV indicated that PAS-nomacopan may be able to inhibit CNV. Studies have shown that due to adverse effects, such as infection, increase in intraocular pressure (“IPO”) and discomfort and anxiety, IVT injection presents a heavy burden on patients therefore a longer dosing interval may be beneficial.
During the third quarter of 2022, Akari announced further positive results from these pre-clinical studies on the tolerability and extended dose interval of long-acting PAS-nomacopan, which, together with data previously presented, suggest PAS-nomacopan has the potential to be a novel treatment option for GA, a chronic progressive
degeneration of the macula in the aging eye leading to lesions on the outer retina that can cause irreversible vision loss. There are currently two FDA-approved therapies for treatment of GA. Both are complement inhibitors (IzervayTM, a C5 inhibitor and SyfovreTM, a C3 inhibitor); that are administered to patients through monthly or every-other-month intravitreous injections into the eye (“IVTs”). Frequent needle injections into the eye can be a source of fear, discomfort, disruption for patients and may decrease patient compliance with optimal dosing regimens.
Akari’s preclinical data, indicating a half-life in rabbit vitreous of 7.4 to 8.4 days suggest it may be possible to inject PAS-nomacopan at intervals of three-months or longer which Akari believes would be less burdensome and more attractive for patients. Sight-threatening CNV is a safety risk associated with complement-only inhibitors used for the treatment of GA. CNV is typically treated with anti-VEGF injections. Currently approved GA treatments have shown increased risks of developing CNV in clinical trials 4X and 2X compared to sham, respectively. Akari believes that dual-action PAS-nomacopan may offer the well-understood benefits of complement C5 inhibition in slowing the progression of GA lesions, while LTB4 inhibition has the potential to help prevent VEGF-A over-expression, a key driver of CNV.
In July 2023, Akari announced completion of Akari’s evaluation of potential PAS-nomacopan candidates and selected a single drug candidate to move forward into further development in GA, including clinical trials for GA, pending IND clearance.
In November 2023, Akari presented a poster on Akari’s pre-clinical development of long-acting PAS-nomacopan as a potential treatment for GA at the 4th Annual Dry AMD Therapeutic Development conference. Akari believes positive pre-clinical results and an advanced high yielding manufacturing process support the potential submission of an IND to evaluate the safety and pharmacokinetics/pharmacodynamics (PK/PD) of a single and repeat dose intravitreous PAS-nomacopan.
Immunogenicity
The immunogenicity of PAS-nomacopan will be evaluated during final non-clinical studies prior to IND submission, and if cleared by the FDA, during a phase 1 clinical trial of PAS-nomacopan. Akari’s experience with nomacopan, the active moiety in PAS-nomacopan, may be of some relevance. Low titer anti-drug antibodies (“ADA”) are detected in patients dosed chronically with nomacopan, however no neutralizing antibodies have been detected to date in clinical studies since drug levels do not fall in the presence of the ADA and pharmacodynamic analyses show that terminal complement activity was fully inhibited (ELISA CH50 <10 U Eq/mL) by nomacopan throughout dosing. Nomacopan was well tolerated with no observations of antibody mediated severe reactions at sites of injection.
Similar observations were made in mice receiving 28 days of daily subcutaneous nomacopan. The data showed nomacopan was well-tolerated with no injection site allergic reactions or behavioral changes. Nomacopan induced formation of low titre anti-drug IgG antibodies in mice after 2 to 4 weeks of daily inoculation but these antibodies were not neutralizing and had no effect on nomacopan’s ability to inhibit complement.
PAS-Nomacopan
Using PASylation®, a proprietary technology licensed from of XL-protein GmbH (“XL-protein”), nomacopan can be modified to generate PAS-nomacopan a long-acting form of nomacopan. The unstructured and uncharged PAS polypeptide greatly increases the apparent molecular size of the drug, slowing kidney clearance and extending the systemic half-life of nomacopan.
Recombinant PAS-nomacopan (67.8 kDa) is a 751 amino acid (“aa”) protein comprising 150 aa nomacopan and a 601 aa PAS polypeptide repeat fused in frame to the N-terminal of nomacopan (Figure A) which plays no part in binding to complement C5 or LTB4.
Figure A. Crystal Structure of Nomacopan Protein (gold) Bound to LTB4 (green) with PAS Polypeptide (red) Fused in Frame to N-terminus of Nomacopan

The PAS 600 amino acid repeat forms a random coil polypeptide. PASylation® has a similar effect to PEGylation and greatly increases the hydrodynamic radius and apparent molecular weight of the modified drug thereby extending half-life and potentially improving the drugs pharmacodynamic properties. The PAS polypeptide is hydrophilic and uncharged at neutral pH and was designed to be resistant to proteases found within the body.
Preclinical studies demonstrate that PAS-nomacopan inhibits complement C5 activation as potently as the non-PASylated protein nomacopan but has a 52-fold extended half-life when injected intravenously into mice of 10.4 + 2.2 hours for PAS-nomacopan versus 0.2 + 0.1 hours for nomacopan. The greatly increased half-life of PAS-nomacopan is reflected in the apparent molecular weight of PAS-nomacopan compared to nomacopan estimated by size exclusion chromatography (624 kDa and 28 kDa respectively) and the hydrodynamic radius determined by dynamic light scattering (9.32 nm and 2.45 nm and respectively).
The hydrodynamic radius of a drug has been found to be positively associated with its expected half-life within the eye. By increasing nomacopan’s hydrodynamic radius from 2.45 nm to 9.32 nm by PASylation®, an IVT dose interval of 3 months or even longer may be possible for PAS-nomacopan for treatment of GA.
PAS-Nomacopan for GA
GA is a chronic progressive degeneration of the macula and is an advanced form of dry age-related macular degeneration (“dAMD”) predominantly diagnosed in people over the age of 50 years. The disease, which can lead to irreversible vision loss, is characterized by localized sharply demarcated atrophy (lesions) of outer retinal tissue, retinal pigment epithelium (“RPE”) and choriocapillaris. GA typically (50-65% of the time) starts in the perifoveal region and in a median 2.5 years expands to involve the fovea, leading to central scotomas and permanent loss of visual acuity. The median time to development of GA in both eyes is 7 years from development of GA in the first eye. An estimated 5 million people worldwide are affected, with an estimated 1 to 1.6 million in the United States alone. The prevalence of GA increases with age. In the US, the estimated prevalence is approximately 0.81% having the atrophic form in at least one eye which increases to approximately 3.5% in patients aged 75 years and older. Akari believes GA is an underdiagnosed disease, with only 25% of patients diagnosed in the US and 50% of those patients presenting with bilateral disease (disease in both eyes). While there are two FDA approved treatments for the disease, which are both complement inhibitors, there is still significant unmet need for patients, including the frequency of therapy and risks of CNV that occurs at higher rates in patients treated with both approved therapies.
Preclinical Characterization of PAS-nomacopan
Tight Binding to C5 and LTB4 and Potent Terminal Complement Inhibition Demonstrated
The C5 and LTB4 binding kinetics and affinity of PAS-nomacopan (KD c.25pM for C5 and c. 255pM for LTB4) is comparable to that of non-PASylated nomacopan (KD c.100pM for C5 and c.130pM for LTB4) determined by means of surface plasmon resonance (“SPR”) and fluorescence titration (Figure B). In vitro PAS-nomacopan also inhibits complement mediated lysis of RBCs at least as effectively as non-PASylated nomacopan (Figure C).
Figure B. Illustrative Binding Kinetics of PAS-Nomacopan to C5 and LTB4

A) Cartoon of setup used for SPR. B) Single cycle kinetic experiment on Biacore X100 instrument (Cytivia). A CM3 sensorchip (Cytivia) was covalently conjugated with 5400 RU Avi-PA(S)®-Mab1.1 (XL-protein) and charged with 38 RU PAS-nomacopan using HBS 0.05% Tween 20 as running buffer at a flow rate of 30uL/min. A dilution series of pure human C5 complement (Complement Technologies) was then injected. After each cycle, the chip was regenerated with 30uL 10mM glycine pH 2.4. C) Fluorescence titration of PAS-nomacopan with LTB4 (Cayman Chemicals). The protein (100nM or 30nM) was dissolved in phosphate buffered saline (“PBS”) and excited at 280nM. Fluorescence was measured at 340/316 nm at 20ºC. Data points were fitted according to the law of mass action for a single ligand binding site.
Figure C. PAS- Nomacopan Inhibits Human Complement and Lysis of Human Erythrocytes as Potently as Nomacopan

Coversin= non-PASylated nomacopan; Coversin = nomacopan; PAS-Coversin = PAS-nomacopan; NC = negative control; PC = positive control
a) Effect of PAS-nomacopan and nomacopan on complement activation by the classical pathway (“CP”). Microtiter plates were coated with human IgM in the presence of Mg2+ and Ca2+ ions to allow activation of the CP. PAS-nomacopan and nomacopan were applied in dilution series in PBS containing 1% v/v human serum. After washing complement activation was detected with a specific alkaline phosphatase labelled antibody directed against the C9 neoantigen that emerges during formation of the MAC. Experiments were performed in triplicate (mean values and SDs are shown). Absorbance values were fitted to a sigmoidal dose response curve. b) Effect of PAS-nomacopan and nomacopan on complement activation by the alternative pathway (AP). Microtiter plates were coated with LPS in the presence of Mg2+ ions and EGTA to specifically activate the AP. PAS-nomacopan and nomacopan were
applied in dilution series in PBS containing 5% v/v human serum. Washing, MAC detection and controls were performed as described for the CP assay. Positive and negative controls were 100% lysis and heat inactivated serum respectively. Experiments were performed in triplicate (mean values and SDs are shown). Absorbance values were fitted to a sigmoidal dose response curve. c) Human erythrocytes were sensitised by incubation with 2-aminoethylisothiouronium bromide (“AET”) which cleaves GPI-anchored proteins (including the complement regulators CD59 and CD55) from the surface of cells. Acidified human serum with and without dilution series of nomacopan or PAS-nomacopan was incubated with the sensitised erythrocytes. After centrifugation, lysis was determined by measuring absorbance at 405nm, thus quantifying released hemoglobin, and normalised against PBS and PBS-ethylenediaminetetraacetic acid (“PBS-EDTA”) in place of active drug which provide 100% and 0% lysis respectively. Controls were analysed in quadruplicate and all other samples in triplicate. Relative absorbance values (+SD) were fitted to a sigmoidal dose response curve.
Evidence that PAS-nomacopan may allow less frequent intravitreous dosing than current GA therapies
To investigate the effect of PASylation on systemic half-life the PK parameters of PAS-nomacopan and nomacopan were determined in female BALB/c (IV) or C57BL/6J (SC) mice after bolus injection at a dose of 137 nmol/kg. Plasma concentrations of the administered protein were quantified at various time points using a sandwich ELISA. In the case of the IV bolus, the nomacopan showed quick monoexponential decay whereas PAS-nomacopan exhibited biexponential decay with much lower slope for the terminal elimination phase. The PK profile for the SC administration of PAS-nomacopan revealed distinct resorption and plasma elimination phases as expected. PASylation of nomacopan results in much slower (52-fold slower) systemic clearance, plausibly by reducing the rate of kidney filtration, leading to a prolonged half-life compared to nomacopan (Figure D and Table A).
Figure D. PK Profile of nomacopan (IV) and PAS-nomacopan (IV and SC) in Mice

Table A. Nomacopan and PAS-Nomacopan PK Parameters
|
|
|
|
|
|
|
|
|
|
Parameters |
|
Nomacopan (IV) |
|
PAS-nomacopan (IV) |
Terminal plasma half-life (h) |
|
0.2 ± 0.1 |
|
10.4 ± 2.2 |
Area under the curve; AUC (nM*h) |
|
682 ± 168 |
|
13,285 ± 1,836 |
Clearance; CL (h /mL*kg) |
|
201 ± 50 |
|
10.3 ± 1.4 |
AUC = area under the curve; CL = clearance; PK = pharmacokinetic
To verify that the substantially increased plasma half-life translates into a prolonged residence in the eye after intravitreous administration a non-Good Laboratory Practices (“GLP”) single dose IVT PK and tolerability study was conducted in New Zealand White (“NZW”) and Dutch belted (“DB”) rabbits using PAS-nomacopan proven to be endotoxin free by monocyte activation test. The objective of the PK portion of this study was to assess the ocular and systemic PK profile of highly purified PAS-nomacopan following a single IVT injection in NZW rabbits. Briefly, groups of NZW rabbits were injected intravitreously with either 20 mg/mL or 60 mg/mL highly purified PAS-nomacopan (proven to have undetectable endotoxin by monocyte activation test) and followed for 28 days. To assess nomacopan exposure profile, groups of 3 animals were sacrificed on days 1 (≤15 minutes post dose), 3, 7, 14 and 28. PAS-nomacopan concentration in eye tissue and plasma was measured. The plasma and eye tissue samples were analysed by a bespoke LC/MS that detects a specific 25 amino acid PAS-nomacopan peptide produced by enzymatic digestion with endoproteinase Lys-C and uses an internal control (“PAS-L-nomacopan”) to assess digestion efficiency. PAS-L-nomacopan has a different 25 amino acid sequence than PAS-nomacopan which allows their separate quantification by MS. The LC/MS method was qualified for use with vitreous, retina and choroid/RPE (“Ch/RPE”) and plasma with lower limits of detection and quantification (“LLOD” and “LLOQ”) established.
The PK profile of PAS-nomacopan is presented in Figure E and PK parameters in vitreous, retina and choroid RPE are summarised in Table B. The estimated half-life in vitreous was between 7.4 and 8.4 days with a proportionate dose related increase in drug concentrations in all eye tissues with about 20 - 25% of the vitreous drug concentration present in retina and RPE/choroid (Figure E). The estimated half-life in rabbit vitreous is relatively long for a biological drug, for example aflibercept (Eylea) which is dosed every 2 months for treatment of neovascular AMD, has an estimated half-life in rabbit vitreous of c.4.8 days (see Supplementary Table 1 in Crowell et al., 2019) and the estimated half-lives of SYFOVRE™ and IZERVAY™ in non- human primates are considerably shorter than that of aflibercept supporting the potential for a nomacopan dosing interval of 3 months or longer for treatment of GA.
Figure E. Vitreous and Retinal Drug Concentrations in NZW Rabbits after Single IVT Dose of PAS-nomacopan

Table B. Summary of PAS-nomacopan Pharmacokinetic Parameters in New Zealand White Rabbit Ocular Tissue
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
PAS-nomacopan in vitreous (V) |
|
|
PAS-nomacopan in retina (R) |
|
|
PAS-nomacopan in RPE/choroid
(RPE/choroid) |
|
|
|
20mg/mL
PAS-nomacopan |
|
|
60mg/mL
PAS-nomacopan |
|
|
20mg/mL
PAS-nomacopan |
|
|
60mg/mL
PAS-nomacopan |
|
|
20mg/mL
PAS-nomacopan |
|
|
60mg/mL
PAS-nomacopan |
|
Cmax |
|
|
726 |
|
|
|
1,419 |
|
|
|
354 |
|
|
|
2,118 |
|
|
|
382 |
|
|
|
1,568 |
|
Tmax |
|
|
0 |
|
|
|
3 |
|
|
|
0 |
|
|
|
0 |
|
|
|
0 |
|
|
|
0 |
|
t1/2 |
|
|
7.4 |
|
|
|
8.4 |
|
|
|
6.0 |
|
|
|
7.0 |
|
|
|
4.6 |
|
|
|
5.5 |
|
AUC (0-28 days) |
|
|
6,936 |
|
|
|
17,172 |
|
|
|
1,946 |
|
|
|
7,802 |
|
|
|
2,043 |
|
|
|
7,280 |
|
Ch = choroid; LLOD = lower limit of detection; V=vitreous; R=retina; RPE/choroid = retinal pigment epithelium/choroid;
Time-point 0 = <15 min after injection.
Number of rabbits per time-point = 3
Cmax = the highest mean value measured (µg/g or µg/mL of tissue)
Tmax = time-point when the highest mean value is measured (day)
t1/2 = ln(2) / (-a) with a = slope of ln (concentration) = f(t) (days). Calculated with AUC remaining >20% instead of <20%, only for information
AUC0-28 days = area under the curve in µg/g or µg/mL of tissue x day PAS-nomacopan concentration was not assessed in plasma samples due a lack of sensitivity (LC/MS assays LLOQ of 50 ug/mL) in rabbit plasma. Further work will be conducted to develop and qualify a bioanalytical ELISA assay of sufficient sensitivity to support analysis of drug concentrations in plasma in the planned toxicity studies to support the initial IND.
Completed PAS-nomacopan Toxicology Studies
A non-GLP single dose IVT ocular tolerability/toxicity studies in NZW and DB rabbits was completed using highly purified PAS-nomacopan (proven to have undetectable endotoxin by monocyte activation test), Before submitting the IND for GA planned additional studies for PAS-nomacopan will include a non-GLP single dose range-finding (“DRF”) study in minipigs, and GLP-compliant 3-month repeated dose IVT toxicology studies in rabbits and minipigs. Data from completed ocular tolerability studies in rabbits will be used for dose selection in the GLP-compliant 3-month repeated dose study, and no further ocular tolerability or DRF studies are planned in the rabbit. FDA have agreed at Pre-IND that minipig and DB rabbit are appropriate species for these IND enabling studies.
The objective of the tolerability study was to compare the ocular tolerability of a highly purified PAS-nomacopan formulation with that of the non-highly purified PAS-nomacopan formulation following a single intravitreous injection in DB and NZW rabbits.
Groups of male DB and female NZW rabbits were injected IVT with either 20 mg/mL or 60 mg/mL more highly purified PAS-nomacopan with undetectable pyrogen levels by monocyte activation test and followed for 28 days (Table C). Animals received a single 50uL IVT dose of the following treatments into their right eye (their left eye was untreated):
•Treatment A: 60 mg/mL of highly purified PAS-nomacopan (Batch XLMG260)
•Treatment B: 20 mg/mL of highly purified PAS-nomacopan (Batch XLMG220)
•Treatment C: Vehicle (PBS)
•Treatment D: 20 mg/mL non-highly purified PAS-nomacopan (Batch P/20180327/1232/138)
Table C. Study Design: Ocular Tolerability Following A Single IVT Administration in Albino and Pigmented Rabbits (A163GB26921 - Tolerability Only)
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Gr. |
|
Treatment |
|
|
Conc.
(mg/mL) |
|
|
Strain b |
|
Route,
Duration |
|
|
Number of Animals |
|
|
|
|
|
|
Sacrifice Day |
|
|
1 c |
|
|
3 |
|
|
7 |
|
|
14 |
|
|
28 |
|
1 |
|
|
A |
|
|
|
60 |
|
|
NZW |
|
|
|
|
|
|
3 |
|
|
|
3 |
|
|
|
3 |
|
|
|
3 |
|
|
|
3 |
|
2 |
|
|
B |
|
|
|
20 |
|
|
NZW |
|
|
|
|
|
|
3 |
|
|
|
3 |
|
|
|
3 |
|
|
|
3 |
|
|
|
3 |
|
3 |
|
|
C |
|
|
|
0 |
|
|
NZW |
|
|
|
|
|
|
3 |
|
|
|
3 |
|
|
|
3 |
|
|
|
3 |
|
|
|
3 |
|
4 |
|
|
D |
|
|
|
20 |
|
|
NZW |
|
|
IVT, SD |
|
|
|
3 |
|
|
|
3 |
|
|
|
3 |
|
|
|
3 |
|
|
|
3 |
|
5 |
|
|
B |
|
|
|
20 |
|
|
DB |
|
|
|
|
|
|
2 |
|
|
|
- |
|
|
|
- |
|
|
|
2 |
|
|
|
2 |
|
6 |
|
|
C |
|
|
|
0 |
|
|
DB |
|
|
|
|
|
|
2 |
|
|
|
- |
|
|
|
- |
|
|
|
2 |
|
|
|
2 |
|
7 |
|
|
D |
|
|
|
20 |
|
|
DB |
|
|
|
|
|
|
2 |
|
|
|
- |
|
|
|
- |
|
|
|
2 |
|
|
|
2 |
|
DB = Dutch Belted; Gr = group; HP = highly purified; IVT = intravitreal; NZW = New Zealand White; PBS = phosphate buffered saline; PK = pharmacokinetic; SD = single dose
Treatment A: 60 mg/mL of highly purified PAS-nomacopan (Batch XLMG260)
Treatment B: 20 mg/mL of highly purified PAS-nomacopan (Batch XLMG220)
Treatment C: Vehicle (PBS)
Treatment D: 20 mg/mL non-highly purified PAS-nomacopan (Batch P/20180327/1232/138)
a Study design table only includes animals destined for ocular histopathology analyses, and omits animals used for ocular PK assessments
b NZW animals (Groups 1-4) were males, DB animals (Groups 5-7) were females.
c Day 1 sacrifice occurred within 15 minutes of IVT dose administration.
The highly purified PAS-nomacopan formulations (Treatments A and B) had similar protein purity (>94% main peak by RP-HPLC) but were demonstrated to be essentially free of all pyrogens by MAT assay. Whereas pyrogens were detectable by MAT assay in Batch P/20180327/1232/138 (Treatment D).
Terminal timepoints were at 15 mins, and on Days 3, 7, 14 and 28. During the study, clinical observations, body weight, ophthalmic examinations (including slit lamp), electroretinogram (“ERG”) and intraocular pressure (“IOP”) were assessed, and histopathology was performed on all ocular tissues (both treated and untreated).
There were no differences in body weight changes between treatment groups and animals remained in good health with no test article-related clinical observations. There did not appear to be a treatment-related effect on IOP or ERG (A or B wave) and no significant changes from baseline were observed. In ophthalmic examinations, shining particles (likely cell infiltrate) were observed in most rabbits (including vehicle) after 2 to 6 days and remained visible until the end of the study (Day 28) in some rabbits. There did not appear to be a difference in the number of rabbits in the PBS (Treatment C), highly purified PAS-nomacopan 60 mg/mL (Treatment A) and highly purified PAS-nomacopan 20 mg/mL (Treatment B) groups exhibiting shining particles in the treated eyes only (14%, 7%, and 11% of rabbits respectively); however, in the non-highly purified PAS-nomacopan (Treatment D) group a greater proportion (relative to PBS and other groups) of rabbits (28%) exhibited shining particles in the treated eyes only.
There were histological observations in all groups including vehicle controls, but drug related-effects were only evident from Day 14 onwards with mild to severe ciliary body, choroid and iris cell infiltrates in NZW rabbits and similar mild to moderate drug related effects seen in DB rabbits.
At day 14, in NZW rabbits, 60 mg/mL highly purified PAS-nomacopan (Treatment A) and 20 mg/mL non-highly purified PAS-nomacopan (Treatment D) each induced 1 case of severe panuveitis, 20 mg/mL highly purified PAS-nomacopan (Treatment B) induced 1 case of moderate uveitis, and 20 mg/mL non-highly purified PAS-nomacopan (Treatment D) 1 case of moderate uveitis and 1 case of hyalitis. In DB rabbits DB, only 1 case of moderate uveitis was found which occurred with 20 mg/mL highly purified PAS-nomacopan (Treatment B).
At Day 28, in non-pigmented rabbits, 60 mg/mL highly purified PAS-nomacopan (Treatment A) and 20 mg/mL non-highly purified PAS-nomacopan (Treatment D) each induced 1 case of panuveitis and 1 case of less severe uveitis. In pigmented DB rabbits, 20 mg/mL highly purified PAS-nomacopan (Treatment B) induced 1 case of moderate uveitis. Moderate optic nerve inflammation was seen at Day 28 in one NZW rabbit treated with 60 mg/mL highly purified PAS-nomacopan (Treatment A). Dystrophic retina graded mild to moderate was observed in NZW rabbits but not in DB rabbits. Dystrophic retina commonly occurs spontaneously in NZW rabbits and was considered unrelated to drug treatment as the incidence of dystrophic retina was no different in PAS-nomacopan treated and vehicle treated NZW rabbits.
The data presented in the study suggest that IVT administration of PAS-nomacopan is associated with some changes indicative of ocular inflammation (cellular infiltrates to anterior eye) in some rabbits after a period of a couple of weeks. The PAS-nomacopan-related observations seem consistent with an immune response to the test item rather than direct toxicity of the test item or the presence of endotoxin. The time course of inflammation observed in this study was more consistent with an immune response which typically peaks 2 or more weeks after IVT injection rather than an innate response which typically peaks 2 to 3 days after IVT injection. It is not uncommon to observe ocular inflammation following administration of biologics to the eye in a nonclinical species such as rabbit. This species is known to generate robust immune and humoral responses to foreign proteins and peptides. All biotherapeutics that are currently approved for ocular use via IVT injection have shown immunogenicity during the ocular tolerability assessment in nonclinical species that manifest as signs of ocular inflammation and cell infiltration.
In addition to intravitreous single dose toxicology with highly purified PAS-nomacopan a non-GLP repeat dose acute systemic study was undertaken using early development batch PAS-nomacopan. Groups of 24 rats (Han Wistar), 12 male and 12 female in each group, received saline (Group 1) or PAS-nomacopan (Group 2 low dose and Group 3 high dose) once daily for 5-days by subcutaneous injection. The PAS-nomacopan stock (25.5mg/mL in PBS pH 7.4) used was pure (c.96% protein purity) but had a notably higher endotoxin value (0.56 endotoxin units [EU]/mg by limulus amebocyte lysate assay) than the PAS-nomacopan that is planned to be used for clinical intravitreous administration. The low dose group received 2mg/kg on day 1 and 1mg/kg/day on days 2 to 5, the high dose group received 60mg/kg on day 1 and 30mg/kg/day on days 2 to 5. Twelve rats from each group (1, 2 and 3) were sacrificed on day 5 and 12 rats from group 1 (saline) and group 3 (high dose) were sacrificed on day 10 after a 5-day recovery period. During the study clinical condition, body weight, food consumption, ophthalmoscopy, hematology (peripheral blood), blood chemistry, urinalysis, organ weights, macropathology and histopathology investigations were undertaken.
No animal died during treatment or recovery and no clinical or ophthalmic signs related to PAS-nomacopan treatment were seen. Body weight, food consumption, hematology and blood chemistry were unaffected throughout by drug treatment and recovery. There was also no effect on organ weights or volume and composition of urine. Macroscopic examination after 5 days of treatment revealed some dark areas at injection sites in some animals treated with PAS-nomacopan and one control male, after 5 days recovery there were no test item related lesions. Histopathological changes at injection sites related to both low and high dose PAS nomacopan were observed, with minimal to slight subcutaneous inflammatory cell infiltrate associated with a higher incidence of fibrosis at the earlier injection sites. Five days after cessation of treatment recovery at the injection sites was apparent.
PAS-nomacopan Inhibition of LTB4 Has Potential to Reduce the Risk of CNV
PAS-nomacopan’s ability to directly decrease CNV was evaluated in a mouse model of laser induced CNV. Seventy C57Bl/6J (pigmented) mice were randomised to one of 5 treatment groups of either single dose PAS-nomacopan, multi-dose PAS-nomacopan (both at 20mg/mL), single dose vehicle, multidose vehicle or multidose alflibercept (Eylea®). Immediately after laser induction mice received 3mL active or vehicle dosed IVT and the multi-dose groups also received IVT injections on days 3, 7 and 10 after laser induction. On Day 16 animals were sacrificed and CNV lesion volume measured by retinal flat mount histology and imaging of blood vessel marker using FITC-isolectin B4.
All animals from each group showed normal body weight evolution during the study and their general behavior and appearance were normal. A significant reduction of CNV lesion volume by single IVT PAS-nomacopan (p = 0.0222) compared to vehicle was observed and the reduction in lesion volume was equivalent to that seen with multiple dose IVT aflibercept (Table D).
Table D. PAS-nomacopan Significantly Decreases CNV in Classic Laser Induced Mouse Model

By contrast multiple dose PAS-nomacopan did not decrease CNV lesion volume compared to vehicle. The reason for this difference between single and multi-dose PAS-nomacopan is not clear, but the PAS-nomacopan used in this study was from an early batch produced by Wacker Biotech GmbH and contained a relatively high concentration of pyrogen (detectable by monocyte activation test) compared to the very low pyrogen present in the PAS-nomacopan drug substance that planned to be used for IND enabling GLP compliant toxicology studies and in the clinic.
In a further experiment PAS-nomacopan and PAS-L-nomacopan effect on retinal disease severity and on production of VEGF-A, which can induce CNV, was evaluated in a model of experimental allergic uveitis (“EAU”). PAS-L-nomacopan is a site directed mutant version of PAS-nomacopan that only inhibits LTB4 and not C5.
To induce EAU female C57Bl/6J mice were immunised with interphotoreceptor retinoid-binding protein (IRBP) IRBP1-20. The IRBP peptide induces autoreactive T-cells recognising retinal antigen mediated by Th17 and/or Th1 cells and disease is perpetuated by myeloid cells. At 14/15 days, when signs of disease appeared, mice were randomised to treatment and received intravitreous injections on days 15 and 18 of 1-2uL equimolar concentrations of active drug (nomacopan, PAS-nomacopan, PAS-L-nomacopan) or dexamethasone or saline. At Day 26 IVT PAS-nomacopan, PAS-L-nomacopan and dexamethasone all significantly ameliorated clinical score compared to saline whereas IVT nomacopan did not significantly reduce the score compared to saline at Day 26. The disease suppression identified by clinical score was confirmed by histopathology. Interestingly, in this EAU model PAS-L-nomacopan (LTB4 inhibition only) was at least as efficacious as PAS-nomacopan which inhibits both C5 and LTB4. This may be because PAS-nomacopan and PAS-L-nomacopan both exhibited equivalent significant suppression of the percentage of CD4+Th17+ cells and infiltrating macrophages present in retinal suspensions extracted from the eye at Day 21, and Th17 cells and activated macrophages are thought to be essential drivers of EAU. By contrast, equimolar nomacopan did not significantly reduce the percentage of CD4+Th17+ cells present in retinal suspensions at Day 21 compared to saline. Although drug concentration in eye were not measured it is possible that nomacopan had no significant effect on clinical score, CD4+Th17+ cells or infiltrating macrophages because the drug may have been rapidly cleared from the eye due to its small hydrodynamic radius. LTB4 injected into the vitreous of naïve B10RIII mice caused focal inflammatory lesions assessed by fundoscopy and recruited
immune cells including activated macrophages in the vitreoretinal space. Immunofluorescence staining on tissue sections from EAU eyes showed a significant increase, compared with healthy eyes, of one or both of LTB4 receptor BLT1 and the C5a receptor C5aR1 on infiltrating cells.
Akari tested PAS-L-nomacopan, which only binds LTB4 to determine if it a) ameliorates symptoms of EAU (clinical score) after induction of disease, and b) suppresses production of VEGF in this model as effectively as an anti-VEGF antibody, supporting the work of Sasaki et al., (2018) which provides mechanism for macrophage recruitment and polarization and VEGF induction by LTB4. The results shown in Figure F demonstrates that LTB4 has proinflammatory role within the eye in this model and in the same mice significantly decreases VEGF-A levels induced by EAU as effectively as an anti-VEGF-A monoclonal antibody. The data highlight the independent effects that inhibition of LTB4 by bispecific PAS nomacopan may have within the eye.
Figure F. PAS-L-Nomacopan (LTB4 Inhibition Only) Decreases Clinical Score and Decreases VEGF-A Levels as Effectively as Anti-VEGF-A Antibody in EAU

Suspended HSCT-TMA Clinical Program
HSCT-TMA is an orphan condition with severe cases having an estimated fatality rate of more than 80% patients with the disease. Complement activity is known to be implicated in HSCT-TMA with sC5b-9 (the soluble form of the membrane attack complex) and CH50 identified as key markers of disease progression; LTB4, which is also inhibited by nomacopan, may also be implicated by causing uncontrolled functioning of certain immune cells, such as neutrophils, that may lead to inflammation, tissue damage, and development of thrombosis. Currently, there are no approved treatment options for adult or pediatric patients with HSCT-TMA in the U.S. or Europe.
In addition, in February 2023, Akari announced it would add a new pipeline program to develop nomacopan as a potential treatment for adult HSCT-TMA, which will include a study that will serve as supportive evidence for the pediatric program.
In March 2023, Akari presented a case study of the first patient to complete treatment in the Part A portion of the Phase 3 clinical study of nomacopan in pediatric HSCT-TMA at the late-breaker at the Transplantation & Cellular Therapy Tandem Meetings and as a poster presentation at the European Society for Blood and Marrow Transplantation 49th Annual Meeting. A 6-year-old male patient at Royal Manchester Children’s Hospital, Manchester University NHS Foundation Trust in Manchester, UK received a 6/8 HLA-mismatched unrelated cord blood HSCT conditioned with fludarabine, treosulfan and thiotepa, for relapsed refractory acute myelogenous leukemia (“AML”). The patient received 7 granulocyte infusions peri-transplant as part of an experimental protocol to augment the graft-versus-leukemia effect. His immediate post-transplant course was complicated by engraftment syndrome, acute gut graft-versus-host disease (“GVHD”) grade 3 and cytomegalovirus (“CMV”) viraemia. At day +66 after transplant, the patient developed features consistent with TMA, was enrolled in the clinical trial, and began treatment with nomacopan on day +74. A single age- and weight-based ablating dose was followed by maintenance dosing for 21 days. After initial PD analysis at day 14 of treatment, the patient was found to have pre-dose terminal
complement activity (“TCA”) slightly higher (value 14.4) than the LLOQ (CH50 >10 U Eq/ml). Although his TCA had been reduced by 95% from a high baseline CH50 of 299.6U Eq/ml and sC5b9 had normalized, dose was increased in line with the study protocol. A few days later the patient developed neurological symptoms following a period of hypertension and was diagnosed with posterior reversible encephalopathy syndrome (“PRES”). Nomacopan was stopped for 3 days and restarted after the diagnosis was deemed to be unrelated to nomacopan treatment. Treatment continued for 46 days until the patient’s urine protein creatinine ratio was corrected for ≥28 days. Gut pathology and thrombocytopenia were resolved. The patient was discharged from the hospital and remains well and in remission. No adverse events related to nomacopan were experienced during the 72-day treatment period.
In May 2024, following Akari’s portfolio prioritization review, Akari’s HSCT-TMA program was suspended, with enrollment in its pediatric clinical study discontinued due to cost and timeline. Following closing of the Merger, Akari plans to work closely with the FDA to define the best path for this technology and will pursue opportunities for external partnering/collaboration, specifically as it relates to the potential eligibility for a priority review voucher in connection with future marketing applications for nomacopan, including as a treatment for pediatric HSCT-TMA.
Market Opportunity in Complement Mediated Diseases
The NIH estimates that approximately 23.5 million Americans may suffer from an autoimmune disorder, although this number is almost certainly an underestimate of the actual prevalence as it includes only 24 diseases for which good epidemiology studies were available. It is estimated that an additional 1.18 million people in the U.S. will acquire/develop an autoimmune disease every five years. Women are more than two times more likely than men to develop an autoimmune disease. Researchers have identified 80-100 different autoimmune diseases and suspect at least 40 additional diseases of having an autoimmune basis. Patients with one autoimmune disease are at increased risk of other diseases with an autoimmune basis. These diseases are chronic and can be life-threatening.
Autoimmune disease is one of the top 10 leading causes of death in female children and women in all age groups up to 64 years of age. The NIH estimates annual direct health care costs for autoimmune diseases to be in the range of $100 billion.
Both the complement and leukotriene pathways work as part of the immune system to disable and clear out foreign invaders and unwanted cells, and as such, plays an important role in the pathology of many autoimmune diseases. The term “Complement Mediated Diseases” applies to diseases and conditions where a patient’s immune system attacks and destroys healthy body tissue by mistake, causing direct damage mediated by complement and via a plethora of mediators induced by complement activation. In addition to those conditions where complement activity is believed to be the primary driver of disease, there are many other poorly treated diseases where in addition to complement activation other inflammatory pathways are implicated. These diseases, such as GA, HSCT-TMA, PNH, aHUS, GBS, Myasthenia Gravis, NMOSD, BP and AKC, are potential targets for bi-specific nomacopan.
Akari believes over 5 million GA patients worldwide are estimated to be affected, with approximately 1 to 1.6 million in the U.S. alone.
Competition in Complement and Leukotriene Mediated Diseases
The development and commercialization of new drugs is highly competitive. Akari expects to face competition with respect to all product candidates that Akari may develop or commercialize in the future from pharmaceutical and biotechnology companies worldwide. The key factors affecting the success of any approved product will be its efficacy, safety profile, drug interactions, method of administration, pricing, reimbursement and level of promotional activity relative to those of competing drugs.
Akari’s potential competitors may have substantially greater financial, technical, and personnel resources than Akari. In addition, many of these competitors have significantly greater commercial infrastructures. Akari’s ability
to compete successfully will depend largely on Akari’s ability to leverage Akari’s collective experience in drug discovery, development and commercialization to:
•discover and develop drugs that are differentiated from other products in the market;
•obtain patent and/or proprietary protection for Akari’s product candidates and technologies;
•obtain required marketing authorizations;
•commercialize Akari’s product candidates ourselves and/or through partners, if approved; and
•attract and retain high-quality personnel, including those with research, development and commercial skills.
There has been a broad research effort in complement-based therapy to date, with eculizumab being the first therapy approved that directly inhibits C5. Although there is currently less research and development effort in the leukotriene field there are approved leukotriene inhibitors used as a treatment for severe asthma. However, Akari is aware of certain other companies and academic institutions that are continuing their efforts to discover and develop alternate complement and/or C5 inhibitors, including, but not limited to, Alexion Pharmaceuticals, a subsidiary of AstraZeneca, Annexon, Inc., Apellis Pharmaceuticals, Inc., Omeros Corporation, Amgen, Inc., IVERIC bio, Inc., Novartis AG, Roche Pharmaceuticals, and UCB, Inc.
Sales and Marketing
Because Akari has been focused on discovery and development of drugs, Akari currently has limited sales, marketing and distribution capabilities in order to commercialize PAS-nomacopan or any other product candidates that may be approved in the future. If PAS-nomacopan or other product candidates Akari may pursue in the future are approved, Akari intends either to establish a sales and marketing organization with technical expertise and supporting distribution capabilities to commercialize such products, or to outsource some or all of these functions to third parties. Akari may take different approaches to commercialization in different geographies. Akari will adopt a similar strategy for the other compounds in Akari’s pipeline.
Manufacturing
Akari currently employs third-party contract development and manufacturing organizations (“CDMOs”), which manufacture in accordance with cGMP requirements, for Akari’s investigational medical products, including active pharmaceutical ingredients, drug substance and drug product for Akari’s currently ongoing preclinical and anticipated clinical research studies for PAS-nomacopan.
Since 2017, Akari has engaged a CDMO, Wacker Biotech GmbH, to develop a manufacturing process for PAS-nomacopan. Two development batches of drug substance and a development batch of drug product were successfully manufactured in 2023. A full-scale batch of GMP drug substance was released in April 2024. The GMP material will be used for all final IND enabling preclinical studies and for drug product manufacture for the planned clinical studies.
Akari does not own or operate, and currently have no plans to establish, any manufacturing facilities. Akari expects to rely on CDMOs for the manufacture of PAS-nomacopan and any other product candidates that Akari may develop, as well as for commercial quantities of any product candidates that are approved.
In the future Akari may encounter disruptions in the supply chain of PAS-nomacopan which could negatively impact Akari’s ability to procure the components for each of Akari’s product candidates for use in preclinical studies and clinical trials and enrolling patients in clinical trials.
Intellectual Property
Akari will be able to protect Akari’s technology and products from unauthorized use by third parties only to the extent it is covered by valid and enforceable patents or is effectively maintained as trade secrets. Patents and other proprietary rights are thus an essential element of Akari’s business.
Akari’s success will depend in part on Akari’s ability to obtain and maintain proprietary protection for Akari’s product candidates, technology, and know-how, to operate without infringing on the proprietary rights of others, and to prevent others from infringing Akari’s proprietary rights. Akari’s policy is to seek to protect Akari’s proprietary position by, among other methods, filing U.S. and foreign patent applications related to Akari’s proprietary technology, inventions, and improvements that are important to the development of Akari’s business and defending Akari’s patent applications and patents if they are subjected to challenge by a third party. Akari also relies on trade secrets, know-how, continuing technological innovation, and in-licensing opportunities to develop and maintain Akari’s proprietary position.
As of September 11, 2024, Akari own or have exclusive rights to patents and patent applications based on 9 international patent applications. This includes five issued United States patents, five patents granted by the European Patent Office and foreign issued patents in other jurisdictions. This further includes pending patent applications in the United States and other jurisdictions. Akari’s patents and patent applications relate to the uses of complement C5 inhibitor protein nomacopan and PAS-nomacopan in the treatment of key disease indications, as well as to nomacopan variants, and uses of histamine binding proteins. As of September 11, 2024, Akari’s current patent portfolio includes granted patents in the jurisdictions of United States, Canada, major European countries, Japan, China, Israel, Republic of Korea, Australia, and pending applications in the jurisdictions of United States, Canada, Europe, Japan, China, Israel, Republic of Korea, Australia and New Zealand.
Issued patents in the US and other countries which cover uses of Akari’s product candidates nomacopan and/or PAS-nomacopan will expire between 2026 and 2038, excluding any patent term adjustment that might be available in certain countries, or any patent term extensions that might be available following the grant of marketing authorizations. Akari has pending patent applications for uses of Akari’s product candidates nomacopan and/or PAS-nomacopan that, if issued, would expire in the United States and in countries outside of the United States between 2031 and 2040, excluding any patent term adjustment that might be available following the grant of the patent and any patent term extensions that might be available following the grant of marketing authorizations. These patent and patent applications relate to subject matters including: methods for treating myasthenia gravis; methods for treating viral infections of the respiratory tract; methods of treating complement-mediated diseases in patients with C5 polymorphisms, methods of treating autoimmune blistering diseases; methods of treating rheumatic diseases; methods of treating proliferative retinal diseases; and nomacopan variants lacking C5 binding.
Akari has licensed rights to patents and patent applications relating to PAS polypeptides and nucleic acids encoding PAS polypeptides, which include patents/applications which cover PAS-nomacopan fusion proteins.
If Akari is unable to obtain, maintain, defend and enforce patent and other intellectual property rights for Akari’s technologies and product candidates nomacopan and/or PAS-nomacopan, or if the scope of the patent and other intellectual property rights obtained is not sufficiently broad, Akari’s competitors and other third parties could develop and commercialize technology, biologics and/or biosimilars similar or identical to Akari’s, and erode or negate any competitive advantage that Akari may have, which could harm Akari’s business and ability to achieve profitability.
Akari can provide no assurance that Akari’s patent applications or those of Akari’s licensors will result in additional patents being issued or that issued patents will afford sufficient protection against competitors with similar technologies, nor can there be any assurance that the patents issued will not be infringed, designed around or invalidated by third parties. Even issued patents may later be found unenforceable or may be modified or revoked in proceedings instituted by third parties before various patent offices or in courts. The degree of future protection for Akari’s proprietary rights is uncertain. Only limited protection may be available and may not adequately protect Akari’s rights or permit us to gain or keep competitive advantage. Composition-of-matter patents on the biological or chemical active pharmaceutical ingredients are generally considered to offer the strongest protection of intellectual property and provide the broadest scope of patent protection for pharmaceutical products, as such patents provide protection without regard to any method of use or any method of manufacturing. While Akari has issued composition-of-matter patents in the United States and other countries, Akari cannot be certain that the claims in Akari’s issued composition-of-matter patents will not be found invalid or unenforceable if challenged. Akari cannot be certain that the claims in any patent applications covering composition-of-matter or formulations that are pending, or that Akari may file, will be considered patentable by the USPTO, and courts in the United States or by the patent offices and courts in foreign countries, nor can Akari be certain that the claims in Akari’s issued
composition-of-matter patents will not be found invalid or unenforceable if challenged. Even if any patent applications that Akari may file relating to specific formulations of Akari’s product candidates issue as patents, formulation patents protect a specific formulation of a product and may not be enforced against competitors making and marketing a product that has the same active pharmaceutical ingredient in a different formulation. Method-of-use patents protect the use of a product for the specified method or for treatment of a particular indication. This type of patent may not be enforced against competitors making and marketing a product that has the same active pharmaceutical ingredient for use in a method not claimed by the patent. Moreover, even if competitors do not actively promote their product for Akari’s targeted indications, physicians may prescribe these products “off-label.” Although off-label prescriptions may infringe or contribute to the infringement of method-of-use patents, the practice is common and such infringement may be difficult to prevent or prosecute. Akari cannot be certain that the claims in Akari’s issued method-of-use patents will not be found invalid or unenforceable if challenged. Akari cannot be certain that the claims in any patent applications covering methods of using Akari’s product candidates that are pending, or that Akari may file, will be considered patentable by the USPTO and courts in the United States or by the patent offices and courts in foreign countries, nor can Akari be certain that the claims in Akari’s issued method-of-use patents will not be found invalid or unenforceable if challenged.
Government Regulation
Government Regulation and Product Approval
Government authorities in the U.S., at the federal, state and local level, and in other countries extensively regulate, among other things, the research, development, testing, manufacture, quality control, approval, labeling, packaging, storage, record-keeping, promotion, advertising, distribution, marketing and export and import of products such as those that Akari are developing. A new drug must be approved by the FDA, generally through the NDA process and a new biologic must be approved by the FDA through the BLA process before it may be legally marketed in the U.S. The animal and other non-clinical data and the results of human clinical trials performed under an IND and under similar foreign applications will become part of the NDA or BLA.
U.S. Drug Development Process
In the U.S., the FDA regulates drugs under the Federal Food, Drug, and Cosmetic Act (“FDCA”) and in the case of biologics, also under the Public Health Service Act (“PHSA”) and the implementing regulations for both statutes. The process of obtaining marketing authorizations and the subsequent compliance with applicable federal, state, local, and foreign statutes and regulations require the expenditure of substantial time and financial resources. Failure to comply with the applicable U.S. requirements at any time during the product development process, approval process or after approval, may subject an applicant to administrative or judicial sanctions. These sanctions could include the FDA’s refusal to approve pending applications, withdrawal of an approval, a clinical hold, warning letters, requesting product recalls, product seizures, total or partial suspension of production or distribution, injunctions, fines, refusals of government contracts, restitution, disgorgement, or civil or criminal penalties. Any agency or judicial enforcement action could have a material adverse effect on Akari.
The process required by the FDA before a drug or biologic may be marketed in the U.S. generally involves the following:
•completion of preclinical laboratory tests, animal studies and formulation studies according to GLP and relevant provisions of the Animal Welfare Act, where applicable, or other applicable laws and regulations;
•submission to the FDA of an IND which must become effective before human clinical trials may begin;
•performance of adequate and well-controlled human clinical trials according to Good Clinical Practices (“GCP”) to establish the safety and efficacy of the proposed drug for its intended use;
•submission to the FDA of an NDA or BLA;
•satisfactory completion of an FDA inspection of the manufacturing facility or facilities at which the drug is produced to assess compliance with cGMP to assure that the facilities, methods and controls are adequate to preserve the drug’s identity, strength, quality and purity; and
•FDA review and approval of the NDA or BLA.
Once a product candidate is identified for development, it enters the preclinical testing stage. Preclinical tests include laboratory evaluations of product chemistry, toxicity and formulation, as well as animal studies. An IND sponsor must submit the results of the preclinical tests, together with manufacturing information and analytical data, to the FDA as part of the IND. The sponsor will also include a protocol detailing, among other things, the objectives of the first phase of the clinical trials, the parameters to be used in monitoring safety, and the effectiveness criteria to be evaluated, if the first phase lends itself to an efficacy evaluation. Some preclinical testing may continue even after the IND is submitted. The IND automatically becomes effective 30 days after receipt by the FDA, unless the FDA, within the 30-day time period, places the clinical trial on a clinical hold. In such a case, the IND sponsor and the FDA must resolve any outstanding concerns before the clinical trial can begin. Clinical holds also may be imposed by the FDA at any time before or during studies due to safety concerns or non-compliance.
All clinical trials must be conducted under the supervision of one or more qualified investigators in accordance with GCP. They must be conducted under protocols detailing the objectives of the trial, dosing procedures, subject selection and exclusion criteria and the safety and effectiveness criteria to be evaluated. Each protocol must be submitted to the FDA as part of the IND, and progress reports detailing the results of the clinical trials must be submitted at least annually. In addition, timely safety reports must be submitted to the FDA and the investigators for serious and unexpected adverse events. An IRB responsible for the research conducted at each institution participating in the clinical trial must review and approve each protocol before a clinical trial commences at that institution and must also approve the information regarding the trial and the consent form that must be provided to each trial subject or his or her legal representative, monitor the study until completed and otherwise comply with IRB regulations.
Human clinical trials are typically conducted in three sequential phases that may overlap or be combined:
•Phase 1: The product candidate is initially introduced into healthy human subjects and tested for safety, dosage tolerance, absorption, metabolism, distribution and excretion. In the case of some products for severe or life-threatening diseases, such as cancer, especially when the product may be too inherently toxic to ethically administer to healthy volunteers, the initial human testing may be conducted in patients.
•Phase 2: This phase involves studies in a limited patient population to identify possible adverse effects and safety risks, to preliminarily evaluate the efficacy of the product for specific targeted diseases and to determine dosage tolerance and optimal dosage.
•Phase 3: Clinical trials are undertaken to further evaluate dosage, clinical efficacy and safety in an expanded patient population at geographically dispersed clinical study sites. These studies are intended to establish the overall risk-benefit ratio of the product candidate and provide, if appropriate, an adequate basis for product labeling.
The FDA or the sponsor may suspend a clinical trial at any time on various grounds, including a finding that the research subjects or patients are being exposed to an unacceptable health risk. Similarly, an IRB can suspend or terminate approval of a clinical trial at its institution if the clinical trial is not being conducted in accordance with the IRB’s requirements or if the drug has been associated with unexpected serious harm to patients. Phase 1, Phase 2, and Phase 3 testing may not be completed successfully within any specified period, if at all.
During the development of a new drug, sponsors are given opportunities to meet with the FDA at certain points. These points may include prior to submission of an IND, at the end of Phase 2, and before an NDA or BLA is submitted. Meetings at other times may be requested. These meetings can provide an opportunity for the sponsor to share information about the data gathered to date, for the FDA to provide advice, and for the sponsor and FDA to reach agreement on the next phase of development. Sponsors typically use the end of Phase 2 meeting to discuss their Phase 2 clinical results and seek feedback on their plans for the pivotal Phase 3 clinical trial that they believe will support approval of the new drug.
Progress reports detailing the results of the clinical trials must be submitted at least annually to the FDA. Safety reports must be submitted to the FDA and the investigators 15 calendar days after the trial sponsor determines that the adverse event information qualifies for reporting. The sponsor also must notify FDA of any unexpected fatal or life-threatening suspected adverse reaction as soon as possible but in no case later than 7 calendar days after the sponsor’s initial receipt of the information. Sponsors of clinical trials of drugs and biologics are required to register and disclose certain clinical trial information on a registry maintained by the National Institutes of Health, at www.clinicaltrials.gov.
Concurrent with clinical trials, companies usually complete additional animal studies and must also develop additional information about the chemistry and physical characteristics of the drug and finalize a process for manufacturing the product in commercial quantities in accordance with cGMP requirements. The manufacturing process must be capable of consistently producing quality batches of the product candidate and, among other things, the manufacturer must develop methods for testing the identity, strength, quality and purity of the final drug. Additionally, appropriate packaging must be selected and tested and stability studies must be conducted to demonstrate that the product candidate does not undergo unacceptable deterioration over its shelf life.
U.S. Review and Approval Processes
The results of product development, preclinical studies and clinical trials, along with descriptions of the manufacturing process, analytical tests conducted on the chemistry of the drug, proposed labeling, and other relevant information are submitted to the FDA as part of an NDA or BLA requesting approval to market the product. The submission of an NDA or BLA is subject to the payment of substantial user fees; a waiver of such fees may be obtained under certain limited circumstances. Within sixty days of receipt, the FDA initially reviews all NDAs and BLAs submitted to ensure that they are sufficiently complete for substantive review before it accepts them for filing. The FDA may request additional information rather than accept a NDA or BLA for filing. In this event, the NDA or BLA must be resubmitted with the additional information. The resubmitted application also is subject to review before the FDA accepts it for filing. Once the submission is accepted for filing, the FDA begins an in-depth substantive review. FDA may refer an NDA or BLA that is novel or that presents difficult questions of safety or efficacy to an advisory committee for review, evaluation and recommendation on questions presented by the FDA, which may include questions related to whether the application should be approved and under what conditions. The FDA is not bound by the recommendation of an advisory committee, but it generally follows such recommendations. Before approving an NDA or BLA, the FDA will typically inspect one or more clinical sites to assure compliance with GCP. Additionally, the FDA will inspect the facility or the facilities at which the product is manufactured to assess compliance with cGMP.
The FDA may also place other conditions on approval, including the requirement for a Risk Evaluation and Mitigation Strategy (“REMS”) to assure the safe use of the product. If the FDA concludes a REMS is needed, the sponsor of the NDA or BLA must submit a proposed REMS, and the FDA will not approve the application without an approved REMS. A REMS could include medication guides, physician communication plans or elements to assure safe use, such as restricted distribution methods, patient registries and other risk minimization tools. Any of these limitations on approval or marketing could restrict the commercial promotion, distribution, prescription or dispensing of products.
The approval process is lengthy and often difficult, and the FDA may refuse to approve an NDA or BLA if the applicable regulatory criteria are not satisfied or may require additional clinical or other data and information. Even if such data and information are submitted, the FDA may ultimately decide that the NDA or BLA does not satisfy the criteria for approval. Data obtained from clinical trials are not always conclusive and the FDA may interpret data differently than how Akari interprets the same data. The FDA reviews an NDA to determine, among other things, whether a product is safe and effective for its intended use and whether its manufacturing is cGMP-compliant to assure and preserve the product’s identity, strength, quality and purity. The FDA reviews a BLA to determine, among other things whether the product is safe, pure and potent and the facility in which it is manufactured, processed, packed or held meets standards designed to assure the product’s continued safety, purity and potency. The FDA may issue a complete response letter (“CRL”), which may require additional clinical or other data or impose other conditions that must be met in order to secure final approval of the NDA or BLA, or an approval letter following satisfactory completion of all aspects of the review process. The applicant may either resubmit the NDA or BLA, addressing all of the deficiencies identified in the letter, withdraw the application, or, in the case of an
NDA, request an opportunity for a hearing. The applicant also may request resolution of any dispute concerning the CRL. If the FDA denies approval of a BLA, the applicant may request, and FDA must issue, a notice of opportunity for hearing.
NDAs or BLAs may receive either standard or priority review. Under current FDA review goals, standard review of an NDA for a new molecular entity (“NME”) or original BLA will be ten months from the date that the NDA or BLA is filed. A drug representing a significant improvement in treatment, prevention or diagnosis of a serious disease or condition may receive a priority review of six months. Priority review does not change the standards for approval, but may expedite the approval process.
If a product receives marketing authorization, the approval may be significantly limited to specific diseases and dosages or the indications for use may otherwise be limited, which could restrict the commercial value of the product. In addition, the FDA may require a sponsor to conduct Phase IV testing, such as clinical trials designed to further assess a drug’s safety and/or effectiveness after NDA or BLA approval, and may require testing and surveillance programs to monitor the safety of approved products which have been commercialized.
The Pediatric Research Equity Act (“PREA”) requires a sponsor to conduct pediatric studies for most drugs and biologics with a new active ingredient, new indication, new dosage form, new dosing regimen or new route of administration. Under PREA, original NDAs and BLAs and certain supplemental applications must contain a pediatric assessment unless the sponsor has received a deferral or waiver. The required assessment must assess the safety and effectiveness of the product for the claimed indications in all relevant pediatric subpopulations and support dosing and administration for each pediatric subpopulation for which the product is safe and effective. The sponsor or FDA may request a deferral of pediatric studies for some or all of the pediatric subpopulations. A deferral may be granted for several reasons, including a finding that the drug or biologic is ready for approval for use in adults before pediatric studies are complete or that additional safety or effectiveness data needs to be collected before pediatric studies can begin.
The Best Pharmaceuticals for Children Act provides NDA holders a six-month period of exclusivity attached to any patent or regulatory exclusivity listed in the Orange Book, and BLA holders a six-month period of exclusivity attached to any unexpired regulatory exclusivity, if certain conditions are met. Conditions for pediatric exclusivity include a determination by the FDA that information relating to the use of a new drug in the pediatric population may produce health benefits in that population, a written request by the FDA for pediatric studies, completion of the studies in accordance with the written request, and submission of reports from the requested studies to the FDA. The issuance of a written request does not require the sponsor to undertake the described studies.
Patent Term Restoration and Marketing Exclusivity
Depending upon the timing, duration and specifics of FDA approval of Akari’s product candidates, some of Akari’s U.S. patents may be eligible for limited patent term extension under the Drug Price Competition and Patent Term Restoration Act of 1984, referred to as the Hatch-Waxman Amendments. The Hatch-Waxman Amendments permit a patent restoration term of up to five years as partial compensation for effective patent term lost due to time spent during product development and the FDA regulatory review process. However, patent term restoration cannot extend the remaining term of a patent beyond a total of 14 years from the product’s approval date. The patent term restoration period is generally one-half the time between the effective date of an IND, and the submission date of an NDA or BLA, plus the time between the submission date of an NDA or BLA and the approval of that application, except that the period is reduced by any time during which the applicant failed to exercise due diligence. Only one patent applicable to an approved drug may be extended, and the extension must be applied for prior to expiration of the patent. The United States Patent and Trademark Office, in consultation with the FDA, reviews and approves the application for any patent term extension or restoration.
Biologics Price Competition and Innovation Act of 2009 (BPCIA)
The BPCIA amended the PHSA to create an abbreviated approval pathway for biosimilar and interchangeable biosimilar products and provide for a twelve-year exclusivity period for the first approved biological product, or reference product, against which a biosimilar or interchangeable biosimilar application is evaluated. A biosimilar product is defined as one that is highly similar to a reference product notwithstanding minor differences in clinically
inactive components and for which there are no clinically meaningful differences between the biological product and the reference product in terms of the safety, purity and potency of the product. An interchangeable biosimilar product is a biosimilar product that, subject to state pharmacy laws, may be substituted for the reference product without the intervention of the health care provider who prescribed the reference product.
The biosimilar applicant must demonstrate that the product is biosimilar based on data from: (1) analytical studies showing that the biosimilar product is highly similar to the reference product; (2) animal studies (including toxicity); and (3) as applicable, one or more clinical studies to demonstrate safety, purity and potency in one or more appropriate conditions of use for which the reference product is approved. In addition, the applicant must show that the biosimilar and reference products have the same mechanism of action for the conditions of use on the label, route of administration, dosage and strength, and the production facility must meet standards designed to assure product safety, purity and potency.
An application for a biosimilar product may not be submitted until four years after the date on which the reference product was first approved. The first approved interchangeable biosimilar product will be granted an exclusivity period of up to one year after it is first commercially marketed, but the exclusivity period may be shortened under certain circumstances.
Orphan Drug Designation
Under the Orphan Drug Act, the FDA may grant orphan drug designation to a drug intended to treat a rare disease or condition, which is generally a disease or condition that affects fewer than 200,000 individuals in the U.S., or more than 200,000 individuals in the U.S. and for which there is no reasonable expectation that the cost of developing and making available in the U.S. a drug for this type of disease or condition will be recovered from sales in the U.S. for that drug. Orphan drug designation must be requested before submitting an NDA or BLA. After the FDA grants orphan drug designation, the identity of the therapeutic agent and its potential orphan use are disclosed publicly by the FDA. Orphan drug designation does not itself convey any advantage in or shorten the duration of the regulatory review and approval process. If a product that has orphan drug designation subsequently receives the first FDA approval for the disease for which it has such designation, the product is entitled to orphan product exclusivity, which means that the FDA may not approve any other applications to market the same drug for the same indication, except in very limited circumstances, for seven years. Orphan drug exclusivity, however, also could block the approval of one of Akari’s product candidates for seven years if a competitor obtains approval of the same drug, for the same designated orphan indication or if Akari’s product candidate is determined to be contained within the competitor’s product for the same indication or disease.
Rare Pediatric Disease Priority Review Vouchers
With enactment of the Food and Drug Administration Safety and Innovation Act of 2012 (“FDASIA”), Congress authorized the FDA under Section 529 of the FDCA to award PRVs, to sponsors of certain rare pediatric disease product applications. This provision, which was further amended by the Advancing Hope Act of 2016, is designed to encourage development of new drug and biological products for prevention and treatment of certain rare pediatric diseases.
Under this program, a sponsor who receives approval for a new drug or biologic for a rare pediatric disease may qualify for a PRV, which can be redeemed for priority review of a subsequent marketing application for a different product. The sponsor of a rare pediatric disease drug product that receives a PRV may transfer, including by sale, the PRV to another sponsor and that PRV may be further transferred any number of times before it is used. A PRV entitles the holder to designate a single human drug application submitted under Section 505(b)(1) of the FDCA or Section 351 of the PHSA as qualifying for a priority review. An FDA priority review may expedite the review process of a marketing application reducing the review time from ten months after formal acceptance of the file to six months after formal acceptance of the file.
In order for a sponsor to receive a PRV in connection with approval of a BLA or NDA, the investigational product must be designated by the FDA as a product for a rare pediatric disease prior to submission of the marketing application. A rare pediatric disease is a disease that is serious or life-threatening and which primarily affects individuals aged from birth to 18 years and fewer than 200,000 people in the United States. Alternatively, the
disease may affect more than 200,000 people in the United States if there is no reasonable expectation that the cost of developing and making available in the United States a product for such disease or condition will be recovered from sales in the United States of such product. In addition, to qualify for a PRV, the sponsor must request the voucher and the BLA or NDA must itself be given priority review, rely on clinical data derived from studies examining a pediatric population and dosages of the product intended for that population, not seek approval for a different adult indication in the original rare pediatric disease product application and be for a product that does not include a previously approved active ingredient.
The Rare Pediatric Disease PRV program was originally set to expire in October 2020 but was extended for an additional six years with passage of the Coronavirus Response and Relief Supplemental Consolidated Appropriations Act of 2021. Under the current statutory sunset provisions, the FDA may only award a rare pediatric disease PRV if a sponsor has a rare pediatric disease designation for the drug or biologic before September 30, 2024, and the NDA or BLA for the product is approved before September 30, 2026.
Fast Track Designation and Accelerated Approval
The FDA has established programs to facilitate the development, and expedite the review of, drugs that are intended for the treatment of a serious or life-threatening disease or condition for which there is no effective treatment and which demonstrate the potential to address unmet medical needs for the condition. Under the fast track program, the sponsor of a product candidate may request that the FDA designate the product candidate for a specific indication as a fast track drug concurrent with, or after, the filing of the IND for the product candidate. The FDA determines if the product candidate qualifies for fast track designation within 60 days of receipt of the sponsor’s request.
The FDA may designate a drug for fast-track status if it is intended to treat a serious or life-threatening illness and nonclinical or clinical data demonstrate the potential to address an unmet medical need. If so designated, the FDA takes steps to expedite the development and review of the product’s marketing application, including by meeting with the sponsor more frequently to provide timely advice so that the development program is as efficient as possible. Another benefit of fast-track designation is that the FDA may initiate review of sections of an NDA or BLA before the application is complete. This rolling review is available if the applicant provides, and the FDA approves, a schedule for the submission of the remaining information and the applicant pays applicable user fees. The FDA’s review goal date does not begin until the last section of the application is submitted, however. Fast track designation may be withdrawn by the FDA if the FDA believes that the designation is no longer supported by data emerging in clinical trials.
The agency may determine that an accelerated approval pathway is appropriate if a product candidate is intended to treat a serious condition and provide meaningful therapeutic benefit to patients over existing treatments based upon a surrogate endpoint that is reasonably likely to predict clinical benefit, or on a clinical endpoint that can be measured earlier than irreversible morbidity or mortality, that is reasonably likely to predict an effect on irreversible morbidity or mortality or other clinical benefit, taking into account the severity, rarity, or prevalence of the condition and the availability or lack of alternative treatments.
In clinical trials, a surrogate endpoint is a measurement of laboratory or clinical signs of a disease or condition that substitutes for a direct measurement of how a patient feels, functions, or survives. Surrogate endpoints can often be measured more easily or more rapidly than other clinical endpoints. As a condition of accelerated approval, the FDA generally requires that the sponsor perform adequate and well-controlled post-marketing clinical trials with due diligence to confirm clinical benefit and, under the Food and Drug Omnibus Reform Act of 2022, the FDA is now permitted to require, as appropriate, that such trials be underway prior to approval or within a specific time period after the date accelerated approval is granted. Failure to conduct required post-approval studies or to confirm clinical benefit through post-marketing studies allows the FDA to withdraw the drug from the market on an expedited basis. In addition, for products under accelerated approval, FDA generally requires all promotional materials, including launch materials, to be submitted for prior review.
Post-Approval Requirements
Once approval of an NDA or BLA is granted, the FDA may withdraw the approval if compliance with regulatory standards is not maintained or if problems are identified after the product reaches the market. Newly discovered or developed safety or effectiveness data may require changes to a product’s approved labeling, including the addition of new warnings and contraindications, and also may require the implementation of other risk management measures, including a REMS or the conduct of post-marketing studies to assess a newly discovered safety issue. Later discovery of previously unknown problems with a product may result in restrictions on the product or even complete withdrawal of the product from the market. After approval, some types of changes to the approved product, such as adding new indications, manufacturing changes and additional labeling claims, are subject to further FDA review and approval. Drug manufacturers and other entities involved in the manufacture and distribution of approved drugs are required to register their establishments with the FDA and certain state agencies, and are subject to periodic unannounced inspections by the FDA and certain state agencies for compliance with cGMP and other laws and regulations. Akari relies, and expect to continue to rely, on third parties for the production of clinical and commercial quantities of Akari’s products. Future inspections by the FDA and other regulatory agencies may identify compliance issues at the facilities of Akari’s contract manufacturers that may disrupt production or distribution, or require substantial resources to correct.
Any drug products manufactured or distributed by Akari pursuant to FDA approvals are subject to continuing regulation by the FDA, including, among other things, requirements related to record-keeping, reporting of adverse experiences, submitting periodic reports, updating safety and efficacy information, drug sampling and distribution, and electronic records and signatures. The FDA also closely regulates labeling, advertising, promotion and other types of information that may be disseminated about products that are placed on the market. Drugs may be promoted only for the approved indications and in a manner that is consistent with the approved label.
From time to time, legislation is drafted, introduced and passed in Congress that could significantly change the statutory provisions governing the development, approval, manufacturing and marketing of products regulated by the FDA. It is impossible to predict whether further legislative changes will be enacted, or FDA regulations, guidance or interpretations changed or what the impact of such changes, if any, may be.
Regulation and Marketing Authorization in the European Union
Preclinical Studies
Preclinical tests include laboratory evaluations of product chemistry, formulation and stability, as well as studies to evaluate toxicity in animal studies, in order to assess the potential safety and efficacy of the product. The conduct of the preclinical tests and formulation of the compounds for testing must comply with the relevant EU regulations and requirements. The results of the preclinical tests, together with relevant manufacturing information and analytical data, are submitted as part of the CTA and MAA.
Clinical Trial Approval
Clinical trials in the EU are governed by the Clinical Trials Regulation, (EU) No 536/2014, or the CT Regulation. The CT Regulation was adopted in 2014 and replaces the Clinical Trials Directive 2001/20/EC, or the CT Directive. To ensure that the rules for clinical trials are identical throughout the EU, the EU clinical trials legislation was passed as a “regulation” that is directly applicable in all EU Member States. All clinical trials performed in the EU are required to be conducted in accordance with the CT Regulation.
The CT Regulation aims to harmonize, simplify and streamline the approval of clinical trials in the EU. The main characteristics of the CT Regulation include:
•A streamlined application procedure via a single-entry point, the EU portal.
•A single set of documents to be prepared and submitted for the application as well as simplified reporting procedures that will spare sponsors from submitting broadly identical information separately to various bodies and different EU Member States.
•A harmonized procedure for the assessment of applications for clinical trials, which is divided in two parts. Part I is assessed jointly by all Member States Concerned. Part II is assessed separately by each Member State Concerned.
•Strictly defined deadlines for the assessment of clinical trial application.
•The involvement of the ethics committees in the assessment procedure in accordance with the national law of the Member State Concerned but within the overall timelines defined by the CT Regulation.
The transitory provisions of the CT Regulation provide that ongoing clinical trials previously authorized under the CT Directive, can remain under the CT Directive, or they can transition to the CTR. By January 31, 2025, all ongoing clinical trials must have transitioned to the CTR.
Marketing Authorization
Authorization to market a product in the Member States of the EU proceeds under one of four procedures: a centralized authorization procedure, a mutual recognition procedure, a decentralized procedure or a national procedure.
Centralized Authorization Procedure
The centralized procedure enables applicants to obtain a marketing authorization that is valid in all EU Member States based on a single application. Certain medicinal products, including products developed by means of biotechnological processes, must undergo the centralized authorization procedure to obtain marketing authorization, which, if granted by the European Commission, is automatically valid in all 27 EU Member States.
The centralized authorization procedure is mandatory for:
•medicinal products developed by means of biotechnological processes such as genetic engineering;
•advanced therapy medicinal products as defined in Article 2 of Regulation (EC) No. 1394/2007 on advanced therapy medicinal products (such as, gene-therapy, somatic cell-therapy or tissue-engineered medicines);
•human immunodeficiency virus;
•acquired immune deficiency syndrome;
•neurodegenerative disorder;
•auto-immune diseases and other immune dysfunctions;
•medicinal products that are designated as orphan medicinal products pursuant to Regulation (EC) No 141/2000.
The centralized authorization procedure is optional for other medicinal products if they contain a new active substance or if the applicant shows that the medicinal product concerned constitutes a significant therapeutic, scientific or technical innovation or that the granting of authorization is in the interest of patients in the EU.
Administrative Procedure
Under the centralized authorization procedure, the EMA’s Committee for Medicinal Products for Human Use (“CHMP”) serves as the scientific committee that renders opinions about the safety, efficacy and quality of medicinal products for human use on behalf of the EMA. The CHMP has 210 days to adopt an opinion as to whether
a marketing authorization should be granted. The process usually takes longer in case additional information is requested, which triggers clock-stops in the procedural timelines. The process is complex and involves extensive consultation with the regulatory authorities of EU Member States and a number of experts. When an application is submitted for a marketing authorization in respect of a product that is of major interest from the point of view of public health and in particular from the viewpoint of therapeutic innovation, the applicant may pursuant to Article 14(9) Regulation (EC) No 726/2004 request an accelerated assessment procedure. If the CHMP accepts such request, the time-limit of 210 days will be reduced to 150 days but it is possible that the CHMP can revert to the standard time limit for the centralized procedure if it considers that it is no longer appropriate to conduct an accelerated assessment. If the opinion is negative, information is given as to the grounds on which this conclusion was reached. After the adoption of the CHMP opinion, a decision on the MAA must be adopted by the European Commission, after consulting the EU Member States, which in total can take more than 60 days.
Conditional Approval
In specific circumstances, EU legislation (Article 14(7) Regulation (EC) No 726/2004 and Regulation (EC) No 507/2006 on Conditional Marketing Authorizations for Medicinal Products for Human Use) enables applicants to obtain a conditional marketing authorization prior to obtaining the comprehensive clinical data required for an application for a full marketing authorization. Such conditional approvals may be granted for product candidates (including medicines designated as orphan medicinal products) if (1) the risk-benefit balance of the product candidate is positive, (2) it is likely that the applicant will be in a position to provide the required comprehensive clinical trial data, (3) the product fulfills unmet medical needs and (4) the benefit to public health of the immediate availability on the market of the medicinal product concerned outweighs the risk inherent in the fact that additional data are still required. A conditional marketing authorization may contain specific obligations to be fulfilled by the marketing authorization holder, including obligations with respect to the completion of ongoing or new studies, and with respect to the collection of pharmacovigilance data. Conditional marketing authorizations are valid for one year, and may be renewed annually, if the risk-benefit balance remains positive, and after an assessment of the need for additional or modified conditions and/or specific obligations. The timelines for the centralized procedure described above also apply with respect to the review by the CHMP of applications for a conditional marketing authorization.
Marketing Authorization under Exceptional Circumstances
Under Article 14(8) Regulation (EC) No 726/2004, products for which the applicant can demonstrate that comprehensive data (in line with the requirements laid down in Annex I of Directive 2001/83/EC, as amended) cannot be provided (due to specific reasons foreseen in the legislation) might be eligible for marketing authorization under exceptional circumstances. This type of authorization is reviewed annually to reassess the risk-benefit balance. The fulfillment of any specific procedures/obligations imposed as part of the marketing authorization under exceptional circumstances is aimed at the provision of information on the safe and effective use of the product and will normally not lead to the completion of a full dossier/approval.
Enhanced Pathways
Enhanced pathways including a potential rolling review of clinical data by EMA have become more common as a result of the COVID-19 pandemic, but significant requirements have to be met to benefit from such enhanced or facilitated pathways to approval.
Market Authorizations Granted by Authorities of EU Member States
In general, if the centralized procedure is not followed, there are three alternative procedures as prescribed in Directive 2001/83/EC:
•The decentralized procedure allows applicants to file identical applications to several EU Member States and receive simultaneous national approvals based on the recognition by EU Member States of an assessment by a reference member state.
•The mutual recognition procedure is based on the acceptance by the competent authorities of the EU Member States of the marketing authorization of a medicinal product by the competent authorities of another EU Member State.
•The national procedure is only available for products intended to be authorized in a single EU Member State. A marketing authorization may be granted only to an applicant established in the EU.
Pediatric Studies
Prior to obtaining a marketing authorization in the EU, applicants have to demonstrate compliance with all measures included in an EMA-approved Pediatric Investigation Plan (“PIP”) covering all subsets of the pediatric population, unless the EMA has granted a product-specific waiver, a class waiver, or a deferral for one or more of the measures included in the PIP. The respective requirements for all marketing authorization procedures are set forth in Regulation (EC) No 1901/2006, which is referred to as the Pediatric Regulation. This requirement also applies when a company wants to add a new indication, pharmaceutical form or route of administration for a medicine that is already authorized. The Pediatric Committee of the EMA (“PDCO”) may grant deferrals for some medicines, allowing a company to delay development of the medicine in children until there is enough information to demonstrate its effectiveness and safety in adults. The PDCO may also grant waivers when development of a medicine in children is not needed or is not appropriate, such as for diseases that only affect the elderly population.
Before a marketing authorization application can be filed, or an existing marketing authorization can be amended, the EMA determines that companies actually comply with the agreed studies and measures listed in each relevant PIP.
Periods of Authorization and Renewals
A marketing authorization is valid for five years in principle and the marketing authorization may be renewed after five years on the basis of a re-evaluation of the risk-benefit balance by the competent authority of the authorizing EU Member State. To this end, the marketing authorization holder must provide the EMA or the competent authority with a consolidated version of the file in respect of quality, safety and efficacy, including all variations introduced since the marketing authorization was granted, at least six months before the marketing authorization ceases to be valid. Once renewed, the marketing authorization is valid for an unlimited period, unless the European Commission or the competent authority decides, on justified grounds relating to pharmacovigilance, to proceed with one additional five-year renewal. Any authorization which is not followed by the actual placing of the product on the EU market (in case of centralized procedure) or on the market of the authorizing EU Member State within three years after authorization ceases to be valid (the so-called sunset clause).
Orphan Designation and Exclusivity
Pursuant to Regulation (EC) No 141/2000 and Regulation (EC) No. 847/2000, the European Commission can grant such orphan medicinal product designation to products for which the sponsor can establish that it is intended for the diagnosis, prevention or treatment of a life-threatening or chronically debilitating condition affecting not more than five in 10,000 people in the EU when the application is made, or a life threatening, seriously debilitating or serious and chronic condition in the EU and that without incentives it is unlikely that the product would generate a sufficient return in the EU to justify the necessary investment in its development. In addition, the sponsor must establish that there is no other satisfactory method approved in the EU of diagnosing, preventing or treating the condition, or if such a method exists, the proposed orphan product will be of significant benefit to patients.
Orphan designation is not a marketing authorization. It is a designation that provides a number of benefits, including fee reductions, regulatory assistance, and the possibility to apply for a centralized EU marketing authorization, as well as ten years of market exclusivity following a marketing authorization. During this market exclusivity period, neither the EMA, the European Commission nor the EU Member States can accept an application or grant a marketing authorization for a “similar medicinal product.” A “similar medicinal product” is defined as a medicinal product containing a similar active substance or substances as those contained in an authorized orphan medicinal product and that is intended for the same therapeutic indication. The market exclusivity period for the authorized therapeutic indication may be reduced to six years if, at the end of the fifth year, it is established that the orphan designation criteria are no longer met, including where it is shown that the product is sufficiently profitable not to justify maintenance of market exclusivity. In addition, a competing similar medicinal product may, in limited circumstances, be authorized prior to the expiration of the market exclusivity period, including if it is shown to be safer, more effective or otherwise clinically superior to the already approved orphan product. Furthermore, a product can lose orphan designation, and the related benefits, prior to obtaining a marketing authorization if it is demonstrated that the orphan designation criteria are no longer met.
Regulatory Data Protection
EU legislation also provides for a system of regulatory data and market exclusivity. According to Article 14(11) of Regulation (EC) No 726/2004, as amended, and Article 10(1) of Directive 2001/83/EC, as amended, upon receiving marketing authorization, new chemical entities approved on the basis of complete and independent data package benefit from eight years of data exclusivity and an additional two years of market exclusivity. Data exclusivity prevents regulatory authorities in the EU from referencing the innovator’s data to assess a generic (abbreviated) application. During the additional two-year period of market exclusivity, a generic marketing authorization can be submitted, and the innovator’s data may be referenced, but no generic medicinal product can be marketed until the expiration of the market exclusivity. The overall ten-year period will be extended to a maximum of eleven years if, during the first eight years of those ten years, the marketing authorization holder (“MAH”) obtains an authorization for one or more new therapeutic indications which, during the scientific evaluation prior to their authorization, are held to bring a significant clinical benefit in comparison with existing therapies. Even if a compound is considered to be a new chemical entity and the innovator is able to gain the period of data exclusivity, another company nevertheless could also market another version of the product if such company obtained marketing authorization based on an MAA with a complete and independent data package of pharmaceutical tests, preclinical tests and clinical trials. However, products designated as orphan medicinal products enjoy, upon receiving marketing authorization, a period of ten years of orphan market exclusivity-see also Orphan Designation and Exclusivity. Depending upon the timing and duration of the EU marketing authorization process, products may be eligible for up to five years’ supplementary protection certificates (“SPCs”) pursuant to Regulation (EC) No 469/2009. Such SPCs extend the rights under the basic patent for the product.
Regulatory Requirements after a Marketing Authorization Has Been Obtained
If Akari obtains authorization for a medicinal product in the EU, Akari will be required to comply with a range of requirements applicable to the manufacturing, marketing, promotion and sale of medicinal products.
Pharmacovigilance and Other Requirements
Akari will, for example, have to comply with the EU’s stringent pharmacovigilance or safety reporting rules, pursuant to which post-authorization studies and additional monitoring obligations can be imposed. Other requirements relate, for example, to the manufacturing of products and APIs in accordance with good manufacturing practice standards. EU regulators may conduct inspections to verify Akari’s compliance with applicable requirements, and Akari will have to continue to expend time, money and effort to remain compliant. Non-compliance with EU requirements regarding safety monitoring or pharmacovigilance, and with requirements related to the development of products for the pediatric population, can also result in significant financial penalties in the EU. Similarly, failure to comply with the EU’s requirements regarding the protection of individual personal data can also lead to significant penalties and sanctions. Individual EU Member States may also impose various sanctions and penalties in case Akari does not comply with locally applicable requirements.
Manufacturing
The manufacturing of authorized product, for which a separate manufacturer’s license is mandatory, must be conducted in strict compliance with the EMA’s GMP requirements and comparable requirements of other regulatory bodies in the EU, which mandate the methods, facilities and controls used in manufacturing, processing and packing of products to assure their safety and identity. The EMA enforces its current GMP requirements through mandatory registration of facilities and inspections of those facilities. The EMA may have a coordinating role for these inspections while the responsibility for carrying them out rests with the EU Member States competent authority under whose responsibility the manufacturer falls. Failure to comply with these requirements could interrupt supply and result in delays, unanticipated costs and lost revenues, and could subject the applicant to potential legal or regulatory action, including but not limited to warning letters, suspension of manufacturing, seizure of product, injunctive action or possible civil and criminal penalties.
Marketing and Promotion
The marketing and promotion of authorized products, including industry-sponsored continuing medical education and advertising directed toward the prescribers of drugs and/or the general public, are strictly regulated in the EU under Directive 2001/83/EC and EU Member States’ national law implementing it. The applicable regulations aim to ensure that information provided by holders of marketing authorizations regarding their products is truthful, balanced and accurately reflects the safety and efficacy claims authorized by the EMA or by the competent authority of the authorizing EU Member State. Failure to comply with these requirements can result in adverse publicity, warning letters, corrective advertising and potential civil and criminal penalties.
Patent Term Extension
In order to compensate the patentee for delays in obtaining a marketing authorization for a patented product, an SPC may be granted extending the exclusivity period for that specific product by up to five years.
A six-month pediatric extension of an SPC may be obtained where the patentee has carried out an agreed pediatric investigation plan, the authorized product information includes information on the results of the studies and the product is authorized in all Member States of the EU. The six-month pediatric extension of SPCs is not available for medicinal products that are designated as orphan medicinal products, as such products benefit from a separate two-year pediatric extension of orphan status and exclusivity. The six-month pediatric extension of SPCs is, however, available for medicinal products which were originally designated as orphan medicinal products but were subsequently (voluntarily) removed from the EU’s Register of Orphan Medicinal Products.
The aforementioned EU rules are generally applicable in the European Economic Area which includes the EU Member States, Iceland, Liechtenstein and Norway.
Reform of the Regulatory Framework in the European Union
The European Commission introduced legislative proposals in April 2023 that, if implemented, will replace the current regulatory framework in the EU for all medicines (including those for rare diseases and for children). The European Commission has provided the legislative proposals to the European Parliament and the European Council for their review and approval. In October 2023, the European Parliament published draft reports proposing amendments to the legislative proposals, which will be debated by the European Parliament. Once the European Commission’s legislative proposals are approved (with or without amendment), they will be adopted into EU law.
UK Regulation
The UK ceased being a Member State of the EU on January 31, 2020, and the EU and the UK have concluded a TCA, which was provisionally applicable since January 1, 2021 and has been formally applicable since May 1, 2021. The TCA includes specific provisions concerning pharmaceuticals, which include the mutual recognition of GMP, inspections of manufacturing facilities for medicinal products and GMP documents issued, but does not provide for wholesale mutual recognition of UK and EU pharmaceutical regulations. At present, Great Britain has implemented previous EU legislation on the marketing, promotion and sale of medicinal products through the Human Medicines Regulations 2012 (as amended) (under the Northern Ireland Protocol, the EU regulatory framework currently continues to apply in Northern Ireland). Except in respect of the EU Clinical Trials Regulation, the regulatory regime in Great Britain therefore aligns in many ways with current EU medicines regulations, however it is possible that these regimes will diverge more significantly in the future now that Great Britain’s regulatory system is independent from the EU and the TCA does not provide for mutual recognition of UK and EU pharmaceutical legislation. However, notwithstanding that there is no wholesale recognition of EU pharmaceutical legislation under the TCA, under a new international recognition framework mentioned below which was put in place by the MHRA on January 1, 2024, the MHRA may take into account decisions on the approval of marketing authorizations from the EMA (and certain other regulators) when considering an application for a Great Britain or UK marketing authorization.
On February 27, 2023, the UK government and the European Commission announced a political agreement in principle to replace the Northern Ireland Protocol with a new set of arrangements, known as the “Windsor
Framework”. This new framework fundamentally changes the existing system under the Northern Ireland Protocol, including with respect to the regulation of medicinal products in the UK. In particular, the MHRA will be responsible for approving all medicinal products destined for the UK market (i.e., Great Britain and Northern Ireland), and the EMA will no longer have any role in approving medicinal products destined for Northern Ireland. A single UK-wide marketing authorization will be granted by the MHRA for all medicinal products to be sold in the UK, enabling products to be sold in a single pack and under a single authorization throughout the UK. The Windsor Framework was approved by the EU-UK Joint Committee on March 24, 2023, so the UK government and the EU will enact legislative measures to bring it into law. On June 9, 2023, the MHRA announced that the medicines aspects of the Windsor Framework will apply from January 1, 2025.
Great Britain is no longer covered by the EU’s procedures for the grant of marketing authorizations (Northern Ireland is currently covered by the centralized authorization procedure and can be covered as a concerned member state under the decentralized or mutual recognition procedures). A separate marketing authorization will be required to market products in Great Britain. On January 1, 2024, a new international recognition framework was put in place by the MHRA, under which the MHRA may have regard to decisions on the approval of marketing authorizations made by the EMA and certain other regulators. Various national procedures are now available to place a product on the market in the UK, Great Britain, or Northern Ireland. The MHRA offers a 150-day assessment timeline for all high quality applications for a UK, Great Britain or Northern Ireland marketing authorization. The 150 day timeline does not, however, include a “clock-stop” period which may occur if issues arise or points require clarification following an initial assessment of the application. Such issues should be addressed within a 60-day period, although extensions may be granted in exceptional cases.
Foreign Regulation
In addition to regulations in the United States, the European Union and the UK, Akari will be subject to a variety of other foreign regulations governing clinical trials and commercial sales and distribution of Akari’s products. Whether or not Akari obtains FDA, EMA or MHRA approval for a product, Akari must obtain approval by the comparable regulatory authorities of other countries or areas before Akari may commence clinical trials or market products in those countries or areas. The approval process and requirements governing the conduct of clinical trials, product licensing, pricing and reimbursement vary greatly from place to place, and the time may be longer or shorter than that required for FDA, EMA or MHRA approval.
Pharmaceutical Pricing and Reimbursement
Sales of pharmaceutical products depend in significant part on the extent of coverage and reimbursement from government programs, including Medicare and Medicaid in the U.S., and other third party payers. Third party payers are sensitive to the cost of drugs and are increasingly seeking to implement cost containment measures to control, restrict access to, or influence the purchase of drugs, biologicals, and other health care products and services. Governments may regulate reimbursement, pricing, and coverage of products in order to control costs or to affect levels of use of certain products. Payers may restrict coverage of some products due to cost concerns, by various means such as using payer formularies under which only selected drugs are covered, variable co-payments that make drugs that are not preferred by the payer more expensive in terms of higher out-of-pocket expenses for patients, and by employing utilization management controls, such as discouraging patients’ use of copay coupons and discount cards and imposing requirements for prior authorization before a prescription can be billed or prior clinical failure on another type of treatment before a new product can be prescribed. Payers may especially impose these obstacles to coverage for higher-priced drugs in order to limit the payer’s cost for treatment of the disease. Consequently, any future products may be subject to payer-driven restrictions, rendering patients responsible for a higher percentage of the total cost of drugs in the outpatient setting. This could lower the demand for any future products if the increased patient out-of-pocket cost-sharing obligations are more than they can afford.
Medicare is a U.S. federal government insurance program that covers individuals aged 65 years or older, as well as individuals of any age with certain disabilities, and individuals with End-Stage Renal Disease. The primary Medicare programs that may affect reimbursement for Akari are Medicare Part B, which covers physician services and outpatient care, and Medicare Part D, which provides a voluntary outpatient prescription drug benefit. Medicare Part B provides limited coverage of certain outpatient drugs and biologicals that are reasonable and necessary for
diagnosis or treatment of an illness or injury. Under Medicare Part B, reimbursement for most drugs is based on a fixed percentage above the applicable product’s average sales price (“ASP”). Manufacturers calculate ASP based on a statutory formula and must report ASP information on a quarterly basis to the Centers for Medicare and Medicaid Services (“CMS”), the federal agency that administers Medicare and the Medicaid Drug Rebate Program. The current reimbursement rate for drugs and biologicals in both the hospital outpatient department setting and the physician office setting is ASP + 6%. The rate for the physician clinic setting is set by statute, but CMS has the authority to adjust the rate for the hospital outpatient setting on an annual basis. This reimbursement rate may decrease in the future. In both settings, the amount of reimbursement for a product’s usage is updated quarterly based on the manufacturer’s submission of new ASP information about its product or based on the submission of ASP information of each manufacturer that sells a product for which there are multiple competitors in that product market.
Medicare Part D is a prescription drug benefit available to all Medicare beneficiaries. It is a voluntary benefit that is implemented through private plans under contractual arrangements with the federal government. Similar to pharmaceutical coverage through private health insurance, Part D plans negotiate discounts from drug manufacturers. Medicare Part D coverage is available through private plans, and the list of prescription drugs covered by Part D plans varies by plan. However, individual plans are required by statute to cover certain therapeutic categories and classes of drugs or biologicals and to have at least two drugs in each unique therapeutic category or class, with certain exceptions. As further described below under “U.S. Healthcare Reform and Other U.S. Healthcare Laws,” the Inflation Reduction Act of 2022 (“IRA”) has made significant changes to the Medicare Part B and Medicare Part D prescription drug benefit are structured.
Beginning April 1, 2013, the Budget Control Act of 2011, Pub. L. No. 112-25, as amended by the American Taxpayer Relief Act of 2012, Pub. L. 112-240, required Medicare payments for all items and services, including drugs and biologicals, to be reduced by 2% under sequestration (i.e., automatic spending reductions). Subsequent legislation extended the 2% reduction, on average, through 2031. This 2% reduction in Medicare payments affects all parts of the Medicare program and could impact any future sales of any future products.
Various states, such as California, have also taken steps to consider and enact laws or regulations that are intended to increase the visibility of the pricing of pharmaceutical products with the goal of reducing the prices at which Akari is able to sell Akari’s products. Because these various actual and proposed legislative changes are intended to operate on a state-by-state level rather than a national one, Akari cannot predict what the full effect of these legislative activities may be on Akari’s business in the future. Medicaid is a government health insurance program for low-income children, families, pregnant women, and people with disabilities. It is jointly funded by the federal and state governments, and it is administered by individual states within parameters established by the federal government. Coverage and reimbursement for drugs and biologics thus varies by state. Drugs and biologics may be covered under the medical or pharmacy benefit. State Medicaid programs may impose utilization management controls, such as prior authorization, step therapy, or quantity limits on drugs and biologics. Medicaid also includes the Medicaid Drug Rebate Program, under which, as a condition of coverage for Akari’s future products by the individual state Medicaid programs, Akari will be required to pay a retrospective rebate to each state Medicaid program for the quarterly utilization of Akari’s products by those respective state Medicaid programs Akari would be required to pay a rebate to each state Medicaid program for quantities of any future products that are dispensed to Medicaid beneficiaries and paid for by a state Medicaid program as a condition of having federal funds being made available to the states for any future products under Medicaid and Medicare Part B. Those rebates are based on pricing data that would be reported by us on a monthly and quarterly basis to CMS. These data include the average manufacturer price and the best price for each product Akari sells. As further described below under “U.S. Healthcare Reform and Other U.S. Healthcare Laws,” the Patient Protection and Affordable Care Act, as amended by the Health Care and Education Reconciliation Act of 2010 (collectively, the “PPACA”) made significant changes to how the Medicaid Drug Rebate Program operates.
Federal law requires that any company that participates in the Medicaid Drug Rebate Program also participate in the Public Health Service’s 340B drug discounted pricing program in order for federal funds to be available for the manufacturer’s drugs under Medicaid and Medicare Part B. The 340B pricing program requires participating manufacturers to agree to charge statutorily-defined covered entities no more than the 340B “ceiling price” for the manufacturer’s covered outpatient drugs. These 340B covered entities include a variety of community health clinics and other entities that receive health services grants from the Public Health Service as well as hospitals that serve a
disproportionate share of low-income patients. The 340B ceiling price is calculated using a statutory formula, which is based on the average manufacturer price and rebate amount for the covered outpatient drug as calculated under the Medicaid Drug Rebate Program. Changes to the definition of average manufacturer price and the Medicaid rebate amount under PPACA and CMS’s issuance of final regulations implementing those changes also could affect the 340B ceiling price calculation for any future products and could negatively impact Akari’s results of operations. As described below under “U.S. Healthcare Reform and Other U.S. Healthcare Laws,” PPACA expanded the 340B program to include additional types of covered entities but exempts “orphan drugs” designated under section 526 of the FDCA from the ceiling price requirements for these newly-eligible entities. CMS has also implemented new regulations that further define and further expand which health care provider entities are eligible to purchase approved drugs at the discounted 340B prices.
In order to be eligible to have products paid for with federal funds under the Medicaid and Medicare Part B programs and purchased by certain federal agencies and grantees, manufacturers must participate in the Department of Veterans Affairs Federal Supply Schedule (“FSS”) pricing program, established by Section 603 of the Veterans Health Care Act of 1992 (“VHCA”). Under this program, Akari would be obligated to make Akari’s innovator “covered drugs” available for procurement on an FSS contract and charge a price to four federal agencies, Department of Veterans Affairs, Department of Defense, Public Health Service and Coast Guard, the so-called “Big Four” government purchasers, that is no higher than the statutory Federal Ceiling Price (“FCP”). The FCP is based on the non-federal average manufacturer price (“Non-FAMP”), which Akari would calculate and report to the Department of Veterans Affairs on a quarterly and annual basis. Under the Tricare Retail Pharmacy program, established by Section 703 of the National Defense Authorization Act, participating manufacturers pay quarterly rebates on utilization of innovator products that are dispensed through the Tricare Retail Pharmacy network to Tricare beneficiaries. The rebates are calculated as the difference between Annual Non-FAMP and FCP. The FCP is based on a weighted average Non-FAMP, which manufacturers are required to report on a quarterly and annual basis to the VA. If a company misstates Non-FAMPs or FCPs it must restate these figures and potentially refund to the government purchasers any overcharges that occurred.
Pursuant to the VHCA, knowing provision of false information in connection with a Non-FAMP filing can subject a manufacturer to significant civil monetary penalties for each item of false information.
FSS contracts are federal procurement contracts that include standard government terms and conditions, separate pricing for each product, and extensive disclosure and certification requirements. All items on FSS contracts are subject to a standard FSS contract clause that requires FSS contract price reductions under certain circumstances where pricing is reduced to an agreed “tracking customer.” Further, in addition to the “Big Four” agencies, all other federal agencies and some non-federal entities are authorized to access FSS contracts. FSS contractors are permitted to charge FSS purchasers other than the Big Four agencies “negotiated pricing” for covered drugs that is not capped by the FCP; instead, such pricing is negotiated based on a mandatory disclosure of the contractor’s commercial “most favored customer” pricing.
In addition, in some foreign countries, the proposed pricing for a drug must be approved before it may be lawfully marketed. Moreover, the requirements governing drug pricing and reimbursement vary widely from country to country. For example, in the EU, the national authorities of the individual EU Member States are free to restrict the range of medicinal products for which their national health insurance systems provide reimbursement and to control the prices and/or reimbursement of medicinal products for human use. Some individual EU Member States adopt policies according to which a specific price or level of reimbursement is approved for the medicinal product. Other EU Member States adopt a system of reference pricing, basing the price or reimbursement level in their territory either, on the pricing and reimbursement levels in other countries, or on the pricing and reimbursement levels of medicinal products intended for the same therapeutic indication. Some EU Member States may require the completion of additional studies that compare the cost effectiveness of a particular product candidate to currently available therapies (so called health technology assessments) in order to obtain reimbursement or pricing approval. Furthermore, some EU Member States impose direct or indirect controls on the profitability of the company placing the medicinal product on the market. There can be no assurance that any country that has price controls or reimbursement limitations for pharmaceutical products will allow favorable reimbursement and pricing arrangements for any of Akari’s product candidates. Historically, products launched in the EU do not follow price structures of the U.S. and generally prices tend to be significantly lower.
U.S. Healthcare Reform and Other U.S. Healthcare Laws
In addition to FDA restrictions on marketing of pharmaceutical products, several other types of state and federal healthcare laws, including those commonly referred to as “fraud and abuse” laws have been applied in recent years to restrict certain marketing practices in the pharmaceutical industry. These laws may impact, among other things, Akari’s proposed sales, marketing and education programs. In addition, Akari may be subject to patient privacy regulation by both the U.S. federal government and the states in which Akari conducts Akari’s business. The laws that may affect Akari’s ability to operate include the following:
•The federal Anti-Kickback Statute prohibits, among other things, knowingly and willfully soliciting, offering, receiving, or paying any remuneration, directly or indirectly, in cash or in kind, to induce or reward purchasing, ordering or arranging for or recommending the purchase or order of any item or service for which payment may be made, in whole or in part, under a federal healthcare program such as Medicare and Medicaid. Liability may be established without a person or entity having actual knowledge of the federal Anti-Kickback Statute or specific intent to violate it. This statute has been interpreted to apply broadly to arrangements between pharmaceutical manufacturers on the one hand and prescribers, patients, purchasers and formulary managers on the other. In addition, PPACA amended the Social Security Act to provide that the government may assert that a claim including items or services resulting from a violation of the federal Anti-Kickback Statute constitutes a false or fraudulent claim for purposes of the federal civil False Claims Act. A conviction for violation of the Anti-Kickback Statute requires mandatory exclusion from participation in federal health care programs. Although there are a number of statutory exemptions and regulatory safe harbors protecting certain common activities from prosecution, the exemptions and safe harbors are drawn narrowly, and those activities may be subject to scrutiny or penalty if they do not qualify for an exemption or safe harbor.
•The federal civil False Claims Act (“FCA”) prohibits, among other things, knowingly presenting, or causing to be presented claims for payment of government funds that are false or fraudulent, or knowingly making, using or causing to be made or used a false record or statement material to such a false or fraudulent claim, or knowingly concealing or knowingly and improperly avoiding, decreasing, or concealing an obligation to pay money to the federal government. This statute also permits a private individual acting as a “whistleblower” to bring actions on behalf of the federal government alleging violations of the FCA and to share in any monetary recovery. The FCA prohibits anyone from knowingly presenting, conspiring to present, making a false statement in order to present, or causing to be presented, for payment to federal programs (including Medicare and Medicaid) claims for items or services, including drugs, that are false or fraudulent, claims for items or services not provided as claimed, or claims for medically unnecessary items or services. This law also prohibits anyone from knowingly underpaying an obligation owed to a federal program. Increasingly, U.S. federal agencies are requiring nonmonetary remedial measures, such as corporate integrity agreements in FCA settlements. FCA liability is potentially significant in the healthcare industry because the statute provides for treble damages and mandatory penalties of $13,946 to $27,894 per false claim or statement for penalties assessed after January 15, 2024. Government enforcement agencies and private whistleblowers have investigated pharmaceutical companies for or asserted liability under the FCA for a variety of alleged promotional and marketing activities, such as providing free product to customers with the expectation that the customers would bill federal programs for the product; providing consulting fees and other benefits to physicians to induce them to prescribe products; engaging in promotion for “off-label” uses; and submitting inflated best price information to the Medicaid Rebate Program; among other reasons.
•The federal False Statements Statute prohibits knowingly and willfully falsifying, concealing, or covering up a material fact or making any materially false, fictitious or fraudulent statement or representation, or making or using any false writing or document knowing the same to contain any materially false, fictitious or fraudulent statement or entry, in connection with the delivery of or payment for healthcare benefits, items, or services.
•The federal Civil Monetary Penalties Law authorizes the imposition of substantial civil monetary penalties against an entity, such as a pharmaceutical manufacturer, that engages in activities including, among others (1) knowingly presenting, or causing to be presented, a claim for services not provided as claimed or that is otherwise false or fraudulent in any way; (2) arranging for or contracting with an individual or entity that is excluded from participation in federal healthcare programs to provide items
or services reimbursable by a federal healthcare program; (3) violations of the federal Anti-Kickback Statute; or (4) failing to report and return a known overpayment.
•HIPAA imposes criminal and civil liability for knowingly and willfully executing, or attempting to execute, a scheme to defraud any healthcare benefit program, or knowingly and willfully falsifying, concealing or covering up a material fact or making any materially false statement in connection with the delivery of, or payment for, healthcare benefits, items or services; similar to the federal Anti-Kickback Statute, a person or entity does not need to have actual knowledge of the statute or specific intent to violate it in order to have committed a violation.
•The majority of states also have statutes similar to the federal anti-kickback law and false claims laws that apply to items and services reimbursed under Medicaid and other state programs, or, in several states, that apply regardless of whether the payer is a government entity or a private commercial entity.
•The federal Open Payments (Physician Payments Sunshine Act) program requires manufacturers of products for which payment is available under Medicare, Medicaid or the State Children’s Health Insurance Program, to track and report annually to the federal government (for disclosure to the public) certain payments and other transfers of value made to physicians and other licensed practitioners (such as nurse practitioners, certified nurse anesthetists, physician assistants, and others) as well as teaching hospitals and ownership and investment interests held by physicians and their immediate family members. In addition, several U.S. states and localities have enacted legislation requiring pharmaceutical companies to establish marketing compliance programs, file periodic reports with the state, and/or make periodic public disclosures on sales, marketing, pricing, clinical trials, and other activities. Other state laws prohibit certain marketing-related activities including the provision of gifts, meals or other items to certain healthcare providers. Many of these laws and regulations contain ambiguous requirements that government officials have not yet clarified. Given the lack of clarity in the laws and their implementation, Akari’s reporting actions could be subject to the penalty provisions of the pertinent federal and state laws and regulations.
•Federal price reporting laws require manufacturers to calculate and report complex pricing metrics to government programs, where such reported prices may be used in the calculation of reimbursement and/or discounts on approved products.
•Federal consumer protection and unfair competition laws broadly regulate marketplace activities and activities that potentially harm consumers.
Sanctions under these federal and state healthcare laws may include civil monetary penalties, exclusion of a manufacturer’s products from reimbursement under government programs, monetary damages, criminal fines, disgorgement, additional reporting obligations and oversight if the manufacture becomes subject to a corporate integrity agreement or other agreement to resolve allegations of non-compliance with these laws, and individual imprisonment.
Federal and state authorities are continuing to devote significant attention and resources to enforcement of fraud and abuse laws within the pharmaceutical industry, and private individuals have been active in alleging violations of the law and bringing suits on behalf of the government under the FCA. For example, federal enforcement agencies recently have investigated certain pharmaceutical companies’ product and patient assistance programs, including manufacturer reimbursement support services, relationships with specialty pharmacies, and grants to independent charitable foundations.
The PPACA was adopted in the U.S. in March 2010. This law substantially changes the way healthcare is financed by both governmental and private insurers in the U.S., and significantly impacts the pharmaceutical industry. PPACA contains a number of provisions that are expected to impact Akari’s business and operations. Changes that may affect Akari’s business include those governing enrollment in federal healthcare programs, reimbursement changes, rules regarding prescription drug benefits under the health insurance exchanges, expansion of the 340B program, expansion of state Medicaid programs, and fraud and abuse and enforcement. These changes will impact existing government healthcare programs and will result in the development of new programs, including Medicare payment for performance initiatives and improvements to the physician quality reporting system and feedback program.
PPACA contains several provisions that have or could potentially impact Akari’s business. PPACA made significant changes to the Medicaid Drug Rebate Program. For example, under PPACA, rebate liability expanded from fee-for-service Medicaid utilization to include the utilization of Medicaid managed care organizations as well. With regard to the amount of the rebates owed, PPACA increased the minimum Medicaid rebate from 15.1% to 23.1% of the average manufacturer price for most innovator products; extended the Medicaid Drug Rebate program to utilization of prescriptions of individuals enrolled in Medicaid managed care organizations; changed the calculation of the rebate for certain innovator products that qualify as line extensions of existing drugs; and capped the total rebate amount for innovator drugs at 100% of the average manufacturer price. In addition, PPACA and subsequent legislation changed the definition of average manufacturer price; subjected manufacturers to new annual fees and taxes for certain branded prescription drugs; created the Medicare Part D coverage gap discount program, in which manufacturers must agree to 70% point-of-sale discounts off negotiated prices of applicable brand drugs to eligible beneficiaries during their coverage gap period, as a condition for the manufacturer’s outpatient drugs to be covered under Medicare Part D; and provided incentives to programs that increase the federal government’s comparative effectiveness research.
PPACA requires pharmaceutical manufacturers of branded prescription drugs to pay a branded prescription drug fee to the federal government. Generally, a fee is imposed by the IRS on each manufacturer or importer of branded prescription drug sales of over $5 million to specific government programs, such as Medicare and Medicaid. Sales of “orphan drugs” are excluded from this fee. “Orphan drugs” are specifically defined for purposes of the fee. For each indication approved by the FDA for the drug, such indication must have been designated as orphan by the FDA under section 526 of the FDCA, an orphan drug tax credit under section 45C of the Internal Revenue Code must have been claimed with respect to such indication, and such tax credit must not have been disallowed by the IRS. Finally, the FDA must not have approved the drug for any indication other than an orphan indication for which a section 45C orphan drug tax credit was claimed (and not disallowed).
Additional provisions of PPACA may negatively affect manufacturer’s revenues in the future. For example, PPACA created the Medicare Part D coverage gap discount program, which manufacturers of branded prescription drugs are required to provide a 50% discount (extended by subsequent legislation to 70%) on branded prescription drugs at the point-of-sale dispensed to beneficiaries when they are in the coverage gap for out-of-pocket spending (commonly known as the “donut hole”).
PPACA also expanded the Public Health Service’s 340B drug pricing discount program. The 340B pricing program requires participating manufacturers to agree to charge statutorily-defined covered entities no more than the 340B “ceiling price” for the manufacturer’s covered outpatient drugs. PPACA expanded the 340B program to include additional types of covered entities: certain free-standing cancer hospitals, critical access hospitals, rural referral centers and sole community hospitals, each as defined by PPACA. PPACA exempts “orphan drugs” designated under section 526 of the FDCA, from the ceiling price requirements for these newly-eligible entities.
In addition to PPACA, the IRA includes several provisions that may impact Akari’s business to varying degrees, including provisions that reduce the out-of-pocket spending cap for Medicare Part D beneficiaries from $7,050 to $2,000 starting in 2025, thereby effectively eliminating the coverage gap; impose new manufacturer financial liability on certain drugs under Medicare Part D, allow the U.S. government to negotiate Medicare Part B and Part D price caps for certain high-cost drugs and biologics without generic or biosimilar competition; require companies to pay rebates to Medicare for certain drug prices that increase faster than inflation; and delay until January 1, 2032 the implementation of the HHS rebate rule that would have limited the fees that pharmacy benefit managers can charge. Further, under the IRA, orphan drugs are exempted from the Medicare drug price negotiation program, but only if they have one orphan designation and for which the only approved indication is for that disease or condition. If a product receives multiple orphan designations or has multiple approved indications, it may not qualify for the orphan drug exemption. The implementation of the IRA is currently subject to ongoing litigation that challenges the constitutionality of the IRA’s Medicare drug price negotiation program. The effects of the IRA on Akari’s business and the healthcare industry in general is not yet known.
Finally, numerous federal and state laws, including state security breach notification laws, state health information privacy laws, and federal and state consumer protection laws govern the collection, use, and disclosure of personal information. In addition, most healthcare providers and research institutions with whom Akari collaborates are subject to privacy and security requirements under HIPAA, as amended by HITECH, and its
implementing regulations. Although Akari is currently neither a “covered entity” nor a “business associate” under HIPAA, and these privacy and security requirements do not apply to Akari, the regulations may affect Akari’s interactions with healthcare providers, health plans, and research institutions from whom Akari obtains patient health information. Further, Akari could be subject to criminal penalties if Akari knowingly obtains individually identifiable health information from a HIPAA covered entity in a manner that is not authorized or permitted by HIPAA or for aiding and abetting the violation of HIPAA.
There is significant interest in the United States in promoting changes in healthcare systems with the stated goals of containing healthcare costs, improving quality and/or expanding access, including increasing legislative and enforcement interest in the United States with respect to specialty drug pricing practices, particularly with respect to drugs that have been subject to relatively large price increases over relatively short time periods. There have been several recent U.S. Congressional inquiries and proposed bills designed to, among other things, bring more transparency to drug pricing and reform government program reimbursement methodologies for drugs. Although multiple efforts to repeal or replace portions of the PPACA have been introduced, and multiple judicial challenges to the PPACA have also been attempted. Further, Executive Orders relating to the regulation of prescription drug pricing have also been introduced over time. Akari cannot predict the scope or impact of future legislative, judicial, or executive efforts to reform healthcare in the United States.
Other Regulations
Akari is also subject to the U.S. Foreign Corrupt Practices Act (“FCPA”), the U.K. Bribery Act (“Bribery Act”), and other anticorruption laws and regulations pertaining to Akari’s financial relationships with foreign government officials. The FCPA prohibits U.S. companies and their representatives from paying, offering to pay, promising, or authorizing the payment of anything of value to any foreign government official, government staff member, political party, or political candidate to obtain or retain business or to otherwise seek favorable treatment. In many countries in which Akari operates, the healthcare professionals with whom Akari interacts may be deemed to be foreign government officials for purposes of the FCPA. The Bribery Act, which applies to any company incorporated or doing business in the UK, prohibits giving, offering, or promising bribes in the public and private sectors, bribing a foreign public official or private person, and failing to have adequate procedures to prevent bribery amongst employees and other agents. Penalties under the Bribery Act include potentially unlimited fines for companies and criminal sanctions for corporate officers under certain circumstances. Liability in relation to breaches of the Bribery Act is strict. This means that it is not necessary to demonstrate elements of a corrupt state of mind.
Recent years have seen a substantial increase in anti-bribery law enforcement activity by U.S. regulators, with more frequent and aggressive investigations and enforcement proceedings by both the U.S. Department of Justice and the SEC, increased enforcement activity by non-U.S. regulators, and increases in criminal and civil proceedings brought against companies and individuals. Increasing regulatory scrutiny of the promotional activities of pharmaceutical companies also has been observed in a number of EU member states. In Germany, a specific anti-corruption provision with regard to healthcare professionals was introduced in the Criminal Code in 2017.
Similar strict restrictions are imposed on the promotion and marketing of products in the EU, where a large portion of Akari’s non-U.S. business is conducted, and other territories. Laws in the EU, including in the individual EU Member States, require promotional materials and advertising for products to comply with the product’s Summary of Product Characteristics (“SmPC”), which is approved by the competent authorities. Promotion of a medicinal product which does not comply with the SmPC is considered to constitute off-label promotion. The off-label promotion of medicinal products is prohibited in the EU and in other territories. The promotion of medicinal products that are not subject to a marketing authorization is also prohibited in the EU. Laws in the EU, including in the individual EU Member States, also prohibit the direct-to-consumer advertising of prescription-only medicinal products. Violations of the rules governing the promotion of medicinal products in the EU and in other territories could be penalized by administrative measures, fines and imprisonment. Furthermore, illegal advertising can be challenged by competitors, and as a result, can be prohibited by court and the responsible company can be obligated to pay damages to the competitor.
Interactions between pharmaceutical companies and physicians are also governed by strict laws, regulations, industry self-regulation codes of conduct and physicians’ codes of professional conduct in the individual EU Member States. The provision of any inducements to physicians to prescribe, recommend, endorse, order, purchase,
supply, use or administer a medicinal product is prohibited. A number of EU Member States have introduced additional rules requiring pharmaceutical companies to publicly disclose their interactions with physicians and to obtain approval from employers, professional organizations and/or competent authorities before entering into agreements with physicians. These rules have been supplemented by provisions of related industry codes, including the EFPIA Disclosure Code on Disclosure of Transfers of Value from Pharmaceutical Companies to Healthcare Professionals and Healthcare Organizations and related codes developed at national level in individual EU Member States. Additional countries may consider or implement similar laws and regulations. Violations of these rules could lead to reputational risk, public reprimands, and/or the imposition of fines or imprisonment. Akari’s present and future business has been and will continue to be subject to various other laws and regulations. Laws, regulations and recommendations relating to safe working conditions, laboratory practices, the experimental use of animals, and the purchase, storage, movement, import and export and use and disposal of hazardous or potentially hazardous substances, including radioactive compounds, used in connection with Akari’s research work are or may be applicable to Akari’s activities. Akari cannot predict the impact of government regulation, which may result from future legislation or administrative action, on Akari’s business.
Employees and Human Capital Resources
Akari’s mission is to deliver advanced therapies to improve the lives of patients and families battling autoimmune and inflammatory diseases. Accordingly, Akari is a team who is passionate about and committed to Akari’s mission and establishing a culture where patients and their families are at the center of all Akari does, with core values that connect us to each other and Akari’s stakeholders, and define who Akari is, what Akari stand for, and how Akari works.
As of September 9, 2024, Akari had 6 employees, 5 of which are full-time. None of Akari’s employees are represented by labor unions or covered by collective bargaining agreements, and Akari considers Akari’s relationship with employees to be good. Akari also utilizes the services of several independent consultants to support Akari’s research and development and general and administrative operations, including Akari’s Interim CEO, Samir R. Patel, M.D. and Akari’s Interim CFO, Wendy DiCicco.
Akari is focused on effective identification, recruitment, development, and retention of, and compensation and benefits to, human resource talent, including workforce and management development, diversity and inclusion initiatives, succession planning, and corporate culture and leadership quality, which are vital to Akari’s success. The principal purposes of Akari’s equity incentive plans are to attract, retain and motivate selected employees, consultants and directors through the granting of stock-based compensation awards and cash-based performance bonus awards.
Corporate Information
Akari was originally established as a private limited company under the laws of England and Wales on October 7, 2004 under the name Freshname No. 333 Limited. On January 19, 2005, Akari changed Akari’s name to Morria Biopharmaceuticals Limited and on February 3, 2005, Akari completed a reverse merger with Morria Biopharmaceuticals Inc., or Morria, a Delaware corporation, in which Morria became Akari’s wholly owned subsidiary and we re-registered as a non-traded public limited company under the laws of England and Wales. On March 22, 2011, Akari incorporated an Israeli subsidiary, Morria Biopharma Ltd. On June 25, 2013, Akari changed its name to Celsus Therapeutics Plc and on October 13, 2013 Morria was renamed Celsus Therapeutics Inc. On September 18, 2015, Akari completed an acquisition of all of the capital stock of Volution Immuno Pharmaceuticals SA (“Volution”), a private Swiss company, from RPC Pharma Limited (“RPC”), Volution’s sole shareholder, in exchange for Akari’s ordinary shares, in accordance with the terms of a Share Exchange Agreement, dated as of July 10, 2015. In connection with the acquisition, Akari’s name was changed to Akari Therapeutics, Plc. As such, Akari’s affairs are governed by Akari’s Articles of Association and the English law.
Akari’s principal UK office is located at 75/76 Wimpole Street, London W1G 9RT, United Kingdom, and Akari’s telephone number is +44 20 8004 0270. Puglisi & Associates (“Puglisi”) serves as Akari’s agent for service of process in the United States. Puglisi’s address is 850 Library Avenue, Suite 204, Newark, Delaware 1971.
Akari’s principal U.S. office is located at 22 Boston Wharf Road FL 7, Boston, Massachusetts 02210, and Akari’s telephone number is (929) 274-7510. Celsus Therapeutics, Inc. serves as Akari’s agent for service of process in the United States.
Description of Properties
Akari currently leases office space for both our U.K. and U.S. headquarters on a short-term basis. The lease for Akari’s U.K. headquarters, located in London, expires in July 2025. Akari leases its U.S. headquarters office space, located in Boston, MA. The lease for Akari’s U.S. headquarters office space expires in November 2024. Akari is not party to any material lease agreements.
Legal Proceedings
From time to time, Akari may become involved in litigation relating to claims arising out of operations in the normal course of business, which Akari considers routine and incidental to our business. Akari currently is not a party to any legal proceedings the adverse outcome of which, in management’s opinion, would have a material adverse effect on Akari’s business, results of operation or financial condition.
v3.24.3
Cover
|
Sep. 13, 2024 |
| Document Information [Line Items] |
|
| Document Type |
8-K
|
| Amendment Flag |
false
|
| Document Period End Date |
Sep. 13, 2024
|
| Entity File Number |
001-36288
|
| Entity Registrant Name |
Akari Therapeutics, Plc
|
| Entity Central Index Key |
0001541157
|
| Entity Tax Identification Number |
98-1034922
|
| Entity Incorporation, State or Country Code |
X0
|
| Entity Address, Address Line One |
22 Boston Wharf Road FL 7
|
| Entity Address, City or Town |
Boston
|
| Entity Address, State or Province |
MA
|
| Entity Address, Postal Zip Code |
02210
|
| City Area Code |
929
|
| Local Phone Number |
274-7510
|
| Written Communications |
false
|
| Soliciting Material |
false
|
| Pre-commencement Tender Offer |
false
|
| Pre-commencement Issuer Tender Offer |
false
|
| Entity Emerging Growth Company |
false
|
| ADR [Member] |
|
| Document Information [Line Items] |
|
| Title of 12(b) Security |
American Depositary Shares, each representing 2,000 Ordinary Shares
|
| Trading Symbol |
AKTX
|
| Security Exchange Name |
NASDAQ
|
| Ordinary Shares, par value $0.0001 per share [Member] |
|
| Document Information [Line Items] |
|
| Title of 12(b) Security |
Ordinary Shares, par value $0.0001 per share*
|
| No Trading Symbol Flag |
true
|
| X |
- DefinitionBoolean flag that is true when the XBRL content amends previously-filed or accepted submission.
| Name: |
dei_AmendmentFlag |
| Namespace Prefix: |
dei_ |
| Data Type: |
xbrli:booleanItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionFor the EDGAR submission types of Form 8-K: the date of the report, the date of the earliest event reported; for the EDGAR submission types of Form N-1A: the filing date; for all other submission types: the end of the reporting or transition period. The format of the date is YYYY-MM-DD.
| Name: |
dei_DocumentPeriodEndDate |
| Namespace Prefix: |
dei_ |
| Data Type: |
xbrli:dateItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionThe type of document being provided (such as 10-K, 10-Q, 485BPOS, etc). The document type is limited to the same value as the supporting SEC submission type, or the word 'Other'.
| Name: |
dei_DocumentType |
| Namespace Prefix: |
dei_ |
| Data Type: |
dei:submissionTypeItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionAddress Line 1 such as Attn, Building Name, Street Name
| Name: |
dei_EntityAddressAddressLine1 |
| Namespace Prefix: |
dei_ |
| Data Type: |
xbrli:normalizedStringItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- Definition
+ References
+ Details
| Name: |
dei_EntityAddressCityOrTown |
| Namespace Prefix: |
dei_ |
| Data Type: |
xbrli:normalizedStringItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionCode for the postal or zip code
| Name: |
dei_EntityAddressPostalZipCode |
| Namespace Prefix: |
dei_ |
| Data Type: |
xbrli:normalizedStringItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionName of the state or province.
| Name: |
dei_EntityAddressStateOrProvince |
| Namespace Prefix: |
dei_ |
| Data Type: |
dei:stateOrProvinceItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionA unique 10-digit SEC-issued value to identify entities that have filed disclosures with the SEC. It is commonly abbreviated as CIK. Reference 1: http://www.xbrl.org/2003/role/presentationRef
-Publisher SEC
-Name Exchange Act
-Number 240
-Section 12
-Subsection b-2
| Name: |
dei_EntityCentralIndexKey |
| Namespace Prefix: |
dei_ |
| Data Type: |
dei:centralIndexKeyItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionIndicate if registrant meets the emerging growth company criteria. Reference 1: http://www.xbrl.org/2003/role/presentationRef
-Publisher SEC
-Name Exchange Act
-Number 240
-Section 12
-Subsection b-2
| Name: |
dei_EntityEmergingGrowthCompany |
| Namespace Prefix: |
dei_ |
| Data Type: |
xbrli:booleanItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionCommission file number. The field allows up to 17 characters. The prefix may contain 1-3 digits, the sequence number may contain 1-8 digits, the optional suffix may contain 1-4 characters, and the fields are separated with a hyphen.
| Name: |
dei_EntityFileNumber |
| Namespace Prefix: |
dei_ |
| Data Type: |
dei:fileNumberItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionTwo-character EDGAR code representing the state or country of incorporation.
| Name: |
dei_EntityIncorporationStateCountryCode |
| Namespace Prefix: |
dei_ |
| Data Type: |
dei:edgarStateCountryItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionThe exact name of the entity filing the report as specified in its charter, which is required by forms filed with the SEC. Reference 1: http://www.xbrl.org/2003/role/presentationRef
-Publisher SEC
-Name Exchange Act
-Number 240
-Section 12
-Subsection b-2
| Name: |
dei_EntityRegistrantName |
| Namespace Prefix: |
dei_ |
| Data Type: |
xbrli:normalizedStringItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionThe Tax Identification Number (TIN), also known as an Employer Identification Number (EIN), is a unique 9-digit value assigned by the IRS. Reference 1: http://www.xbrl.org/2003/role/presentationRef
-Publisher SEC
-Name Exchange Act
-Number 240
-Section 12
-Subsection b-2
| Name: |
dei_EntityTaxIdentificationNumber |
| Namespace Prefix: |
dei_ |
| Data Type: |
dei:employerIdItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionLocal phone number for entity.
| Name: |
dei_LocalPhoneNumber |
| Namespace Prefix: |
dei_ |
| Data Type: |
xbrli:normalizedStringItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionBoolean flag that is true only for a security having no trading symbol.
| Name: |
dei_NoTradingSymbolFlag |
| Namespace Prefix: |
dei_ |
| Data Type: |
dei:trueItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionBoolean flag that is true when the Form 8-K filing is intended to satisfy the filing obligation of the registrant as pre-commencement communications pursuant to Rule 13e-4(c) under the Exchange Act. Reference 1: http://www.xbrl.org/2003/role/presentationRef
-Publisher SEC
-Name Exchange Act
-Number 240
-Section 13e
-Subsection 4c
| Name: |
dei_PreCommencementIssuerTenderOffer |
| Namespace Prefix: |
dei_ |
| Data Type: |
xbrli:booleanItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionBoolean flag that is true when the Form 8-K filing is intended to satisfy the filing obligation of the registrant as pre-commencement communications pursuant to Rule 14d-2(b) under the Exchange Act. Reference 1: http://www.xbrl.org/2003/role/presentationRef
-Publisher SEC
-Name Exchange Act
-Number 240
-Section 14d
-Subsection 2b
| Name: |
dei_PreCommencementTenderOffer |
| Namespace Prefix: |
dei_ |
| Data Type: |
xbrli:booleanItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionTitle of a 12(b) registered security. Reference 1: http://www.xbrl.org/2003/role/presentationRef
-Publisher SEC
-Name Exchange Act
-Number 240
-Section 12
-Subsection b
| Name: |
dei_Security12bTitle |
| Namespace Prefix: |
dei_ |
| Data Type: |
dei:securityTitleItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionName of the Exchange on which a security is registered. Reference 1: http://www.xbrl.org/2003/role/presentationRef
-Publisher SEC
-Name Exchange Act
-Number 240
-Section 12
-Subsection d1-1
| Name: |
dei_SecurityExchangeName |
| Namespace Prefix: |
dei_ |
| Data Type: |
dei:edgarExchangeCodeItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionBoolean flag that is true when the Form 8-K filing is intended to satisfy the filing obligation of the registrant as soliciting material pursuant to Rule 14a-12 under the Exchange Act. Reference 1: http://www.xbrl.org/2003/role/presentationRef
-Publisher SEC
-Name Exchange Act
-Number 240
-Section 14a
-Subsection 12
| Name: |
dei_SolicitingMaterial |
| Namespace Prefix: |
dei_ |
| Data Type: |
xbrli:booleanItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionTrading symbol of an instrument as listed on an exchange.
| Name: |
dei_TradingSymbol |
| Namespace Prefix: |
dei_ |
| Data Type: |
dei:tradingSymbolItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionBoolean flag that is true when the Form 8-K filing is intended to satisfy the filing obligation of the registrant as written communications pursuant to Rule 425 under the Securities Act. Reference 1: http://www.xbrl.org/2003/role/presentationRef
-Publisher SEC
-Name Securities Act
-Number 230
-Section 425
| Name: |
dei_WrittenCommunications |
| Namespace Prefix: |
dei_ |
| Data Type: |
xbrli:booleanItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- Details
| Name: |
us-gaap_StatementClassOfStockAxis=dei_AdrMember |
| Namespace Prefix: |
|
| Data Type: |
na |
| Balance Type: |
|
| Period Type: |
|
|
| X |
- Details
| Name: |
us-gaap_StatementClassOfStockAxis=aktx_OrdinarySharesParValue0.0001PerShareMember |
| Namespace Prefix: |
|
| Data Type: |
na |
| Balance Type: |
|
| Period Type: |
|
|
Akari Therapeutics (NASDAQ:AKTX)
過去 株価チャート
から 9 2024 まで 10 2024
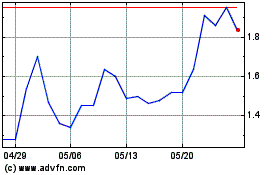
Akari Therapeutics (NASDAQ:AKTX)
過去 株価チャート
から 10 2023 まで 10 2024