falseQ212-3100018324662024xbrli:sharesiso4217:USDiso4217:USDxbrli:sharesalhc:Entityalhc:segmentxbrli:pure00018324662024-01-012024-06-3000018324662024-07-2900018324662024-06-3000018324662023-12-3100018324662024-04-012024-06-3000018324662023-04-012023-06-3000018324662023-01-012023-06-300001832466us-gaap:CommonStockMember2024-03-310001832466us-gaap:AdditionalPaidInCapitalMember2024-03-310001832466us-gaap:RetainedEarningsMember2024-03-310001832466us-gaap:NoncontrollingInterestMember2024-03-3100018324662024-03-310001832466us-gaap:RetainedEarningsMember2024-04-012024-06-300001832466us-gaap:NoncontrollingInterestMember2024-04-012024-06-300001832466us-gaap:CommonStockMember2024-04-012024-06-300001832466us-gaap:AdditionalPaidInCapitalMember2024-04-012024-06-300001832466us-gaap:CommonStockMember2024-06-300001832466us-gaap:AdditionalPaidInCapitalMember2024-06-300001832466us-gaap:RetainedEarningsMember2024-06-300001832466us-gaap:NoncontrollingInterestMember2024-06-300001832466us-gaap:CommonStockMember2023-03-310001832466us-gaap:AdditionalPaidInCapitalMember2023-03-310001832466us-gaap:RetainedEarningsMember2023-03-310001832466us-gaap:NoncontrollingInterestMember2023-03-3100018324662023-03-310001832466us-gaap:CommonStockMember2023-04-012023-06-300001832466us-gaap:AdditionalPaidInCapitalMember2023-04-012023-06-300001832466us-gaap:RetainedEarningsMember2023-04-012023-06-300001832466us-gaap:NoncontrollingInterestMember2023-04-012023-06-300001832466us-gaap:CommonStockMember2023-06-300001832466us-gaap:AdditionalPaidInCapitalMember2023-06-300001832466us-gaap:RetainedEarningsMember2023-06-300001832466us-gaap:NoncontrollingInterestMember2023-06-3000018324662023-06-300001832466us-gaap:CommonStockMember2023-12-310001832466us-gaap:AdditionalPaidInCapitalMember2023-12-310001832466us-gaap:RetainedEarningsMember2023-12-310001832466us-gaap:NoncontrollingInterestMember2023-12-310001832466us-gaap:RetainedEarningsMember2024-01-012024-06-300001832466us-gaap:NoncontrollingInterestMember2024-01-012024-06-300001832466us-gaap:CommonStockMember2024-01-012024-06-300001832466us-gaap:AdditionalPaidInCapitalMember2024-01-012024-06-300001832466us-gaap:CommonStockMember2022-12-310001832466us-gaap:AdditionalPaidInCapitalMember2022-12-310001832466us-gaap:RetainedEarningsMember2022-12-310001832466us-gaap:NoncontrollingInterestMember2022-12-3100018324662022-12-310001832466us-gaap:RetainedEarningsMember2023-01-012023-06-300001832466us-gaap:NoncontrollingInterestMember2023-01-012023-06-300001832466us-gaap:CommonStockMember2023-01-012023-06-300001832466us-gaap:AdditionalPaidInCapitalMember2023-01-012023-06-300001832466us-gaap:FairValueInputsLevel3Member2023-12-310001832466us-gaap:FairValueInputsLevel3Member2024-06-300001832466us-gaap:HealthCarePremiumMember2024-04-012024-06-300001832466us-gaap:HealthCarePremiumMember2023-04-012023-06-300001832466us-gaap:HealthCarePremiumMember2024-01-012024-06-300001832466us-gaap:HealthCarePremiumMember2023-01-012023-06-300001832466alhc:HealthCareCapitationMember2024-04-012024-06-300001832466alhc:HealthCareCapitationMember2023-04-012023-06-300001832466alhc:HealthCareCapitationMember2024-01-012024-06-300001832466alhc:HealthCareCapitationMember2023-01-012023-06-300001832466alhc:RealizingEquityAccessAndCommunityHealthREACHModelMember2024-04-012024-06-300001832466alhc:RealizingEquityAccessAndCommunityHealthREACHModelMember2024-01-012024-06-300001832466alhc:RealizingEquityAccessAndCommunityHealthREACHModelMember2023-04-012023-06-300001832466alhc:RealizingEquityAccessAndCommunityHealthREACHModelMember2023-01-012023-06-300001832466srt:MinimumMember2024-01-012024-06-300001832466us-gaap:ComputerEquipmentMember2024-06-300001832466srt:MinimumMemberalhc:OfficeEquipmentAndFurnitureMember2024-06-300001832466srt:MaximumMemberalhc:OfficeEquipmentAndFurnitureMember2024-06-300001832466us-gaap:SoftwareDevelopmentMembersrt:MinimumMember2024-06-300001832466us-gaap:SoftwareDevelopmentMembersrt:MaximumMember2024-06-300001832466us-gaap:LeaseholdImprovementsMember2024-06-3000018324662023-01-012023-12-310001832466us-gaap:StockOptionMember2024-01-012024-06-300001832466us-gaap:StockOptionMember2023-01-012023-06-300001832466us-gaap:RestrictedStockUnitsRSUMember2024-01-012024-06-300001832466us-gaap:RestrictedStockUnitsRSUMember2023-01-012023-06-300001832466us-gaap:USTreasurySecuritiesMember2024-06-300001832466us-gaap:USTreasurySecuritiesMemberus-gaap:FairValueInputsLevel1Member2024-06-300001832466us-gaap:USTreasurySecuritiesMemberus-gaap:FairValueInputsLevel2Member2024-06-300001832466us-gaap:USTreasurySecuritiesMemberus-gaap:FairValueInputsLevel3Member2024-06-300001832466us-gaap:CertificatesOfDepositMember2024-06-300001832466us-gaap:CertificatesOfDepositMemberus-gaap:FairValueInputsLevel1Member2024-06-300001832466us-gaap:FairValueInputsLevel2Memberus-gaap:CertificatesOfDepositMember2024-06-300001832466us-gaap:CertificatesOfDepositMemberus-gaap:FairValueInputsLevel3Member2024-06-300001832466us-gaap:FairValueInputsLevel1Member2024-06-300001832466us-gaap:FairValueInputsLevel2Member2024-06-300001832466us-gaap:USTreasurySecuritiesMember2023-12-310001832466us-gaap:USTreasurySecuritiesMemberus-gaap:FairValueInputsLevel1Member2023-12-310001832466us-gaap:USTreasurySecuritiesMemberus-gaap:FairValueInputsLevel2Member2023-12-310001832466us-gaap:USTreasurySecuritiesMemberus-gaap:FairValueInputsLevel3Member2023-12-310001832466us-gaap:CertificatesOfDepositMember2023-12-310001832466us-gaap:CertificatesOfDepositMemberus-gaap:FairValueInputsLevel1Member2023-12-310001832466us-gaap:FairValueInputsLevel2Memberus-gaap:CertificatesOfDepositMember2023-12-310001832466us-gaap:CertificatesOfDepositMemberus-gaap:FairValueInputsLevel3Member2023-12-310001832466us-gaap:FairValueInputsLevel1Member2023-12-310001832466us-gaap:FairValueInputsLevel2Member2023-12-310001832466us-gaap:USTreasuryBillSecuritiesMemberus-gaap:ShortTermInvestmentsMember2024-06-300001832466us-gaap:USTreasuryBillSecuritiesMemberus-gaap:ShortTermInvestmentsMember2023-12-310001832466us-gaap:USTreasuryBillSecuritiesMember2024-06-300001832466us-gaap:CashAndCashEquivalentsMemberus-gaap:USTreasuryBillSecuritiesMember2024-06-300001832466us-gaap:CashAndCashEquivalentsMemberus-gaap:USTreasuryBillSecuritiesMember2023-12-310001832466us-gaap:USTreasuryBillSecuritiesMember2023-12-310001832466us-gaap:ComputerEquipmentMember2023-12-310001832466us-gaap:FurnitureAndFixturesMember2024-06-300001832466us-gaap:FurnitureAndFixturesMember2023-12-310001832466alhc:SoftwareMember2024-06-300001832466alhc:SoftwareMember2023-12-310001832466us-gaap:LeaseholdImprovementsMember2023-12-310001832466us-gaap:ConstructionInProgressMember2024-06-300001832466us-gaap:ConstructionInProgressMember2023-12-310001832466alhc:MedicalExpensesMember2024-04-012024-06-300001832466alhc:MedicalExpensesMember2023-04-012023-06-300001832466alhc:MedicalExpensesMember2024-01-012024-06-300001832466alhc:MedicalExpensesMember2023-01-012023-06-300001832466us-gaap:LicenseMember2024-06-300001832466alhc:PlanRelationshipMember2024-06-300001832466alhc:PlanRelationshipMember2024-01-012024-06-300001832466us-gaap:OtherIntangibleAssetsMember2024-06-300001832466srt:MinimumMemberus-gaap:OtherIntangibleAssetsMember2024-01-012024-06-300001832466srt:MaximumMemberus-gaap:OtherIntangibleAssetsMember2024-01-012024-06-300001832466us-gaap:LicenseMember2023-12-310001832466alhc:PlanRelationshipMember2023-12-310001832466alhc:PlanRelationshipMember2023-01-012023-12-310001832466us-gaap:OtherIntangibleAssetsMember2023-12-310001832466srt:MinimumMemberus-gaap:OtherIntangibleAssetsMember2023-01-012023-12-310001832466srt:MaximumMemberus-gaap:OtherIntangibleAssetsMember2023-01-012023-12-310001832466us-gaap:SecuredDebtMemberalhc:OxfordTermLoanMember2022-09-020001832466us-gaap:SecuredDebtMemberus-gaap:DelayedDrawTermLoanMember2022-09-022022-09-020001832466us-gaap:SecuredDebtMemberus-gaap:DelayedDrawTermLoanMember2024-06-142024-06-140001832466us-gaap:DelayedDrawTermLoanMember2024-06-300001832466us-gaap:SecuredDebtMemberalhc:OxfordTermLoanMemberus-gaap:BaseRateMember2022-09-022022-09-020001832466us-gaap:SecuredDebtMemberalhc:OxfordTermLoanMember2022-09-022022-09-020001832466us-gaap:SecuredDebtMemberalhc:OxfordTermLoanMembersrt:MinimumMember2024-01-012024-06-300001832466us-gaap:SecuredDebtMembersrt:MaximumMemberalhc:OxfordTermLoanMember2024-04-012024-06-300001832466us-gaap:SecuredDebtMemberus-gaap:DelayedDrawTermLoanMember2022-09-020001832466us-gaap:SecuredDebtMembersrt:MinimumMember2022-09-020001832466us-gaap:DomesticCountryMember2024-01-012024-06-300001832466us-gaap:DomesticCountryMember2024-06-300001832466srt:SubsidiariesMemberus-gaap:DomesticCountryMember2024-06-300001832466us-gaap:DomesticCountryMember2023-12-310001832466us-gaap:StateAndLocalJurisdictionMember2023-12-310001832466us-gaap:EmployeeStockOptionMember2024-01-012024-06-3000018324662024-01-012024-03-310001832466us-gaap:RestrictedStockMember2024-01-012024-06-300001832466alhc:PreIpoAwardsConvertedRestrictedStockAwardsMember2024-01-012024-06-300001832466us-gaap:RestrictedStockMember2023-12-310001832466us-gaap:RestrictedStockMember2023-01-012023-03-310001832466us-gaap:RestrictedStockMember2024-03-310001832466us-gaap:RestrictedStockMember2024-04-012024-06-300001832466us-gaap:RestrictedStockMember2024-06-300001832466us-gaap:RestrictedStockUnitsRSUMember2023-12-310001832466us-gaap:RestrictedStockUnitsRSUMember2024-01-012024-03-310001832466us-gaap:RestrictedStockUnitsRSUMember2024-03-310001832466us-gaap:RestrictedStockUnitsRSUMember2024-04-012024-06-300001832466us-gaap:RestrictedStockUnitsRSUMember2024-06-300001832466srt:MinimumMemberalhc:PerformanceBasedRestrictedStockUnitsMember2023-09-142023-09-140001832466srt:MaximumMemberalhc:PerformanceBasedRestrictedStockUnitsMember2023-09-142023-09-140001832466alhc:PerformanceBasedRestrictedStockUnitsMembersrt:ScenarioForecastMember2024-12-310001832466alhc:PerformanceBasedRestrictedStockUnitsMembersrt:ScenarioForecastMember2025-03-012025-03-010001832466alhc:PerformanceBasedRestrictedStockUnitsMembersrt:ScenarioForecastMember2025-12-312025-12-310001832466srt:MinimumMemberalhc:PerformanceBasedRestrictedStockUnitsMember2024-03-132024-03-130001832466srt:MaximumMemberalhc:PerformanceBasedRestrictedStockUnitsMember2024-03-132024-03-130001832466alhc:PerformanceBasedRestrictedStockUnitsMembersrt:ScenarioForecastMember2026-12-310001832466alhc:PerformanceBasedRestrictedStockUnitsMembersrt:ScenarioForecastMember2027-03-012027-03-010001832466alhc:PerformanceBasedRestrictedStockUnitsMember2023-12-310001832466alhc:PerformanceBasedRestrictedStockUnitsMember2024-01-012024-03-310001832466alhc:PerformanceBasedRestrictedStockUnitsMember2024-03-310001832466alhc:PerformanceBasedRestrictedStockUnitsMember2024-04-012024-06-300001832466alhc:PerformanceBasedRestrictedStockUnitsMember2024-06-300001832466us-gaap:SellingGeneralAndAdministrativeExpensesMember2024-04-012024-06-300001832466us-gaap:SellingGeneralAndAdministrativeExpensesMember2023-04-012023-06-300001832466us-gaap:SellingGeneralAndAdministrativeExpensesMember2024-01-012024-06-300001832466us-gaap:SellingGeneralAndAdministrativeExpensesMember2023-01-012023-06-300001832466alhc:NonVestedAwardsRsaOptionsAndRsuMember2024-01-012024-06-3000018324662023-08-152023-08-15
UNITED STATES
SECURITIES AND EXCHANGE COMMISSION
WASHINGTON, DC 20549
_______________________________________
FORM 10-Q
_______________________________________
(Mark One)
| | | | | |
| x | QUARTERLY REPORT PURSUANT TO SECTION 13 OR 15(d) OF THE SECURITIES EXCHANGE ACT OF 1934 |
For the quarterly period ended June 30, 2024
OR
| | | | | |
| o | TRANSITION REPORT PURSUANT TO SECTION 13 OR 15(d) OF THE SECURITIES EXCHANGE ACT OF 1934 |
For the transition period from to
Commission File Number: 001-40295
_______________________________________
ALIGNMENT HEALTHCARE, INC.
(Exact Name of Registrant as Specified in its Charter)
_______________________________________
| | | | | |
| Delaware | 46-5596242 |
(State or other jurisdiction of incorporation or organization) | (I.R.S. Employer Identification No.) |
1100 W. Town and Country Road, Suite 1600 Orange, California | 92868 |
| (Address of principal executive offices) | (Zip Code) |
Registrant’s telephone number, including area code: (844) 310-2247
_______________________________________
Securities registered pursuant to Section 12(b) of the Act:
| | | | | | | | | | | | | | |
| Title of each class | | Trading Symbol(s) | | Name of each exchange on which registered |
| Common Stock, par value $0.001 per share | | ALHC | | The Nasdaq Stock Market LLC |
Indicate by check mark whether the registrant (1) has filed all reports required to be filed by Section 13 or 15(d) of the Securities Exchange Act of 1934 during the preceding 12 months (or for such shorter period that the registrant was required to file such reports), and (2) has been subject to such filing requirements for the past 90 days. Yes x No o
Indicate by check mark whether the registrant has submitted electronically every Interactive Data File required to be submitted pursuant to Rule 405 of Regulation S-T (§232.405 of this chapter) during the preceding 12 months (or for such shorter period that the registrant was required to submit such files). Yes x No o
Indicate by check mark whether the registrant is a large accelerated filer, an accelerated filer, a non-accelerated filer, smaller reporting company, or an emerging growth company. See the definitions of “large accelerated filer,” “accelerated filer,” “smaller reporting company,” and “emerging growth company” in Rule 12b-2 of the Exchange Act.
| | | | | | | | | | | | | | | | | | | | |
| Large accelerated Filer | | x | | Accelerated filer | | o |
| Non-accelerated filer | | o | | Smaller reporting company | | o |
| Emerging growth company | | o | | | | |
If an emerging growth company, indicate by check mark if the registrant has elected not to use the extended transition period for complying with any new or revised financial accounting standards provided pursuant to Section 13(a) of the Exchange Act. o
Indicate by check mark whether the registrant is a shell company (as defined in Rule 12b-2 of the Exchange Act). Yes o No x
As of July 29, 2024, the registrant had 191,299,946 shares of common stock, $0.001 par value per share, outstanding.
Table of Contents
FORWARD-LOOKING STATEMENTS
Throughout this quarterly report on Form 10-Q (this “Quarterly Report”), we make “forward-looking statements” within the meaning of the U.S. Private Securities Litigation Reform Act of 1995. All statements other than statements of historical fact included in this Quarterly Report are forward-looking statements. Forward-looking statements give our current expectations relating to our financial condition, results of operations, plans, objectives, future performance and business. You can identify forward-looking statements by the fact that they do not relate strictly to historical or current facts. These statements may include words such as “anticipate,” “estimate,” “expect,” “project,” “plan,” “intend,” “believe,” “may,” “will,” “should,” “can have,” “likely” and other words and terms of similar meaning. The forward-looking statements contained in this Quarterly Report are generally located in the material set forth under the heading “Management’s Discussion and Analysis of Financial Condition and Results of Operations” but may be found in other locations as well. These statements are based upon management’s current expectations, assumptions and estimates and are not guarantees of timing, future results or performance. All forward-looking statements are subject to risks and uncertainties that may cause actual results to differ materially from those that we expected, including:
•our history of net losses, and our ability to achieve or maintain profitability in an environment of increasing expenses;
•the effect of our relatively limited operating history on investors’ ability to evaluate our current business and future prospects;
•the viability of our growth strategy and our ability to realize expected results;
•our ability to attract new members and to successfully enter into new markets;
•the quality and pricing of our products and services;
•our ability to maintain a high rating for our health plans on the Five Star Quality Rating System;
•our ability to develop and maintain satisfactory relationships with care providers that service our members;
•our ability to manage our growth effectively, execute our business plan, maintain high levels of service and member satisfaction or adequately address competitive challenges;
•our ability to compete in the healthcare industry;
•the impact on our business of security breaches, loss of data or other disruptions causing the compromise of sensitive information or preventing us from accessing critical information;
•the impact on our business of disruptions in our disaster recovery systems or management continuity planning;
•the cost of legal proceedings and litigation, including intellectual property and privacy disputes;
•our dependence on reimbursements by the Centers for Medicare and Medicaid Services ("CMS") and premium payments by individuals;
•other risks associated with being a government contractor;
•the impact on our business of the healthcare services industry becoming more cyclical;
•our ability to manage acquisitions, divestitures and other significant transactions successfully;
•our ability to maintain, enhance and protect our reputation and brand recognition;
•our ability to effectively invest in, implement improvements to and properly maintain the uninterrupted operation and data integrity of our information technology and other business systems;
•our ability to obtain, maintain, protect and enforce intellectual property protection for our technology;
•the potential adverse impact of claims by third parties that we are infringing on, misappropriating or otherwise violating their intellectual property rights;
•the impact of any restrictions on our use of or ability to license data or our failure to license data and integrate third-party technologies;
•our dependence on our senior management team and other key employees;
•the concentration of our health plans in a limited number of U.S. states;
•our management team’s limited experience managing a public company;
•our ability to generate sufficient cash flow to service all of our indebtedness and the potential impact of certain affirmative and negative covenants in our term loan agreement on our business;
•the impact of shortages of qualified personnel and related increases in our labor costs;
•the risk that our records may contain inaccurate or unsupportable information regarding risk adjustment scores of members;
•our ability to accurately estimate incurred but not reported medical expenses;
•the impact of negative publicity regarding the managed healthcare industry;
•the impact of weather and other factors beyond our control on our clinics, the centers out of which our external providers operate, and the facilities that host our AVA platform (as defined below);
•the impact on our business of renegotiation, non-renewal or termination of risk agreements with hospitals, physicians, nurses, pharmacists and medical support staff;
•risks associated with estimating the amount of liabilities that we recognize under our risk agreements with providers;
•our ability to respond to general economic conditions, including but not limited to, increased inflation and higher interest rates;
•risks associated with an economic downturn, including pressure on governmental budgets and reduced spending for health and human service programs;
•our ability to develop and maintain proper and effective internal control over financial reporting;
•the impact of state and federal efforts to reduce Medicare spending;
•our ability to comply with applicable federal, state and local rules and regulations, including those relating to data privacy and security; and
•other factors disclosed in the section entitled “Risk Factors” and elsewhere in this Quarterly Report.
We derive many of our forward-looking statements from our operating budgets and forecasts, which are based on many detailed assumptions. While we believe that our assumptions are reasonable, we caution that it is very difficult to predict the impact of known factors, and it is impossible for us to anticipate all factors that could affect our actual results. Important factors that could cause actual results to differ materially from our expectations, or cautionary statements, are disclosed under the sections entitled “Risk Factors” and “Management’s Discussion and Analysis of Financial Condition and Results of Operations” in this Quarterly Report.
All written and oral forward-looking statements attributable to us, or persons acting on our behalf, are expressly qualified in their entirety by these cautionary statements as well as other cautionary statements that are made from time to time in our other SEC filings and public communications. You should evaluate all forward-looking statements made in this Quarterly Report in the context of these risks and uncertainties.
We caution you that the important factors referenced above may not contain all of the factors that are important to you. In addition, we cannot assure you that we will realize the results or developments we expect or anticipate or, even if substantially realized, that they will result in the consequences or affect us or our operations in the way we expect. The forward-looking statements included in this Quarterly Report are made only as of the date hereof. We undertake no obligation to update or revise any forward-looking statement as a result of new information, future events or otherwise, except as otherwise required by law.
PART I—FINANCIAL INFORMATION
Item 1. Financial Statements.
Alignment Healthcare, Inc.
Condensed Consolidated Balance Sheets
(amounts in thousands, except par value and share amounts)
(Unaudited)
| | | | | | | | | | | |
| | June 30,
2024 | | December 31,
2023 |
| Assets | | | |
| Current Assets: | | | |
| Cash and cash equivalents | $ | 339,007 | | | $ | 202,904 | |
Accounts receivable (less allowance for credit losses of $95 at June 30, 2024 and $0 at December 31, 2023) | 183,214 | | | 119,749 | |
| Investments - current | 24,701 | | | 115,914 | |
| Prepaid expenses and other current assets | 52,191 | | | 44,970 | |
| Total current assets | 599,113 | | | 483,537 | |
| Property and equipment, net | 62,430 | | | 51,901 | |
| Right of use asset, net | 8,085 | | | 9,959 | |
| Goodwill | 34,826 | | | 34,826 | |
| Intangible Assets, net | 5,201 | | | 5,252 | |
| Other assets | 6,603 | | | 6,405 | |
| Total assets | $ | 716,258 | | | $ | 591,880 | |
| Liabilities and Stockholders' Equity | | | |
| Current Liabilities: | | | |
| Medical expenses payable | $ | 315,369 | | | $ | 205,399 | |
| Accounts payable and accrued expenses | 23,336 | | | 23,511 | |
| Accrued compensation | 32,834 | | | 34,112 | |
| Total current liabilities | 371,539 | | | 263,022 | |
| Long-term debt, net of debt issuance costs | 211,742 | | | 161,813 | |
| Long-term portion of lease liabilities | 8,179 | | | 8,974 | |
| Total liabilities | 591,460 | | | 433,809 | |
| Commitments and Contingencies (Note 12) | | | |
| Stockholders' Equity: | | | |
Preferred stock, $.001 par value; 100,000,000 shares authorized as of June 30, 2024 and December 31, 2023, respectively; no shares issued and outstanding as of June 30, 2024 and December 31, 2023 | — | | | — | |
Common stock, $.001 par value; 1,000,000,000 shares authorized as of June 30, 2024 and December 31, 2023; 191,236,747 and 188,951,643 shares issued and outstanding as of June 30, 2024 and December 31, 2023, respectively | 191 | | | 189 | |
| Additional paid-in capital | 1,074,303 | | | 1,037,015 | |
| Accumulated deficit | (950,789) | | | (880,258) | |
| Total Alignment Healthcare, Inc. stockholders' equity | 123,705 | | | 156,946 | |
| Noncontrolling interest | 1,093 | | | 1,125 | |
| Total stockholders' equity | 124,798 | | | 158,071 | |
| Total liabilities and stockholders' equity | $ | 716,258 | | | $ | 591,880 | |
See accompanying notes to unaudited condensed consolidated financial statements.
Alignment Healthcare, Inc.
Condensed Consolidated Statements of Operations
(amounts in thousands, except share and per share amounts)
(Unaudited)
| | | | | | | | | | | | | | | | | | | | | | | |
| Three Months Ended June 30, | | Six Months Ended June 30, |
| 2024 | | 2023 | | 2024 | | 2023 |
| Revenues: | | | | | | | |
| Earned premiums | $ | 674,094 | | | $ | 456,877 | | | $ | 1,295,650 | | | $ | 891,689 | |
| Other | 7,192 | | | 5,502 | | | 14,237 | | | 9,845 | |
| Total revenues | 681,286 | | | 462,379 | | | 1,309,887 | | | 901,534 | |
| Expenses: | | | | | | | |
| Medical expenses | 605,312 | | | 410,644 | | | 1,178,530 | | | 806,959 | |
| Selling, general, and administrative expenses | 87,863 | | | 70,199 | | | 178,375 | | | 140,607 | |
| Depreciation and amortization | 6,493 | | | 5,195 | | | 12,470 | | | 10,116 | |
| Total expenses | 699,668 | | | 486,038 | | | 1,369,375 | | | 957,682 | |
| Loss from operations | (18,382) | | | (23,659) | | | (59,488) | | | (56,148) | |
| Other expenses: | | | | | | | |
| Interest expense | 5,691 | | | 5,262 | | | 11,118 | | | 10,281 | |
| Other income, net | (92) | | | (428) | | | (50) | | | (566) | |
| Total other expenses | 5,599 | | | 4,834 | | | 11,068 | | | 9,715 | |
| Loss before income taxes | (23,981) | | | (28,493) | | | (70,556) | | | (65,863) | |
| Provision for income taxes | 22 | | | 1 | | | 22 | | | 2 | |
| Net loss | $ | (24,003) | | | $ | (28,494) | | | $ | (70,578) | | | $ | (65,865) | |
| Less: Net (income) loss attributable to noncontrolling interest | (7) | | | 17 | | | 47 | | | 104 | |
| Net loss attributable to Alignment Healthcare, Inc. | $ | (24,010) | | | $ | (28,477) | | | $ | (70,531) | | | $ | (65,761) | |
| Total weighted-average common shares outstanding - basic and diluted | 190,891,787 | | 185,991,460 | | | 189,948,725 | | | 184,560,652 |
| Net loss per share - basic and diluted | $ | (0.13) | | | $ | (0.15) | | | $ | (0.37) | | | $ | (0.36) | |
| | | | | | | |
See accompanying notes to unaudited condensed consolidated financial statements.
Alignment Healthcare, Inc.
Condensed Consolidated Statements of Stockholders' Equity
(amounts in thousands, except par value and share amounts)
(Unaudited)
| | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | |
| Common Stock | | | | | | | | |
| Shares | | Amount | | Additional
Paid-In Capital | | Accumulated
Deficit | | Noncontrolling Interest | | Total |
| Balance at March 31, 2024 | 191,156,569 | | $ | 191 | | | $ | 1,057,519 | | | $ | (926,779) | | | $ | 1,086 | | | $ | 132,017 | |
| Net loss | — | | — | | | — | | | (24,010) | | | 7 | | | (24,003) | |
| Issuance of common stock upon vesting of restricted stock units | 80,178 | | — | | | — | | | — | | | — | | | — | |
| | | | | | | | | | | |
| Equity-based compensation | — | | — | | | 16,784 | | | — | | | — | | | 16,784 | |
| Balance at June 30, 2024 | 191,236,747 | | $ | 191 | | | $ | 1,074,303 | | | $ | (950,789) | | | $ | 1,093 | | | $ | 124,798 | |
| | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | |
| Common Stock | | | | | | | | |
| Shares | | Amount | | Additional
Paid-In Capital | | Accumulated
Deficit | | Noncontrolling interest | | Total |
| Balance at March 31, 2023 | 188,475,278 | | $ | 188 | | | $ | 992,158 | | | $ | (769,525) | | | $ | 1,119 | | | $ | 223,940 | |
| Net loss | — | | — | | | — | | | (28,477) | | | (17) | | | (28,494) | |
| Issuance of common stock upon vesting of restricted stock units | 43,195 | | — | | | — | | | — | | | — | | | — | |
| Forfeitures | (5,708) | | — | | | — | | | — | | | — | | | — | |
| Equity-based compensation | — | | — | | | 15,636 | | | — | | | — | | | 15,636 | |
| Noncontrolling interest attributable to subsidiary | — | | — | | | — | | | — | | | 30 | | | 30 | |
| Balance at June 30, 2023 | 188,512,765 | | $ | 188 | | | $ | 1,007,794 | | | $ | (798,002) | | | $ | 1,132 | | | $ | 211,112 | |
See accompanying notes to unaudited condensed consolidated financial statements.
Alignment Healthcare, Inc.
Condensed Consolidated Statements of Stockholders' Equity
(amounts in thousands, except par value and share amounts)
(Unaudited)
| | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | |
| Common Stock | | | | | | | | |
| Shares | | Amount | | Additional
Paid-In Capital | | Accumulated
Deficit | | Noncontrolling interest | | Total |
| Balance at December 31, 2023 | 188,951,643 | | $ | 189 | | | $ | 1,037,015 | | | $ | (880,258) | | | $ | 1,125 | | | $ | 158,071 | |
| Net loss | — | | — | | | — | | | (70,531) | | | (47) | | | (70,578) | |
| Issuance of common stock upon vesting of restricted stock units | 2,357,723 | | 2 | | | — | | | — | | | — | | | 2 | |
| Forfeitures | (2,799) | | — | | | — | | | — | | | — | | | — | |
| Shares withheld related to net restricted stock settlement | (69,820) | | — | | | (350) | | | — | | | — | | | (350) | |
| Equity-based compensation | — | | — | | | 37,638 | | | — | | | — | | | 37,638 | |
| Noncontrolling interest attributable to subsidiary | — | | — | | | — | | | — | | | 15 | | | 15 | |
| Balance at June 30, 2024 | 191,236,747 | | | $ | 191 | | | $ | 1,074,303 | | | $ | (950,789) | | | $ | 1,093 | | | $ | 124,798 | |
| | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | |
| Common Stock | | | | | | | | |
| Shares | | Amount | | Additional
Paid-In Capital | | Accumulated
Deficit | | Noncontrolling interest | | Total |
| Balance at December 31, 2022 | 187,280,015 | | $ | 187 | | | $ | 970,180 | | | $ | (732,241) | | | $ | 1,176 | | | $ | 239,302 | |
| Net loss | — | | — | | | — | | | (65,761) | | | (104) | | | (65,865) | |
| Issuance of common stock upon vesting of restricted stock units | 1,247,972 | | 1 | | | — | | | — | | | | | 1 | |
| Forfeitures | (15,222) | | — | | | — | | | — | | | — | | | — | |
| Equity-based compensation | — | | — | | | 37,614 | | | — | | | — | | | 37,614 | |
| Repurchase of noncontrolling interest attributable to subsidiary | — | | — | | | — | | | — | | | 60 | | | 60 | |
| Balance at June 30, 2023 | 188,512,765 | | $ | 188 | | | $ | 1,007,794 | | | $ | (798,002) | | | $ | 1,132 | | | $ | 211,112 | |
See accompanying notes to unaudited condensed consolidated financial statements.
Alignment Healthcare, Inc.
Condensed Consolidated Statements of Cash Flows
(amounts in thousands)
(Unaudited)
| | | | | | | | | | | |
| Six Months Ended June 30, |
| 2024 | | 2023 |
| Operating Activities: | | | |
| Net loss | $ | (70,578) | | | $ | (65,865) | |
| Adjustments to reconcile net loss to net cash provided by operating activities: | | | |
| Provision for credit loss | 95 | | | 51 | |
| Loss (gain) on right of use assets | 143 | | | (289) | |
| Depreciation and amortization | 12,568 | | | 10,246 | |
| Amortization-investment discount | (1,762) | | | (1,716) | |
| Amortization-debt issuance costs | 612 | | | 734 | |
| Equity-based compensation | 37,638 | | | 37,614 | |
| Non-cash lease expense | 930 | | | 1,348 | |
| Changes in operating assets and liabilities: | | | |
| Accounts receivable | (63,560) | | | 3,914 | |
| Prepaid expenses and other current assets | (7,221) | | | (35,077) | |
| Other assets | 92 | | | (112) | |
| Medical expenses payable | 109,970 | | | 37,063 | |
| Accounts payable and accrued expenses | 1,373 | | | (8,996) | |
| Deferred premium revenue | (310) | | | 147,169 | |
| Accrued compensation | (1,278) | | | (1,632) | |
| Lease liabilities | (1,421) | | | (2,165) | |
| Net cash provided by operating activities | 17,291 | | | 122,287 | |
| Investing Activities: | | | |
| Purchase of investments | (40,000) | | | (156,943) | |
| Maturities of investments | 132,525 | | | 36,150 | |
| Acquisition of property and equipment | (22,854) | | | (15,845) | |
| Net cash provided by (used in) investing activities | 69,671 | | | (136,638) | |
| Financing Activities: | | | |
| Proceeds from long-term debt | 50,000 | | | — | |
| Debt issuance costs | (512) | | | — | |
| Payment of employment taxes related to release of restricted stock | (350) | | | — | |
| Contributions from noncontrolling interest holders | 15 | | | 60 | |
| Net cash provided by financing activities | 49,153 | | | 60 | |
| Net increase (decrease) in cash | 136,115 | | | (14,291) | |
| Cash, cash equivalents and restricted cash at beginning of period | 204,954 | | | 411,299 | |
| Cash, cash equivalents and restricted cash at end of period | $ | 341,069 | | | $ | 397,008 | |
| Supplemental disclosure of cash flow information: | | | |
| Cash paid for interest | $ | 10,247 | | | $ | 8,986 | |
| Supplemental non-cash investing and financing activities: | | | |
| Acquisition of property in accounts payable | $ | 122 | | | $ | 42 | |
The following table provides a reconciliation of cash, cash equivalents and restricted cash reported within the condensed consolidated balance sheets to the total above:
| | | | | | | | | | | |
| | June 30, 2024 | | June 30, 2023 |
| Cash and cash equivalents | $ | 339,007 | | | $ | 395,258 | |
| Restricted cash in other assets | 2,062 | | | 1,750 | |
| Total | $ | 341,069 | | | $ | 397,008 | |
See accompanying notes to unaudited condensed consolidated financial statements.
Alignment Healthcare, Inc.
Notes to Unaudited Condensed Consolidated Financial Statements
(amounts in thousands, except share amounts)
1. Organization
Alignment Healthcare, Inc. (collectively, “we” or “us” or “our” or the “Company”), is a next generation, consumer-centric health care platform that is purpose-built to provide seniors with high quality, affordable care with a vastly improved consumer experience. Enabled by our innovative technology and care delivery model, the Company focuses on improving outcomes in the Medicare Advantage sector. The Company’s operations primarily consist of Medicare Advantage Plans in the states of California, North Carolina, Nevada, Arizona, Florida and Texas.
2. Summary of Significant Accounting Policies
Basis of Presentation
The accompanying condensed consolidated financial statements and accompanying notes have been prepared in accordance with accounting principles generally accepted in the United States of America (“U.S. GAAP”). The balance sheet as of December 31, 2023, included herein, was derived from audited financial statements, but does not include all disclosures required by GAAP. In accordance with the rules and regulations of the U.S. Securities and Exchange Commission ("SEC"), the Company has omitted certain footnote disclosures that would substantially duplicate the disclosures contained in its annual audited consolidated financial statements. Therefore, these condensed consolidated financial statements should be read in conjunction with the Company's Annual Report on Form 10-K for the year-ended December 31, 2023 as filed with the SEC. Furthermore, the condensed consolidated financial statements include the accounts of the Company, our subsidiaries, and three immaterial variable interest entities in which we are the primary beneficiary. All intercompany transactions have been eliminated in consolidation. Noncontrolling interest is presented within the equity section of the condensed consolidated balance sheets.
We have no components of other comprehensive income (loss), and accordingly, comprehensive income (loss) is the same as the net income (loss) for all periods presented.
Use of Estimates
The preparation of the condensed consolidated financial statements requires management to make estimates and judgments that affect the amounts reported in the condensed consolidated financial statements. Our significant estimates include, but are not limited to, the determination of medical expenses payable; the impact of risk adjustment provisions related to our Medicare contracts; collectability of receivables; valuation of related impairment recognition of long-lived assets, including goodwill and intangible assets; equity-based compensation expense; and contingent liabilities. Estimates and judgments are based upon historical information and on various other assumptions that are believed to be reasonable under the circumstances. Actual results could differ materially from those estimates and the impact of any change in estimates is included in earnings in the period in which the estimate is adjusted.
Segments
We have determined that our chief executive officer is the chief operating decision maker (“CODM”) who regularly reviews financial operating results on a consolidated basis for purposes of allocating resources and evaluating financial performance. We operate and manage the business as one reportable segment and one operating segment, which is to provide healthcare services to our seniors. Factors used in determining the reportable segment include the nature of operating activities, our organizational and reporting structure, and the type of information reviewed by the CODM to allocate resources and evaluate financial performance. All of our assets are located in the United States.
Fair Value Measurements
Fair value is the price that would be received to sell an asset or paid to transfer a liability in an orderly transaction between market participants at the measurement date. Our current assets and current liabilities approximate fair value because of the
short-term nature of these financial instruments. Financial instruments measured at fair value on a recurring basis were based upon a three-tier hierarchy as follows:
Level 1 - Quoted prices in active markets for identical assets or liabilities
Level 2 - Other inputs that are observable for the asset or liability, either directly or indirectly, for substantially the full term of the asset or liability
Level 3 - Unobservable inputs that reflect management’s best estimate of what market participants would use in pricing the asset or liability at the measurement date
The fair value of cash, cash equivalents, restricted cash and U.S. Treasury bills was determined based on Level 1 inputs. The fair value of certificate of deposits, which are recorded in other assets in the condensed consolidated balance sheets, was determined based on Level 2 inputs. There were no assets or liabilities measured at fair value using Level 3 inputs as of June 30, 2024 and December 31, 2023. Our long-term debt was reported at carrying value.
Revenue and Accounts Receivable
Earned premium revenue consisted of premium revenue and capitation revenue for the three and six months ended June 30, 2024 and 2023 were as follows:
| | | | | | | | | | | | | | | | | | | | | | | |
| Three Months Ended
June 30, | | Six Months Ended
June 30, |
| 2024 | | 2023 | | 2024 | | 2023 |
| Premium | $ | 673,532 | | | $ | 424,704 | | | $ | 1,293,254 | | | $ | 824,444 | |
| Capitation | 562 | | | 32,173 | | | 2,396 | | | 67,245 | |
| Total | $ | 674,094 | | | $ | 456,877 | | | $ | 1,295,650 | | | $ | 891,689 | |
Premium revenue is derived monthly from the federal government based on our contracts with the Centers for Medicare and Medicaid Services (“CMS”). In accordance with these arrangements, we assume the responsibility for the outcomes and the economic risk of funding our members’ health care, supplemental benefits and related administration costs. We recognize premium revenue in the month that members are entitled to receive health care services, and premiums collected in advance are deferred. The monthly reimbursement includes a fixed payment per member per month (“PMPM”), which is adjusted based on certain risk factors derived from medical diagnoses and conditions of our members. The adjustments are estimated by projecting the ultimate annual premium and are recognized ratably during the year, with adjustments each period to reflect changes in the estimated ultimate premium. Premiums are also recorded net of estimated uncollectible amounts and retroactive membership adjustments.
Capitation revenue consists primarily of capitated fees for medical care services provided by us under arrangements with third-party payors. In 2023, capitation revenue consisted primarily of revenue from CMS related to our participation in the CMS "ACO Realizing Equity, Access, and Community Health Model” or “ACO REACH” model, as discussed below.
Under those arrangements with third-party payors, we receive a PMPM payment for a defined member population, and we are responsible for providing health care services to the member population over the contract period. We are solely responsible for the cost of health care services related to the member population and in some cases, we are financially responsible for the supplemental benefits provided by us to the members. We act as a principal in arranging for and controlling the services provided by our provider network and we are at risk for arranging and providing health care services.
The premium and capitation payments we receive monthly from CMS for our members are determined from our annual bid or similarly from third-party payors under our capitation arrangement. These payments represent revenues for providing health care coverage, including Medicare Part D benefits. Under the Medicare Part D program, our members and the members of the third-party payors receive standard drug benefits. We may also provide enhanced benefits at our own expense. We recognize premium or capitation revenue for providing this insurance coverage in the month that members are entitled to receive health care services and any premium or capitation collected in advance is deferred. Our CMS payment related to Medicare Part D is subject to risk sharing through the Medicare Part D risk corridor provisions.
We also participate in the CMS ACO REACH program, formerly the Direct Contracting Model ("DCE"). CMS serves as the claim adjudicator for institutional and specialists care, and directly pays for such fee for service claims. The ACO REACH entity ("ACO") is responsible for the cost of health care services related to the patient population attributed to the ACO by participating in 100% savings/losses via the risk share model and in some cases, are financially responsible for the supplemental benefits provided to the patients. In 2024, we entered into a management services and risk management agreement with a third-party healthcare company. The third party will be responsible for arranging and controlling the health care services provided to the ACO members, and for providing certain management and support services with respect to ACO operations. The third party will also assume specified upside and downside financial risk relative to the ACO’s performance. As a result of this arrangement, revenue is recorded on a net basis within other revenue on the condensed consolidated statement of operations for the three and six months ended June 30, 2024. Revenue recognized by the ACO for the three and six months ended June 30, 2024 was $(744) and $241, respectively.
Prior to 2024, the ACO acted as a principal in arranging for and controlling services provided directly by their contracts with primary care physicians, as well as services provided by preferred institutional care providers and specialists. Capitation payments for the ACO program were determined from an annual benchmark established by CMS. These payments, which were adjusted for variable considerations, represented revenue for providing health care services, including primary care as well as institutional and specialist care. The ACO recognized capitation revenue for providing these services in the period in which the performance obligations were satisfied by transferring services to the members. Revenue recognized by the ACO for the three and six months ended June 30, 2023 was $30,113 and $62,227, respectively.
Interest income earned on our cash deposits and short-term investments is included within other revenue on the condensed consolidated statements of operations. Interest income for the three and six months ended June 30, 2024 was $5,602 and $11,045, respectively. Interest income for the three and six months ended June 30, 2023 was $4,727 and $8,444, respectively.
Revenue Adjustments
Payments by CMS to health plans are determined via a competitive bidding process with CMS and are based upon the cost of care in a local market and the average utilization of services by the member enrolled. These payments are subject to periodic adjustments under CMS’ “risk adjustment model,” which compensates health plans based on the health severity and certain demographic factors of each individual member. Members diagnosed with certain conditions are paid at a higher monthly payment than members who are healthier. Under this risk adjustment model, CMS calculates the risk adjustment payment using diagnosis data from hospital inpatient, hospital outpatient, and physician treatment settings. The Company and health care providers collect, capture, and submit the necessary and available diagnosis data to CMS within prescribed deadlines. Both premium and capitation revenues (including Medicare Part D) are subject to adjustments under the risk adjustment model.
Throughout the year, we estimate risk adjustment payments based upon the diagnosis data submitted and expected to be submitted to CMS. Those estimated risk adjustment payments are recorded as an adjustment to premium and capitation revenue. Our risk adjustment data is also subject to review by the government, including audit by regulators.
Our recognized premium revenue for our Medicare Advantage Plans in California, North Carolina, Nevada, Arizona, Texas and Florida are each subject to a minimum annual medical loss ratio (“MLR”) of 85%. The MLR represents medical costs as a percentage of premium revenue. The Code of Federal Regulations defines what constitutes medical costs and premium revenue, including certain additional expenses related to improving the quality of care provided, and the exclusion of certain taxes and fees, in each case as permitted or required by CMS and applicable regulatory requirements. If the minimum MLR is not met, we are required to remit a portion of the premiums back to the federal government. The amount remitted, if any, is recognized as an adjustment to premium revenues in the condensed consolidated statements of operations. The amounts payable under this provision were immaterial at June 30, 2024 and December 31, 2023.
Medicare Part D payments are also subject to a federal risk corridor program, which limits a health plan’s overall losses or profit if actual spending for basic Medicare Part D benefits is much higher or lower than what was anticipated. Risk corridor is recorded within premium revenue. The risk corridor provisions compare costs targeted in our bids or third-party payors’ bids to actual prescription drug costs, limited to actual costs that would have been incurred under the standard coverage as defined by CMS. Variances exceeding certain thresholds may result in CMS or third-party payors making additional payments to us or require us to refund a portion of the premiums we received. We estimate and recognize an adjustment to premium revenue related to these provisions based upon pharmacy claims experience. We record a
receivable or payable at the contract level and classify the amount as current or long-term in our condensed consolidated balance sheet based on the timing of expected settlement.
Variable consideration estimates related to ACO contract revenue are based on the most likely outcome method and that a significant reversal in the amount of cumulative revenue recognized would not occur.
Receivables, including risk adjusted premium due from the government or through third-party payors, pharmacy rebates, and other receivables, are shown net of allowances for credit losses and retroactive membership adjustments.
Property and Equipment—Net
Depreciation expense is computed using the straight-line method generally based on the following estimated useful lives:
| | | | | |
| Description | Estimated Service Lives (years) |
| Computer and equipment | 5 |
| Office equipment and furniture | 5-7 |
| Software | 3-5 |
| Leasehold improvements | 15 (or lease term, if shorter) |
Depreciation expense related to property and equipment used to service our members or at our clinics are included within medical expenses in the condensed consolidated statements of operations.
Medical Expenses
Medical expenses include claim payments, capitation payments, pharmacy costs net of rebates, allocations of certain centralized expenses, internal care delivery expenses and various other costs incurred to provide health insurance coverage and care to members, as well as estimates of future payments to hospitals and others for medical care and other supplemental benefits provided.
We have contracts with a network of hospitals, physicians, and other providers and compensate those providers and ancillary organizations based on contractual arrangements or CMS Medicare compensation guidelines. We pay these contracting providers either through fee-for-service arrangement in which the provider is paid negotiated rates for specific services provided or a capitation payment, which represent monthly contractual fees disbursed for each member regardless of medical services provided to the member. We are responsible for the entirety of the cost of health care services related to the member population, in addition to supplemental benefits provided by us to our seniors. In 2023, we also recorded claims expenses related to our institutional and specialist care related to our ACO program with CMS as we acted as the principal in the transaction. As discussed above, beginning in 2024, claims expense related to the ACO program is netted against ACO revenue as we act as the agent in these transactions.
Capitation-related expenses are recorded on an accrual basis during the coverage period. Expenses related to fee-for-service contracts are recorded in the period in which the related services are dispensed.
Pharmacy costs represent payments for members’ prescription drug benefits, net of rebates from drug manufacturers. Receivables for such pharmacy rebates are included in accounts receivable in the condensed consolidated balance sheet.
In August 2022, the Inflation Reduction Act ("IRA") was signed into law. The law intends to increase tax revenue and reduce Medicare costs through lower prescription drug prices, inflation rebates, and capping annual Medicare Part D out of pocket expenses. The provisions of the law are set to take effect over the next seven years. There was no material impact on our consolidated financial statements at June 30, 2024, and we do not anticipate a material impact to operations for the remainder of fiscal year 2024. We are in the process of evaluating the impact the IRA will have on our business for fiscal years beyond 2024.
Medical Expenses Payable
Medical expenses payable includes estimates of our obligations for medical care services that have been rendered on behalf of our members and the members of the third-party payors, but for which claims have either not yet been received or
processed, loss adjustment expense reserve for the expected costs of settling these claims, and for liabilities related to physician, hospital, and other medical cost disputes.
We develop estimates for medical expenses incurred but not yet paid (“IBNP”), which includes an estimate for claims incurred but not reported (“IBNR”) and a payable for adjudicated claims. IBNR is estimated using an actuarial process that is consistently applied and centrally controlled. Medical expenses payable also includes an estimate for the costs necessary to process unpaid claims at the end of each period. We estimate the IBNR liability using actuarial methods that are commonly used by health insurance actuaries and meet Actuarial Standards of Practice. These actuarial methods consider factors, such as cost trends and completion factors that are assessed based on historical data for payment patterns, product mix, seasonality, utilization of health care services, and other relevant factors. Each period, we re-examine previously established IBNR estimates based on actual claim submissions and other changes in facts and circumstances. As the IBNR estimates recorded in prior periods develop, we adjust the amount of the estimates and include the changes in estimates in medical expenses in the period in which the change is identified.
Actuarial Standards of Practice generally require that the IBNP estimates be adequate to cover obligations under moderately adverse conditions. Moderately adverse conditions are situations in which the actual claims are expected to be higher than the otherwise estimated value of such claims at the time of estimate. In many situations, the claims amount ultimately settled will be different than the estimate that satisfies the Actuarial Standards of Practice. We include in our IBNP an estimate for medical claims liability under moderately adverse conditions, which represents the risk of adverse deviation of the estimates in our actuarial method of reserving. We believe that medical expenses payable is adequate to cover future claims payments required. However, such estimates are based on knowledge of current events and anticipated future events. Therefore, the actual liability could differ materially from the amounts provided.
We reassess the profitability of contracts for providing coverage to members when current operating results or forecasts indicate probable future losses. A premium deficiency reserve is established in current operations to the extent that the sum of expected future costs, claim adjustment expenses, and maintenance costs exceed related future premiums under contracts without consideration of investment income. For purposes of determining premium deficiencies, contracts are grouped in a manner consistent with the method of acquiring, servicing, and measuring the profitability of such contracts. Losses recognized as a premium deficiency result in a beneficial effect in subsequent periods as operating losses under these contracts are charged to the liability previously established.
Part D Subsidies
We also receive advance payments each month from CMS related to Catastrophic Reinsurance, Coverage Gap Discount, and the Low-Income Member Cost Sharing Subsidy (“Subsidies”). Reinsurance subsidies represent funding from CMS for our portion of prescription drug costs, which exceed the member’s out-of-pocket threshold or the catastrophic coverage level. Low-income cost subsidies represent funding from CMS for all or a portion of the deductible, the coinsurance and co-payment amounts above the out-of-pocket threshold for low-income beneficiaries. Additionally, the Health Care Reform Law mandates consumer discounts of 75% on brand-name prescription drugs for Part D plan participants in the coverage gap. The majority of the discounts are funded by the pharmaceutical manufacturers, while we fund a smaller portion and administer the application of the total discount.
These Subsidies represent cost reimbursements under the Medicare Part D program and are recorded as deposits or payables. These Subsidies received in excess of, or less than, actual subsidized benefits paid are refundable to or recoverable from CMS through an annual reconciliation process following the end of the contract year.
Shared Risk Reserve Arrangements
We established a fund (also referred to as “a pool”) for risk and profit-sharing with various independent physician associations (“IPAs”). The pool enables us and our IPAs to share in the financial responsibility and/or upside associated with providing covered medical expenses to our members. The risk pool is based on a contractually agreed upon medical budget, typically based upon a percentage of revenue. If actual medical expenses are less than the budgeted amount, this results in a surplus. Conversely, if actual medical expenses are greater than the budgeted amount, this results in a deficit. We will distribute the surplus, or a portion thereof, to each IPA based upon contractual terms. Deficits are charged to shared risk providers’ risk pool as per the contractual term and evaluated for collectability at each reporting period.
We record risk-sharing receivables and payables on a gross basis on the condensed consolidated balance sheet. Throughout the year, we evaluate expected losses on risk-sharing receivables and record the resulting expected losses to the reserve.
We systematically build and release reserves based on adequacy and its assessment of expected losses on a monthly basis. Credit loss associated with risk share deficit receivables are recorded within medical expense in the condensed consolidated statements of operations. As of June 30, 2024 and December 31, 2023, we recorded a valuation allowance for substantially all of the risk-sharing receivable balance due to collection risk related to the balance. The risk-sharing payable is included within medical expenses payable on the condensed consolidated balance sheet.
Concentrations of Credit Risk
Financial instruments that potentially subject us to concentrations of credit risk consist primarily of cash deposits and current and restricted investments with financial institutions. Accounts at each financial institution are insured by the Federal Deposit Insurance Corporation (“FDIC”) up to certain limits. At June 30, 2024 and December 31, 2023, there was $362,396 and $316,977, respectively, in excess of FDIC-insured limits.
Equity-Based Compensation
Equity-based compensation expense is measured and recognized based on the grant date fair value of the awards. The grant date fair value of stock options is estimated using the Black-Scholes option pricing model. The grant date fair value of restricted stock units (“RSUs”) and restricted stock awards (“RSAs”) is estimated based on the fair value of our underlying common stock on the date of grant.
The Black-Scholes option pricing model requires the use of highly subjective assumptions, including the award’s expected term, the fair value of the underlying common stock, the expected volatility of the price of the common stock, risk-free interest rates, and the expected dividend yield of the common stock. The assumptions used to determine the fair value of the stock-based awards are management’s best estimates and involve inherent uncertainties and the application of judgment. The expected term represents the period the stock-based awards are expected to be outstanding. As we do not have sufficient historical experience for determining the expected term of the stock option awards granted, we utilize the simplified method available under U.S. GAAP. As we do not have a substantial trading history, volatility assumptions were developed using a combination of the Company's historical volatility and the historical volatilities of a set of peer companies, adjusted for debt-equity leverage. Equity-based compensation expense for awards with service-based vesting only is recognized on a graded vesting schedule over the requisite service period of the awards, which is generally four years.
Equity-based compensation expense for RSU awards with performance-based vesting is recognized over the requisite service period on a graded vesting schedule and is only recognized when the Company concludes that it is probable that the performance condition(s) will be achieved. At each reporting period, the Company reassesses the probability of achieving the performance criteria. Determining whether the performance criteria will be achieved involves judgment, and the estimate of share-based compensation expense may be revised periodically based on changes in the probability of achieving the performance criteria. Revisions are reflected in the period in which the estimate is changed. We account for forfeitures as they occur.
Equity-based compensation is recorded within selling, general and administrative expenses, and medical expenses based on the function of the applicable employee and non-employee.
Noncontrolling interest
In October 2022, the Company acquired a subsidiary and recorded a noncontrolling interest for the portion of equity ownership not attributable to Alignment Healthcare, Inc. The noncontrolling interest in the subsidiary was initially recognized at estimated fair value on October 1, 2022 and is presented within total equity in the Company's condensed consolidated balance sheet. The net (income) loss attributable to this noncontrolling interest was $(7) and $47, respectively, for the three and six months ended June 30, 2024. The net loss attributable to this noncontrolling interest was $17 and $104, respectively, for the three and six months ended June 30, 2023.
Net Loss per Share
Net loss per share is calculated based on net loss attributable to Alignment Healthcare, Inc.'s stockholders. The following table sets forth the computation of basic and diluted net loss per share for the three and six months ended June 30, 2024 and 2023:
| | | | | | | | | | | | | | | | | | | | | | | |
| | Three Months Ended
June 30, | | Six Months Ended
June 30, |
| | 2024 | | 2023 | | 2024 | | 2023 |
| Numerator: | | | | | | | |
| Net loss | $ | (24,003) | | | $ | (28,494) | | | $ | (70,578) | | | $ | (65,865) | |
| Less: Net (income) loss attributable to noncontrolling interests | (7) | | | 17 | | | 47 | | | 104 | |
| Net loss attributable to Alignment Healthcare, Inc. | $ | (24,010) | | | $ | (28,477) | | | $ | (70,531) | | | $ | (65,761) | |
| Denominator: | | | | | | | |
| Total weighted-average common shares outstanding - basic and diluted | 191,431,917 | | 188,496,252 | | 190,514,927 | | 188,029,447 |
| Less: Restricted shares of common stock | (540,130) | | (2,504,792) | | (566,202) | | (3,468,795) |
| Total weighted-average common shares outstanding, net of restricted shares of common stock - basic and diluted | 190,891,787 | | 185,991,460 | | 189,948,725 | | 184,560,652 |
| Net loss per share: | | | | | | | |
| Net loss per share - basic and diluted | $ | (0.13) | | | $ | (0.15) | | | $ | (0.37) | | | $ | (0.36) | |
Basic net loss per share is the same as diluted net loss per share for periods presented as the inclusion of all potentially dilutive shares would have been anti-dilutive.
In addition to the restricted shares of common stock, we also excluded the following potential common shares, presented based on amounts outstanding at each period end, from the computation of diluted net loss per share as of June 30, 2024 and 2023:
| | | | | | | | | | | |
| | June 30, |
| | 2024 | | 2023 |
| Stock options | 8,949,589 | | 10,566,529 |
| Restricted stock units | 22,196,478 | | 10,145,593 |
| Total | 31,146,067 | | 20,712,122 |
Recent Accounting Pronouncements Issued
In November 2023, the FASB issued a new accounting standard around segment disclosures. The new standard requires a public entity to disclose significant segment expenses and other segment items on an annual and interim basis and provide, in interim periods, all disclosures about a reportable segment’s profit or loss and assets that are currently required annually. Additionally, it requires a public entity to disclose the title and position of the Chief Operating Decision Maker. The ASU does not change how a public entity identifies its operating segments, aggregates them, or applies the quantitative thresholds to determine its reportable segments. The new standard is effective for fiscal years beginning after December 15, 2023, and interim periods within fiscal years beginning after December 15, 2024, with early adoption permitted. A public entity should apply the amendments in this ASU retrospectively to all prior periods presented in the financial statements. We expect this ASU to only impact our disclosures with no impacts to our results of operations, cash flows and financial condition.
3. Fair Value
The following tables present the carrying value and fair value of these financial instruments as of June 30, 2024 and December 31, 2023:
| | | | | | | | | | | | | | | | | | | | | | | |
| June 30, 2024 |
| | | Fair Value |
| Carrying
Value | | Level 1 | | Level 2 | | Level 3 |
| U.S. Treasury bills | $ | 44,628 | | | $ | 44,577 | | | $ | — | | | $ | — | |
| Certificate of deposits | 2,336 | | | — | | | 2,336 | | | — | |
| Total | $ | 46,964 | | | $ | 44,577 | | | $ | 2,336 | | | $ | — | |
| | | | | | | | | | | | | | | | | | | | | | | |
| December 31, 2023 |
| | | Fair Value |
| Carrying
Value | | Level 1 | | Level 2 | | Level 3 |
| U.S. Treasury bills | $ | 117,337 | | | $ | 117,310 | | | $ | — | | | $ | — | |
| Certificate of deposits | 1,755 | | | — | | | 1,755 | | | — | |
| Total | $ | 119,092 | | | $ | 117,310 | | | $ | 1,755 | | | $ | — | |
The carrying value of long-term debt represents the outstanding balance, net of unamortized debt issuance costs. As of June 30, 2024 and December 31, 2023, the fair value of our long-term debt approximates the carrying value.
Our nonfinancial assets and liabilities, which include goodwill, intangible assets, property, and equipment, are not required to be measured at fair value on a recurring basis. However, on a periodic basis, or whenever events or changes in circumstances indicate that their carrying value may not be recoverable, we assess these assets for impairment. There was no such impairment as of June 30, 2024 and December 31, 2023.
U.S. Treasury Securities Investments
As of June 30, 2024 and December 31, 2023, the Company had $24,651 and $115,914, respectively, of investments in U.S. Treasury bills which were classified as held to maturity and carried at amortized cost. These investments are included in short-term investments in the condensed consolidated balance sheets as the original maturities are greater than three months and less than twelve months. The Company has the intent and ability to hold these securities to maturity and gross unrecognized losses were $0.
As of June 30, 2024 and December 31, 2023, the Company had $18,602 and $22,232, respectively, of investments in U.S. Treasury bill money market funds with an original maturity of less than three months. These investments are considered cash equivalents and are included in cash and cash equivalents in the condensed consolidated balances sheets.
Restricted Investments
Restricted investments are composed of investments in U.S. Treasury bills and certificates of deposits and are included within other assets in the condensed consolidated balance sheets. As of June 30, 2024 and December 31, 2023, the Company had $1,375 and $1,423 of restricted investments in U.S. Treasury bills and $2,336 and $1,755 of restricted investments in certificates of deposits, respectively. The Company has the intent and ability to hold these investments until maturity; therefore, these investments are stated at amortized cost. Restricted investments are required to be maintained at a financial institution within certain states. As of June 30, 2024 and December 31, 2023, these investments had maturities with less than 12 months. Due to the nature of the state's requirements, these assets are classified as noncurrent assets regardless of the contractual maturity date.
4. Accounts Receivable
Accounts receivable consisted of the following as of June 30, 2024 and December 31, 2023:
| | | | | | | | | | | |
| | June 30,
2024 | | December 31,
2023 |
| Government receivables | $ | 78,529 | | | $ | 35,529 | |
| Pharmacy rebate receivables | 94,695 | | | 75,894 | |
| Other receivables | 10,085 | | | 8,326 | |
| Total accounts receivable | 183,309 | | | 119,749 | |
| Allowance for credit losses | (95) | | | — | |
| Accounts receivable, net | $ | 183,214 | | | $ | 119,749 | |
The allowance for expected credit losses for accounts receivable is based primarily on past collections experience relative to the length of time receivables are past due. However, when available evidence reasonably supports an assumption that future economic conditions will differ from current and historical payment collections, an adjustment is reflected in the allowance for expected credit losses. We record pharmacy rebates and other receivables based on contractual terms and expected collections and our estimation process for contractual allowances for such balances generally results in an allowance for balances outstanding greater than 90 days or if expected credit risks are known.
Receivables and any associated allowance are written off only when all collection attempts have failed and such amounts are determined unrecoverable. We regularly review the adequacy of these allowances based on a variety of factors, including age of the outstanding receivable and collection history. When circumstances related to specific collection patterns change, estimates of the recoverability of receivables are adjusted. Because substantially all of our receivable amounts are readily determinable and a large portion of our creditors are governmental authorities, our allowance for credit losses is insignificant.
We recorded a credit loss related to accounts receivable of $95 and $50 during the three months ended June 30, 2024 and 2023, respectively, and $95 and $51 during the six months ended June 30, 2024 and 2023. The amounts were recorded in selling general, and administrative expenses in the condensed consolidated statements of operations.
5. Property and Equipment
Property and equipment consisted of the following as of June 30, 2024 and December 31, 2023:
| | | | | | | | | | | |
| June 30,
2024 | | December 31,
2023 |
| Computers and equipment | $ | 12,235 | | | $ | 11,447 | |
| Office equipment and furniture | 4,397 | | | 4,396 | |
| Software | 165,697 | | | 148,864 | |
| Leasehold improvements | 6,347 | | | 6,347 | |
| Construction in progress | 9,887 | | | 4,532 | |
| Subtotal | 198,563 | | | 175,586 | |
| Less accumulated depreciation | (136,133) | | | (123,685) | |
| Property and equipment-net | $ | 62,430 | | | $ | 51,901 | |
Depreciation expense for the three months ended June 30, 2024 and 2023 was $6,516 and $5,190, respectively, of which $46 and $69, respectively, were included in medical expenses. Depreciation expense for the six months ended June 30, 2024 and 2023 was $12,517 and $10,075, respectively, of which $98 and $130, respectively, were included in medical expenses.
6. Goodwill and Intangible Assets
Intangible assets consisted of the following as of June 30, 2024 and December 31, 2023:
| | | | | | | | | | | | | | | | | | | | | | | |
| June 30, 2024 |
| Gross Carrying Value | | Accumulated Amortization | | Net Carrying Value | | Weighted Average Life |
| Goodwill | $ | 34,826 | | | $ | — | | | $ | 34,826 | | | — |
| License (indefinite lived) | 4,967 | | | — | | | 4,967 | | | — |
| Plan member relationships | 2,700 | | | (2,700) | | | — | | | 9 years |
| Other | 1,050 | | | (816) | | | 234 | | | 2 - 10 years |
| Total | $ | 43,543 | | | $ | (3,516) | | | $ | 40,027 | | | |
| | | | | | | | | | | | | | | | | | | | | | | |
| December 31, 2023 |
| Gross Carrying Value | | Accumulated Amortization | | Net Carrying Value | | Weighted Average Life |
| Goodwill | $ | 34,826 | | | $ | — | | | $ | 34,826 | | | — |
| License (indefinite lived) | 4,967 | | | — | | | 4,967 | | | — |
| Plan member relationships | 2,700 | | | (2,700) | | | — | | | 9 years |
| Other | 1,050 | | | (765) | | | 285 | | | 2 - 10 years |
| Total | $ | 43,543 | | | $ | (3,465) | | | $ | 40,078 | | | |
Amortization expense relating to intangible assets for the three months ended June 30, 2024 and 2023, was $23 and $74, respectively. Amortization expense relating to intangible assets for the six months ended June 30, 2024 and 2023, $51 and $171, respectively. Estimated amortization expense relating to intangible assets for each of the next five years ending December 31, is as follows:
| | | | | |
| Remainder of 2024 | $ | 31 | |
| 2025 | 60 | |
| 2026 | 60 | |
| 2027 | 60 | |
| 2028 | 23 | |
| |
| $ | 234 | |
There were no impairment charges related to goodwill and intangible assets for the three and six months ended June 30, 2024 and 2023.
7. Medical Expenses Payable
The following table is a detail of medical expenses payable as of June 30, 2024 and December 31, 2023:
| | | | | | | | | | | |
| | June 30,
2024 | | December 31,
2023 |
| Claims incurred but not paid | $ | 156,379 | | | $ | 95,664 | |
| Capitation and risk-sharing payable | 69,316 | | | 50,894 | |
| Other | 89,674 | | | 58,841 | |
| Medical expenses payable | $ | 315,369 | | | $ | 205,399 | |
Each period, we re-examine previously established outstanding claims reserve estimates based on actual claims submissions and other changes in facts and circumstances. As more complete claim information becomes available, we adjust the amount of the estimates and include the changes in estimates in claim costs in the period in which the change is
identified. Substantially, all of the total claims paid by us are known and settled within the first year from the date of service, and substantially, all remaining claim amounts are paid within a three-year period.
The following table presents components of the change in medical expenses payable as of June 30, 2024 and 2023:
| | | | | | | | | | | |
| June 30,
2024 | | June 30,
2023 |
| Claims incurred but not paid - beginning balance | $ | 95,664 | | | $ | 88,813 | |
| Incurred related to: | | | |
| Current year | 407,156 | | | 235,027 | |
| Prior years | (7,257) | | | (7,168) | |
| Total incurred, net of reinsurance | 399,899 | | | 227,859 | |
| Payments related to: | | | |
| Current year | 263,824 | | | 156,152 | |
| Prior years | 75,360 | | | 68,632 | |
| Total payments, net of reinsurance | 339,184 | | | 224,784 | |
| Claims incurred but not paid - ending balance | 156,379 | | | 91,888 | |
| Capitation payable, risk-sharing payable, and other | 158,990 | | | 115,310 | |
| Total medical expenses payable | $ | 315,369 | | | $ | 207,198 | |
We re-examine previously established outstanding claims reserve estimates based on actual claims submissions and other changes in facts and circumstances. We recognized a favorable prior year development, excluding provision for adverse deviation, of $2,460 and $3,331 for the three and six months ended June 30, 2024. The favorable prior year development was primarily due to better-than-expected claims recoveries and actual claims expense being less than expected.
8. Long-Term Debt
Long-term debt is recorded at carrying value in the condensed consolidated balance sheets. The carrying value of long-term debt outstanding, net of unamortized debt issuance costs, consisted of the following as of June 30, 2024 and December 31, 2023:
| | | | | | | | | | | |
| June 30,
2024 | | December 31,
2023 |
| Long-term debt | $ | 215,000 | | | $ | 165,000 | |
| Less unamortized debt issuance costs | (3,258) | | | (3,187) | |
| Long-term debt-net of amortization | 211,742 | | | 161,813 | |
| Less current portion of long-term debt | — | | | — | |
| Long-term debt - net of current portion | $ | 211,742 | | | $ | 161,813 | |
Oxford Term Loan
On September 2, 2022 (the "Effective Date"), Alignment Healthcare USA, LLC entered into a senior secured term loan agreement (the “Oxford Loan Agreement”) with Oxford Finance LLC (“Oxford”), as administrative agent, collateral agent and a lender, and the other lenders from time to time party thereto (collectively, the “Lenders”), pursuant to which the Lenders have agreed to lend an aggregate principal amount of up to $250,000 in a series of term loans (the “Term Loans”). Pursuant to the Oxford Loan Agreement, we received an initial Term Loan of $165,000 on the Effective Date and had the option to borrow up to an additional $85,000 of Term Loans (such additional Term Loans, the “Delayed Draw Term Loans”). On June 14, 2024, we borrowed $50,000 in aggregate principal amount of the Delayed Draw Term Loans prior to the expiration date for such amount of the Delayed Draw Term Loans of June 30, 2024. As of June 30, 2024 we have the option to borrow an additional $35,000 in undrawn Delayed Draw Term Loans, which expires on September 1, 2025.
Interest on the Term Loans is a variable rate equal to (i) the secured overnight financing rate ("SOFR") administered by the Federal Reserve Bank of New York for a one-month tenor, subject to a floor of 1.00%, plus (ii) an applicable margin of
6.50%. All unpaid principal and accrued and unpaid interest with respect to each Term Loan is due and payable in full on September 1, 2027. The interest rate applied during the six months ended June 30, 2024 ranged from 11.82% to 11.85%.
The initial Term Loan was subject to a commitment fee of $1,650 and an origination fee of $1,650. The Delayed Draw Term Loans are subject to a commitment fee of $850. We incurred additional debt issuance costs of $1,096 related to attorney fees and other third-party costs. We also incurred an origination fee of $500 related to the $50,000 draw down of the Delayed Draw Term Loans. The commitment and origination fees are included within debt issuance costs and were deferred and will be amortized to interest expense over the debt term using the straight line method, which is materially consistent with the effective interest method. The debt issuance costs related to the initial Term Loan are presented in the condensed consolidated balance sheet as a direct deduction from the carrying value of the term loan. The debt issuance costs related to the Delayed Draw Term Loan are presented in the condensed consolidated balance sheet as other assets.
The Term Loans are jointly and severally guaranteed by Alignment Healthcare, Inc. and certain of our wholly owned subsidiaries and collateralized by all unrestricted assets.
For certain prepayments of the Term Loans prior to the second anniversary of the Effective Date, we will be required to pay a prepayment fee of 1.00% of the principal amount of the Term Loans being prepaid.
The Oxford Loan Agreement includes customary events of default, including, among others, payment defaults, breach of representations and warranties, covenant defaults, judgment defaults, insolvency and bankruptcy defaults, and change of control. The occurrence of an event of default could result in the acceleration of the obligations under the Oxford Loan Agreement, termination of the Term Loan commitments and the right to foreclose on the collateral securing the obligations. During the existence of an event of default, the outstanding Term Loans will accrue interest at a rate per annum equal to 2.00% plus the otherwise applicable interest rate. Additionally, in the event of any contemplated asset sale or series of asset sales yielding net proceeds in excess of $2,500, except those excluded per the Oxford Loan Agreement, we are required to prepay the aggregate outstanding principal balance of the Term Loans in an amount equal to the entire amount of the asset sale net proceeds, plus any accrued and unpaid interest.
The Oxford Loan Agreement includes financial covenants that require the Borrower Parties to (i) maintain minimum liquidity, as defined in the Loan Agreement, of $23,000 and (ii) satisfy a maximum permitted ratio of debt to trailing twelve-month revenue, as set forth in the Loan Agreement. As of June 30, 2024 and December 31, 2023, we were in compliance with the Oxford financial covenants.
Future maturities under the term loan for each of the next five years ending December 31, are as follows:
| | | | | |
| Amount |
| Remainder of 2024 | $ | — | |
| 2025 | 2,150 | |
| 2026 | 2,150 | |
| 2027 | 210,700 | |
| 2028 | — | |
| $ | 215,000 | |
9. Income Taxes
For the three and six months ended June 30, 2024, we recorded income tax expense of $22 and $22, respectively. For the three and six months ended June 30, 2023, we recorded income tax expense of $1 and $2, respectively. The increase in tax for the three and six months ended June 30, 2024 when compared to the three and six months ended June 30, 2023, is primarily attributable to an increase in state taxes. Our future effective tax rate may vary from the statutory tax rate primarily due to changes in our valuation allowance, state taxes, and excess executive compensation.
We have federal and state cumulative net operating losses ("NOLs") as of June 30, 2024 and December 31, 2023. Given the history of losses, and after consideration for the risk associated with estimates of future taxable income, we established a full valuation allowance against net deferred tax assets at June 30, 2024 and 2023. Under the Tax Cuts and Jobs Act (“TCJA”), federal NOLs generated after 2017 will be carried forward indefinitely but are limited to an 80% deduction of taxable income. NOLs generated prior to 2018 have a 20-year carryforward period and can be used to offset 100% of
taxable income. An exception to the TCJA federal NOL rule applies to certain of our subsidiaries and requires all NOLs generated from those entities to have a 20-year carryforward period and offset 100% of taxable income. For the year ended December 31, 2023 federal and state NOL carryforwards were $504,097 and $498,933, respectively. $312,446 of the total federal net operating loss carryforwards have an indefinite life while the remaining federal and state net operating loss carryforwards begin to expire in 2033 if not utilized. On June 27, 2024, California Senate Bill 167 (“SB 167”) was enacted into law, suspending California NOL utilization for taxpayers with more than $1 million of taxable income, effective for tax years 2024, 2025, and 2026. SB 167 includes an extended carryover period for the suspended NOLs with an additional year carryforward for each year of suspension. The Company will continue to monitor this legislation and its impact on our deferred tax assets.
An “ownership change” as defined under Section 382 of the Internal Revenue Code ("IRC"), could potentially limit the ability to utilize certain tax attributes including the Company’s substantial NOLs. Ownership change is generally defined as any significant change in ownership of more than 50% of its stock over a three-year testing period. If, as a result of current or future transactions involving our common stock, we undergo cumulative ownership changes which exceed 50% over a testing period, our ability to utilize our NOL carryforwards would be subject to additional limitations under IRC Section 382. We continue to monitor changes in ownership with respect to these income tax provisions.
10. Equity-Based Compensation
Equity Awards
Stock Options
Our outstanding stock options generally vest 25% annually over four years and generally expire 10 years from the date of the grant. The 2021 Equity Incentive Plan provides that stock option grants will be made with an exercise price at no less than the estimated fair value of common stock at the date of the grant.
The following is a summary of the stock option transactions as of and for the three and six months ended June 30, 2024:
| | | | | | | | | | | | | | | | | | | | | | | |
| | Stock Options Outstanding |
| (amounts in thousands, except shares and per share amount) | Shares Subject to Options Outstanding | | Weighted- Average Exercise Price per Option | | Weighted- Average Remaining Contractual Terms (in years) | | Aggregate Intrinsic Value |
| Balances as of December 31, 2023 | 9,135,879 | | $ | 16.95 | | | 7.29 | | $ | 79 | |
| Options granted | — | | — | | | | | |
| Options exercised | — | | — | | | | | |
| Options forfeited / expired | (112,536) | | 15.41 | | | | | |
| Balances as of March 31, 2024 | 9,023,343 | | $ | 16.97 | | | 7.04 | | — | |
| Options granted | — | | — | | | | | |
| Options exercised | — | | — | | | | | |
| Options forfeited / expired | (73,754) | | 16.62 | | | | | |
| Balances as of June 30, 2024 | 8,949,589 | | $ | 16.97 | | | 6.79 | | $ | 27 | |
| Vested and Exercisable as of June 30, 2024 | 6,297,452 | | $ | 17.28 | | | 6.75 | | $ | 14 | |
| | | | | | | |
| | | | | | | |
| | | | | | | |
| | | | | | | |
| | | | | | | |
Aggregate intrinsic value represents the difference between the exercise price of the option and the closing price of our common stock. For the three and six months ended June 30, 2024 and 2023, no options were exercised. No options were granted during the three and six months ended June 30, 2024.
Restricted Stock Awards
Our outstanding Restricted Stock Awards ("RSA") generally vest 25% annually over four years. RSAs converted from pre-IPO awards generally vest on the later of the fourth anniversary of the original vesting commencement date or 50% annually on the first and second anniversary of the IPO.
The following is a summary of RSA transactions for the three and six months ended June 30, 2024:
| | | | | | | | | | | |
| | Restricted Shares | | Weighted-Average Grant Date Fair Value |
| Unvested and outstanding as of December 31, 2023 | 683,953 | | $ | 5.86 | |
| Vested | (140,856) | | 13.22 | |
| Forfeited | (2,799) | | 5.05 | |
| Unvested and outstanding as of March 31, 2024 | 540,298 | | $ | 3.94 | |
| Vested | (3,056) | | 2.49 | |
| Forfeited | — | | — | |
| Unvested and outstanding as of June 30, 2024 | 537,242 | | $ | 3.95 | |
| | | |
| | | |
| | | |
Restricted Stock Units
Our outstanding Restricted Stock Units ("RSU") generally vest 25% annually over four years.
The following is a summary of RSU transactions as of and for the three and six months ended June 30, 2024:
| | | | | | | | | | | |
| | Restricted Stock Units | | Weighted-Average Grant Date Fair Value |
| Unvested and outstanding as of December 31, 2023 | 10,541,625 | | $ | 11.25 | |
| Granted | 6,517,337 | | 5.05 |
Vested(1) | (2,385,493) | | 8.25 |
| Cancelled/forfeited | (282,972) | | 9.36 |
| Unvested and outstanding as of March 31, 2024 | 14,390,497 | | $ | 8.97 | |
| Granted | 103,292 | | 5.62 |
| Vested | (80,178) | | 6.07 |
| Cancelled/forfeited | (395,338) | | 8.40 |
| Unvested and outstanding as of June 30, 2024 | 14,018,273 | | $ | 8.98 | |
| | | |
| | | |
| | | |
| | | |
(1) Includes 107,948 shares that vested, but the issuance and delivery of the shares was deferred.
Performance-based Restricted Stock Units ("PSUs")
On September 14, 2023, the Board of Directors of the Company approved the grant of performance-based restricted stock units under the Company's 2021 Equity Incentive Plan to its executive management team and other key employees. Each grantee is eligible to vest in a number of PSUs ranging from 0% to 150% of the target number of PSUs granted, based on the aggregated achievement by the Company of certain performance metrics during the performance period beginning on January 1, 2024 and ending on December 31, 2024. The achievement of PSUs relative to the approved target is based on the following performance metrics and relative weighting: Health Plan Revenue Growth Percentage 60%, At-Risk Returning Member Medical Benefit Ratio 20% and Adjusted EBITDA, less Capital Expenditures 20%.
50% of the total number of earned PSUs will become vested upon certification of achievement of the performance metrics by the Compensation Committee on or about March 1, 2025 and the remaining 50% of earned PSUs will be become vested as of December 31, 2025, subject to continued service to the Company through such dates.
On March 13, 2024, the Compensation Committee of the Board of Directors of the Company approved additional grants of PSUs under the Company's 2021 Equity Incentive Plan. Each grantee is eligible to vest in a number of PSUs ranging from 0% to 200% of the target number of PSUs granted, based on the aggregated achievement by the Company of certain performance metrics during the performance period beginning on January 1, 2024 and ending on December 31, 2026. The achievement of PSUs relative to the approved target is based on the following performance metrics and relative weighting: Revenue 50% and Adjusted EBITDA 50%. 100% of the total number of earned PSUs will become vested upon
certification of achievement of the performance metrics by the Compensation Committee on or about March 1, 2027, subject to continued service to the Company through such date.
The following is a summary of PSU transactions for the three and six months ended June 30, 2024:
| | | | | | | | | | | |
| | Performance-based restricted stock units | | Weighted-Average Grant Date Fair Value |
| Unvested and outstanding as of December 31, 2023 | 7,233,205 | | $ | 5.74 | |
| Granted | 1,160,000 | | 5.00 | |
| Vested | — | | — | |
| Cancelled/forfeited | (16,667) | | 5.74 | |
| Unvested and outstanding as of March 31, 2024 | 8,376,538 | | $ | 5.64 | |
| Granted | — | | — | |
| Vested | — | | — | |
| Cancelled/forfeited | (198,333) | | 5.67 | |
| Unvested and outstanding as of June 30, 2024 | 8,178,205 | | $ | 5.64 | |
Equity-Based Compensation Expense
Total equity-based compensation expense was presented on the statement of operations as follows:
| | | | | | | | | | | | | | | | | | | | | | | |
| | Three Months Ended June 30, | | Six Months Ended June 30, |
| (amounts in thousands) | 2024 | | 2023 | | 2024 | | 2023 |
| Selling, general and administrative expenses | $ | 16,022 | | | $ | 13,869 | | | $ | 35,743 | | | $ | 33,323 | |
| Medical expenses | 762 | | | 1,767 | | | 1,895 | | | 4,291 | |
| Total equity-based compensation expense | $ | 16,784 | | | $ | 15,636 | | | $ | 37,638 | | | $ | 37,614 | |
As of June 30, 2024, there was $93,667 in unrecognized compensation expense related to all non-vested awards (RSAs, options, RSUs and PSUs) that will be recognized over the weighted-average period of 1.70 years.
11. Regulatory Requirements and Restricted Funds
Our health plans or risk-bearing entities are required to maintain minimum capital requirements prescribed by various regulatory authorities in each of the states in which it operates.
Risk-Based Capital Regulatory
The National Association of Insurance Commissioners has adopted rules, which, if implemented by the states, set minimum capitalization requirements for insurance companies, health maintenance organizations ("HMOs"), and other entities bearing risk for health care coverage. The requirements take the form of risk-based capital (“RBC”) rules, which may vary from state to state. Certain states in which our health plans or risk bearing entities operate have adopted the RBC rules. Our health plans or risk-bearing entities were in compliance with the minimum capital requirements as of June 30, 2024.
Tangible Net Equity
Our health plan in California is required to comply with the tangible net equity (“TNE”) requirements. The required amount is the larger of: (1) $1,000; (2) 2% of the first $150,000 of annualized premium revenue, plus 1% of annualized premium revenue in excess of $150,000; or (3) 8% of the first $150,000 of annualized health care expenditures, except for those paid on a capitated or managed hospital payment basis, plus 4% of the annualized health care expenditures in excess of $150,000, except those paid on a capitated or managed hospital payment basis, plus 4% of annualized hospital expenditures paid on a managed hospital payment basis. We were in compliance with the TNE requirement as of June 30, 2024.
We have the ability to provide additional capital to each of our health plans or risk-bearing entities when necessary to ensure that the RBC and TNE requirements are met.
Certain states regulate the payment of dividends, loans, or other cash transfers from our regulated subsidiaries to our non-regulated subsidiaries and parent company. Such payments may require approval by state regulatory authorities and are limited based on certain financial criteria, such as the entity’s level of statutory income and statutory capital and surplus, or the entity’s level of tangible net equity or net worth, amongst other measures. These regulations vary by state. We were in compliance with the RBC and TNE requirements as of June 30, 2024.
Restricted Assets
Pursuant to the regulations governing our subsidiaries, we maintain certain deposits required by the government authorities in the form of cash, certificate of deposit and Treasury bills as protection in the event of insolvency. The use of funds from these investments is limited as required by regulation in the various states in which we operate, or as needed in the event of insolvency. Therefore, these deposits are reported within other assets on the condensed consolidated balance sheets.
We hold these assets until maturity, at which time these assets will renew or are invested in a similar type of investment instrument. Given the regulatory requirements, we expect to hold these investments for long-term. As a result, we do not expect the value of these investments to decline significantly due to a sudden change in market interest rates. These investments are carried at amortized cost, which approximates fair value. See note 3, Fair Value, for further discussion.
12. Commitments and Contingencies
Legal Proceedings
We record a liability and accrue the costs for a loss when an unfavorable outcome is probable and the amount of the loss can be reasonably estimated. In some cases, no estimate of the possible loss or range of loss in excess of amounts accrued, if any, can be made because of the inherently unpredictable nature of legal and regulatory proceedings. While the liability and accrued costs reflect our best estimate, the actual amounts may materially be different.
On April 27, 2022, a former employee of the Company filed a purported class action lawsuit (Dabney v. Alignment Healthcare USA, LLC, Orange County Superior Court) alleging that the Company failed to provide hourly employees with required meal and rest breaks or pay such workers a premium equal to an hour of pay for missed meal or rest breaks. Discovery in the matter commenced on June 8, 2022. On September 2, 2022, the court granted a stay of proceedings and discovery in anticipation of mediation scheduled for August 2023. On August 15, 2023, the Company entered into a tentative settlement of the action in consideration of an aggregate payment of $913. The settlement of this matter is subject to approval by the court which is expected in the third quarter of 2024. As a result of the tentative settlement, the Company has accrued for a potential liability of $913 as of June 30, 2024 and December 31, 2023 for this matter, which was recorded within accounts payable and accrued expenses on the consolidated balance sheet and selling, general and administrative expenses on the consolidated statement of operations.
We may be involved in various litigation matters in the ordinary course of business. In the opinion of management, the ultimate resolution of legal proceedings is not expected to have a material adverse effect on the condensed consolidated financial statements. Amounts accrued for legal proceedings were not material as of June 30, 2024 and December 31, 2023.
Item 2. Management’s Discussion and Analysis of Financial Condition and Results of Operations.
MANAGEMENT’S DISCUSSION AND ANALYSIS OF
FINANCIAL CONDITION AND RESULTS OF OPERATIONS
The following discussion and analysis should be read in conjunction with our audited financial statements and the accompanying notes as well as “Risk Factors” and “Management’s Discussion and Analysis of Financial Condition and Results of Operations” included in our Annual Report on Form 10-K for the year ended December 31, 2023 (our "Annual Report"), as well as our unaudited condensed consolidated financial statements and related notes presented herein in Part I, Item 1 included elsewhere in this Quarterly Report. Unless the context otherwise indicates or requires, the terms “we”, “our” and the “Company” as used herein refer to Alignment Healthcare, Inc. and its consolidated subsidiaries, including Alignment Healthcare Holdings, LLC, which is Alignment Healthcare, Inc.’s predecessor for financial reporting purposes.
In addition to historical data, the discussion contains forward-looking statements about the business, operations and financial performance of the Company based on our current expectations that involves risks, uncertainties and assumptions. Actual results could differ materially from those discussed in or implied by forward-looking statements as a result of various factors, including those discussed above in "Forward-Looking Statements," and Part II, Item 1A, "Risk Factors.”
Overview
Alignment is a next generation, consumer-centric platform designed to improve the healthcare experience for seniors. We deliver this experience through our Medicare Advantage plans, which are customized to meet the needs of a diverse array of seniors. Our innovative model of consumer-centric healthcare is purpose-built to provide seniors with care as it should be: high quality, low cost and accompanied by a vastly improved consumer experience. We combine a proprietary technology platform and a high-touch clinical model that enhances our members’ lifestyles and health outcomes while simultaneously controlling costs, which allows us to reinvest savings back into our platform and products to directly benefit the senior consumer. We have grown Health Plan Membership, which we define as members enrolled in our health maintenance organization ("HMO") and preferred provider organization ("PPO") contracts (the "Alignment Health Plans"), from approximately 13,000 at inception to 175,100 as of June 30, 2024, representing a 30% compound annual growth rate across 53 markets and 6 states. Our ultimate goal is to bring this differentiated, advocacy-driven healthcare experience to millions of senior consumers in the United States and to become the most trusted senior healthcare brand in the country.
Our model is based on a flywheel concept, referred to as our “virtuous cycle,” which is designed to delight our senior consumers. We start by listening to and engaging with our seniors in order to provide a superior experience in both their healthcare and daily living needs. Through our proprietary technology platform, Alignment's Virtual Application ("AVA"), we utilize data and predictive algorithms that are specifically designed to ensure personalized care is delivered to each member. When our information-enabled care model is combined with our member engagement, we are able to improve healthcare outcomes by, for example, reducing unnecessary hospital admissions, which in turn lowers overall costs. Our ability to manage healthcare expenditures while maintaining quality and member satisfaction is a distinct and sustainable competitive advantage. Our lower total healthcare expenditures allow us to reinvest our savings into richer coverage and benefits, which propels our growth in revenue and membership due to the enhanced consumer value proposition. As we grow, we continue to listen to and incorporate member feedback, and we are able to further enhance benefits and produce strong clinical outcomes. Our virtuous cycle, based on the principle of doing well by doing good, is highly repeatable and a core tenet of our ability to continue to expand in existing and new markets in the future.
For the 2024 plan year, Alignment offers plans in 53 markets across California (22 markets), North Carolina (16 markets), Nevada (6 markets), Arizona (3 markets), Texas (2 markets) and Florida (4 markets). There are approximately 8.7 million Medicare-eligible seniors in our current markets.
Factors Affecting Our Performance
Our proprietary technology platform, AVA, is a key element of our business with capabilities that we expect to impact our future performance. AVA enables us to personalize and manage our member relationships, care quality and experience, and to coordinate and manage risk with our provider partners. AVA’s unified platform, analytical tools and data across the healthcare ecosystem enable us to produce consistent outcomes, unit economics and support new member growth.
Additionally, our historical financial performance has been, and we expect our financial performance in the future will be, driven by our ability to:
•Capitalize on Our Existing Market Growth Opportunity: Our ability to attract and retain members to grow in our existing markets depends on our ability to offer a superior value proposition. We have proven that we can compete against, and take market share from, large established players in highly competitive markets. According to CMS data, we were one of the top three Medicare Advantage Organizations in terms of HMO net members growth in our California counties between 2016 and 2024. There are approximately 4.7 million Medicare-eligible individuals enrolled in Medicare Advantage plans in our existing 53 counties, of which our approximately 175,100 Health Plan Members represent only 4% market share. We believe that there are still significant opportunities for future growth even in our most mature markets where we have a 10-35% market share. Additionally, we are evaluating other opportunities to leverage our historical investments in our technology platform and our comprehensive clinical model across our existing and potentially new geographies.
•Drive Growth and Consistent Outcomes Through New Market Expansion: We enter new markets with the goal of building brand awareness across our key stakeholders to achieve meaningful market share over time. We intend to focus on markets with significant senior populations where we expect to be able to replicate our model most effectively. Our existing markets also feature a diverse array of membership profiles across ethnicities, income levels and acuity. In 2023 we expanded into 14 new markets across our four existing states and two new states, Florida and Texas, and in 2024, we expanded into one new market in California.
•Provide Superior Service, Care and Consumer Satisfaction: We are highly focused on providing superior service and care to our members and on maintaining high levels of consumer satisfaction, which are key to our financial performance and growth. The CMS Five Star Quality Rating System provides economic incentives to Medicare Advantage plans that achieve higher Star ratings by (i) meeting certain care criteria (such as completing particular preventative screening procedures or ensuring proper follow-up care is provided for specific conditions or episodes) and (ii) receiving high member satisfaction ratings. These incentives impact financial performance in the year following the CMS Rating Year (for example, CMS’s announcement of the 2024 Ratings occurred in the second half of 2023 and will impact our financial performance in 2025). In aggregate, more than 90% of our health plan members are enrolled in plans rated 4 stars and above, meaning the vast majority of members consistently receive a high-quality care experience, as defined under CMS star measurement criteria. Additionally, the California HMO plan has achieved a 4-star or greater rating for seven consecutive years.
•Effectively Manage the Quality of Care to Improve Member Outcomes: Our care delivery model is based on a clinical continuum through which we have created a highly personalized experience that is unique to each member depending on their personal health and circumstances. Utilizing data and predictive analytics generated by AVA, our clinical continuum separates seniors into four categories in order to provide optimized care for every stage of a senior’s life: healthy, healthy utilizer, pre-chronic and chronic. We partner with our broader network of community providers to service members in our non-chronic categories, and we have developed a Care Anywhere program implemented by our internal clinical teams to care for our higher risk and/or chronically ill members. By investing in our members’ care proactively, our model has consistently reduced unnecessary and costly care while improving the quality of our members’ lifestyle and healthcare experience. By delivering superior care and preventing avoidable utilization of the healthcare system, we are able to reduce our claims expenditures in some of our largest medical expense categories, which translates to superior medical benefits ratio (“MBR”) financial performance and ultimately the ability to offer richer products in the market.
•Achieve Superior Unit Economics: As our senior population ages, their healthcare needs become more frequent and complex. To combat the healthcare cost increases that typically result, we proactively look to (i) connect with our population early in their enrollment with Alignment to assess their care needs, (ii) develop care plans and engage those members with more chronic, complex health challenges in our clinical model, and (iii) continue to monitor and evaluate our healthier members in a preventative fashion over time. Given the Medicare Advantage payment mechanism and the retention of the vast majority of our members who continue to choose Alignment after their initial selection year, we are able to focus our efforts on driving favorable long-term health outcomes for our entire population. As a result, our clinical
model efforts have demonstrated the ability to lower the MBRs of our returning members. We believe this is evidence of our ability to manage the financial risk of our members as they age, and that these favorable underlying unit economic trends translate directly to our ability to continue to deliver a richer product to the marketplace. With this dynamic in mind, our consolidated MBR may be impacted year-to-year based on our pace of new member growth and mix of members by cohort. However, we believe our ability to sustain MBR performance improvement over time positions us well to invest in new member growth to drive long-term financial performance.
•Invest in our Platform and Growth: We plan to continue to invest in our business in order to further develop our AVA platform, pursue new expansion opportunities and create innovative product offerings. In addition, in order to maintain a differentiated value proposition for our members, we continue to invest in innovative product offerings and supplementary benefits to meet the evolving needs of the senior consumer. We anticipate further investments in our business as we expand into new markets and pursue strategic acquisitions, which we expect will primarily be focused on healthcare delivery groups in key geographies, standalone and provider-sponsored Medicare Advantage plans and other complementary risk bearing assets.
•Navigate Seasonality to our Business: Our operational and financial results will experience some variability depending upon the time of year in which they are measured. We experience the largest portion of member growth during the first quarter, when plan enrollment selections made during the annual enrollment period ("AEP") from October 15th through December 7th of the prior year take effect. As a result, we expect to see a majority of our member growth occur on January 1 of a given calendar year. As the year progresses, our per-member revenue often declines as new members join us, typically with less complete or accurate documentation (and therefore lower risk-adjustment scores), and senior mortality disproportionately impacts our higher-acuity (and therefore greater revenue) members. Medical costs will vary seasonally depending on a number of factors, but most significantly the weather. Certain illnesses, such as the influenza virus, are far more prevalent during colder months of the year, which will result in an increase in medical expenses during these time periods. We therefore expect to see higher levels of per-member medical costs in the first and fourth quarters. The design of our prescription drug coverage (Medicare Part D) results in coverage that varies as a member’s cumulative out-of-pocket costs pass through successive stages of a member’s plan period, which begins annually on January 1 for renewals. These plan designs generally result in us sharing a greater portion of the responsibility for total prescription drug costs in the early stages of the year and less in the latter stages, which typically results in a higher MBR on our Part D program in the first half of the year relative to the second half of the year. In addition, we expect our corporate, general and administrative expenses to increase in absolute dollars for the foreseeable future to support our growth and because of additional costs of being a public company. Due to the timing of many of these investments, including our primary sales and marketing season, we typically incur a greater level of investment in the second half of the year relative to the first half of the year.
Executive Summary
The following table presents key financial statistics for the periods indicated:
| | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | |
| | Three Months Ended June 30, | | | | Six Months Ended June 30, | | |
| (dollars in '000's, except percentages) | 2024 | | 2023 | | % Change | | 2024 | | 2023 | | % Change |
| Health plan membership (at period end) | 175,100 | | 112,200 | | 56.1 | % | | 175,100 | | 112,200 | | 56.1 | % |
| Medical benefits ratio | 88.7 | % | | 88.4 | % | | 0.3 | % | | 89.8 | % | | 89.0 | % | | 0.8 | % |
| Revenues | $ | 681,286 | | $ | 462,379 | | | 47.3 | % | | $ | 1,309,887 | | | $ | 901,534 | | | 45.3 | % |
| Loss from Operations | $ | (18,382) | | $ | (23,659) | | | 22.3 | % | | $ | (59,488) | | | $ | (56,148) | | | (5.9) | % |
| Net loss | $ | (24,003) | | $ | (28,494) | | | 15.8 | % | | $ | (70,578) | | | $ | (65,865) | | | (7.2) | % |
Adjusted EBITDA(1) | $ | 6,034 | | $ | (2,055) | | | 393.6 | % | | $ | (5,946) | | | $ | (7,227) | | | 17.7 | % |
Adjusted gross profit (1) | $ | 76,803 | | $ | 53,571 | | | 43.4 | % | | $ | 134,146 | | | $ | 98,996 | | | 35.5 | % |
(1)See "Adjusted EBITDA" and "Adjusted Gross Profit" below for a reconciliation to the most directly comparable financial measure calculated in accordance with GAAP and related disclosures.
Health Plan Membership
We define Health Plan Membership as the number of members enrolled in our HMO and PPO contracts as of the end of a reporting period. We believe this is an important metric to assess growth of our underlying business, which is indicative of our ability to consistently offer a superior value proposition to seniors. This metric excludes third party payor members with respect to which we are at-risk for managing their healthcare expenditures, which represented 400 members as of June 30, 2024 and 2023. It also excludes the approximately 8,600 and 7,600 ACO REACH members as of June 30, 2024 and 2023, respectively.
Adjusted Gross Profit and Medical Benefits Ratio
Adjusted gross profit is a non-GAAP financial measure that we define as loss from operations before depreciation and amortization, clinical equity-based compensation expense, clinical restructuring costs and selling, general, and administrative expenses. Adjusted gross profit is a key measure used by our management and Board to understand and evaluate our operating performance and trends before the impact of our consolidated selling, general and administrative expenses.
Adjusted gross profit should not be considered in isolation of, or as an alternative to, measures prepared in accordance with GAAP. There are a number of limitations related to the use of adjusted gross profit in lieu of loss from operations, which is the most directly comparable financial measure calculated in accordance with GAAP.
Our use of the term adjusted gross profit may vary from the use of similar terms by other companies in our industry and accordingly may not be comparable to similarly titled measures used by other companies.
Adjusted gross profit is reconciled as follows:
| | | | | | | | | | | | | | | | | | | | | | | |
| | Three Months Ended June 30, | | Six Months Ended June 30, |
| | 2024 | | 2023 | | 2024 | | 2023 |
| (dollars in thousands) | | | | | | | |
| Loss from operations | $ | (18,382) | | | $ | (23,659) | | | $ | (59,488) | | | $ | (56,148) | |
| Add back: | | | | | | | |
| Equity-based compensation (medical expenses) | 762 | | | 1,767 | | | 1,895 | | | 4,291 | |
| Depreciation (medical expenses) | 46 | | | 69 | | | 98 | | | 130 | |
Restructuring costs (medical expenses)(1) | 21 | | | — | | | 796 | | | — | |
| Depreciation and amortization | 6,493 | | | 5,195 | | | 12,470 | | | 10,116 | |
| Selling, general, and administrative expenses | 87,863 | | | 70,199 | | | 178,375 | | | 140,607 | |
| Total add back | 95,185 | | | 77,230 | | | 193,634 | | | 155,144 | |
| Adjusted gross profit | $ | 76,803 | | | $ | 53,571 | | | $ | 134,146 | | | $ | 98,996 | |
(1)Represents severance and related costs incurred as part of a corporate restructuring designed to streamline our organizational structure and drive operational efficiencies.
We calculate our MBR by dividing total medical expenses, excluding depreciation, equity-based compensation and clinical restructuring costs, by total revenues in a given period. We believe our MBR is an indicator of our gross profit for our Medicare Advantage plans and demonstrates the ability of our clinical model to produce superior outcomes by identifying and providing targeted care to our high-risk members resulting in improved member health and reduced total population medical expenses. We expect that this metric may fluctuate over time due to a variety of factors, including our pace of new member growth given that new members typically join Alignment with higher MBRs, while our model has demonstrated an ability to improve MBR for a given cohort over time.
When we determine, on an annual basis, whether we have satisfied the CMS minimum Medical Loss Ratio of 85%, adjustments are made to the MBR calculation to include certain additional expenses related to improving the quality of care provided, and to exclude certain taxes and fees, in each case as permitted or required by CMS and applicable regulatory requirements.
Adjusted EBITDA
Adjusted EBITDA is a non-GAAP financial measure that we define as net loss before interest expense, income taxes, depreciation and amortization expense, acquisition expenses, certain litigation costs, gains or losses on right of use ("ROU") assets, restructuring costs and equity-based compensation expense. Adjusted EBITDA is a key measure used by our management and our Board to understand and evaluate our operating performance and trends, to prepare and approve our annual budget and to develop short and long-term operating plans. In particular, we believe that the exclusion of the amounts eliminated in calculating Adjusted EBITDA provides useful measures for period-to-period comparisons of our business, as we do not consider the excluded items to be part of our ongoing results of operations. Given our intent to continue to invest in our platform and the scalability of our business in the short to medium-term, we believe Adjusted EBITDA over the long term will be an important indicator of value creation.
Adjusted EBITDA should not be considered in isolation of, or as an alternative to, measures prepared in accordance with GAAP. There are a number of limitations related to the use of Adjusted EBITDA in lieu of net loss, which is the most directly comparable financial measure calculated in accordance with GAAP.
Our use of the term Adjusted EBITDA may vary from the use of similar terms by other companies in our industry and accordingly may not be comparable to similarly titled measures used by other companies.
Adjusted EBITDA is reconciled as follows:
| | | | | | | | | | | | | | | | | | | | | | | |
| | Three Months Ended June 30, | | Six Months Ended June 30, |
| | 2024 | | 2023 | | 2024 | | 2023 |
| (dollars in thousands) | | | | | | | |
| Net loss | $ | (24,003) | | | $ | (28,494) | | | $ | (70,578) | | | $ | (65,865) | |
| Less: Net (income) loss attributable to noncontrolling interest | (7) | | | 17 | | | 47 | | | 104 | |
| Adjustments: | | | | | | | |
| Interest expense | 5,691 | | | 5,262 | | | 11,118 | | | 10,281 | |
| Depreciation and amortization | 6,539 | | | 5,264 | | | 12,568 | | | 10,246 | |
| Income taxes | 22 | | | 1 | | | 22 | | | 2 | |
Equity-based compensation(1) | 16,784 | | | 15,636 | | | 37,638 | | | 37,614 | |
Acquisition expenses(2) | 12 | | | 548 | | | 12 | | | 680 | |
Litigation costs (3) | 401 | | | — | | | 721 | | | — | |
(Gain) loss on ROU assets(4) | — | | | (289) | | | 143 | | | (289) | |
Restructuring costs(5) | 595 | | | — | | | 2,363 | | | — | |
| Adjusted EBITDA | $ | 6,034 | | | $ | (2,055) | | | $ | (5,946) | | | $ | (7,227) | |
(1)Represents equity-based compensation related to grants made in the applicable year, as well as equity-based compensation related to the timing of the IPO, which includes previously issued stock appreciation rights ("SARs") liability awards, modifications related to transaction vesting units, and grants made in conjunction with the IPO.
(2)Represents acquisition-related fees, such as legal and advisory fees, that are non-capitalizable.
(3)Represents litigation costs considered outside of the ordinary course of business based on the following considerations which we assess regularly: (i) the frequency of similar cases that have been brought to date, or are expected to be brought within two years, (ii) complexity of the case, (iii) nature of the remedies sought, (iv) litigation posture of the Company, (v) counterparty involved, and (vi) the Company's overall litigation strategy.
(4)Represents gains or losses related to ROU assets that were terminated or subleased in the respective period.
(5)Represents severance and related costs incurred as part of a corporate restructuring designed to streamline our organizational structure and drive operational efficiencies.
Results of Operations
The following table sets forth our consolidated statements of operations data for the periods indicated:
| | | | | | | | | | | | | | | | | | | | | | | |
| | Three Months Ended June 30, | | Six Months Ended June 30, |
| | 2024 | | 2023 | | 2024 | | 2023 |
| (dollars in thousands) | | | | | | | |
| Revenues: | | | | | | | |
| Earned premiums | $ | 674,094 | | | $ | 456,877 | | | $ | 1,295,650 | | | $ | 891,689 | |
| Other | 7,192 | | | 5,502 | | | 14,237 | | | 9,845 | |
| Total revenues | 681,286 | | | 462,379 | | | 1,309,887 | | | 901,534 | |
| Expenses: | | | | | | | |
| Medical expenses | 605,312 | | | 410,644 | | | 1,178,530 | | | 806,959 | |
| Selling, general and administrative expenses | 87,863 | | | 70,199 | | | 178,375 | | | 140,607 | |
| Depreciation and amortization | 6,493 | | | 5,195 | | | 12,470 | | | 10,116 | |
| Total expenses | 699,668 | | | 486,038 | | | 1,369,375 | | | 957,682 | |
| Loss from operations | (18,382) | | | (23,659) | | | (59,488) | | | (56,148) | |
| Other expenses: | | | | | | | |
| Interest expense | 5,691 | | | 5,262 | | | 11,118 | | | 10,281 | |
| Other income, net | (92) | | | (428) | | | (50) | | | (566) | |
| Total other expenses | 5,599 | | | 4,834 | | | 11,068 | | | 9,715 | |
| Loss before income taxes | (23,981) | | | (28,493) | | | (70,556) | | | (65,863) | |
| Provision for income taxes | 22 | | | 1 | | | 22 | | | 2 | |
| Net loss | $ | (24,003) | | | $ | (28,494) | | | $ | (70,578) | | | $ | (65,865) | |
| Less: Net (income) loss attributable to noncontrolling interest | (7) | | | 17 | | | 47 | | | 104 | |
| Net loss attributable to Alignment Healthcare, Inc. | $ | (24,010) | | | $ | (28,477) | | | $ | (70,531) | | | $ | (65,761) | |
The following table sets forth our consolidated statements of operations data expressed as a percentage of total revenues for the periods indicated:
| | | | | | | | | | | | | | | | | | | | | | | |
| | Three Months Ended June 30, | | Six Months Ended June 30, |
| | 2024 | | 2023 | | 2024 | | 2023 |
| (% of revenue) | | | | | | | |
| Revenues: | | | | | | | |
| Earned premiums | 99 | % | | 99 | % | | 99 | % | | 99 | % |
| Other | 1 | | | 1 | | | 1 | | | 1 | |
| Total revenues | 100 | | | 100 | | | 100 | | | 100 | |
| Expenses: | | | | | | | |
| Medical expenses | 89 | | | 89 | | | 90 | | | 89 | |
| Selling, general and administrative expenses | 13 | | | 15 | | | 14 | | | 16 | |
| Depreciation and amortization | 1 | | | 1 | | | 1 | | | 1 | |
| Total expenses | 103 | | | 105 | | | 105 | | | 106 | |
| Loss from operations | (3) | | | (5) | | | (5) | | | (6) | |
| Other expenses: | | | | | | | |
| Interest expense | 1 | | | 1 | | | 1 | | | 1 | |
| Other income, net | — | | | — | | | — | | | — | |
| Total other expenses | 1 | | | 1 | | | 1 | | | 1 | |
| Loss before income taxes | (4) | | | (6) | | | (6) | | | (7) | |
| Provision for income taxes | — | | | — | | | — | | | — | |
| Net loss | (4) | | | (6) | | | (6) | | | (7) | |
| Less: Net (income) loss attributable to noncontrolling interest | — | | | — | | | — | | | — | |
| Net loss attributable to Alignment Healthcare, Inc. | (4) | % | | (6) | % | | (6) | % | | (7) | % |
Revenues
| | | | | | | | | | | | | | | | | | | | | | | |
| Three Months Ended June 30, | | Change |
| 2024 | | 2023 | | $ | | % |
| (dollars in thousands) | | | | | | | |
| Revenues: | | | | | | | |
| Earned premiums | $ | 674,094 | | | $ | 456,877 | | | $ | 217,217 | | | 47.5 | % |
| Other | 7,192 | | | 5,502 | | | 1,690 | | | 30.7 | % |
| Total revenues | $ | 681,286 | | | $ | 462,379 | | | $ | 218,907 | | | 47.3 | % |
| | | | | | | | | | | | | | | | | | | | | | | |
| Six Months Ended June 30, | | Change |
| 2024 | | 2023 | | $ | | % |
| (dollars in thousands) | | | | | | | |
| Revenues: | | | | | | | |
| Earned premiums | $ | 1,295,650 | | | $ | 891,689 | | | $ | 403,961 | | | 45.3 | % |
| Other | 14,237 | | | 9,845 | | | 4,392 | | | 44.6 | % |
| Total revenues | $ | 1,309,887 | | | $ | 901,534 | | | $ | 408,353 | | | 45.3 | % |
Earned Premiums. Earned premium revenues were $674.1 million and $456.9 million for the three months ended June 30, 2024 and 2023, respectively, an increase of $217.2 million or 47.5%. Earned premium revenues were $1,295.7 million and $891.7 million for the six months ended June 30, 2024 and 2023, respectively, an increase of $404.0 million or 45.3%. The increase was primarily driven by growth in our Health Plan membership, which increased 56.1% between June 30, 2023
and June 30, 2024. The increase was offset by a decrease in ACO REACH revenue due to the change from gross to net revenue treatment. ACO REACH revenue decreased $31.3 million, or 104.0%, for the three months ended June 30, 2024 compared to the three months ended June 30, 2023 and decreased $63.2 million, or 101.6%, for the six months ended June 30, 2024 compared to the six months ended June 30, 2023.
Other Revenue. Other revenue increased $1.7 million for the three months ended June 30, 2024 compared to the three months ended June 30, 2023, an increase of 30.7%. Other revenue increased $4.4 million for the six months ended June 30, 2024 compared to the six months ended June 30, 2023, an increase of 44.6%. The increase is mainly attributable to an increase in the interest rate of our interest earning cash balances and the change in gross to net revenue treatment for ACO REACH.
Expenses
| | | | | | | | | | | | | | | | | | | | | | | |
| | Three Months Ended June 30, | | Change |
| | 2024 | | 2023 | | $ | | % |
| (dollars in thousands) | | | | | | | |
| Expenses: | | | | | | | |
| Medical expenses | $ | 605,312 | | | $ | 410,644 | | | $ | 194,668 | | | 47.4 | % |
| Selling, general and administrative expenses | 87,863 | | | 70,199 | | | 17,664 | | | 25.2 | % |
| Depreciation and amortization | 6,493 | | | 5,195 | | | 1,298 | | | 25.0 | % |
| Total expenses | $ | 699,668 | | | $ | 486,038 | | | $ | 213,630 | | | 44.0 | % |
| | | | | | | | | | | | | | | | | | | | | | | |
| | Six Months Ended June 30, | | Change |
| | 2024 | | 2023 | | $ | | % |
| (dollars in thousands) | | | | | | | |
| Expenses: | | | | | | | |
| Medical expenses | $ | 1,178,530 | | | $ | 806,959 | | | $ | 371,571 | | | 46.0 | % |
| Selling, general and administrative expenses | 178,375 | | | 140,607 | | | 37,768 | | | 26.9 | % |
| Depreciation and amortization | 12,470 | | | 10,116 | | | 2,354 | | | 23.3 | % |
| Total expenses | $ | 1,369,375 | | | $ | 957,682 | | | $ | 411,693 | | | 43.0 | % |
Medical Expenses. Medical expenses were $605.3 million and $410.6 million for the three months ended June 30, 2024 and 2023, respectively, an increase of $194.7 million, or 47.4%. Medical expenses were $1,178.5 million and $806.9 million for the six months ended June 30, 2024 and 2023, respectively, an increase of $371.6 million, or 46.0%. The increase was driven primarily by the growth in Alignment’s Health Plan membership. Overall, medical expenses for the six months ended June 30, 2024 grew at a slightly higher rate than earned premium revenues compared to the six months ended June 30, 2023, primarily due to 2024 having a higher percentage of new members relative to returning members, richer member benefits and increases in unit costs, offset by lower inpatient admissions per thousand and the change in ACO REACH accounting.
Selling, General and Administrative Expenses. Selling, general and administrative expenses were $87.9 million and $70.2 million for the three months ended June 30, 2024 and 2023, respectively, an increase of $17.7 million, or 25.2%. Selling, general and administrative expenses were $178.4 million and $140.6 million for the six months ended June 30, 2024 and 2023, respectively, an increase of $37.8 million, or 26.9%.The increase was primarily due to an increase in ongoing investments and expenditures in network development, operations and sales and marketing to drive the growth of Alignment's Health Plan membership. Selling, general, and administrative expenses grew at a slower rate than revenue for the three and six months ended June 30, 2024 compared to the three and six months ended June 30, 2023 due to economies of scale gained from Alignment's 2024 membership growth.
Depreciation and Amortization. Depreciation and amortization expense was $6.5 million and $5.2 million for the three months ended June 30, 2024 and 2023, respectively, an increase of $1.3 million, or 25.0%. Depreciation and amortization expense was $12.5 million and $10.1 million for the six months ended June 30, 2024 and 2023, respectively, an increase of
$2.4 million, or 23.3%. The increase was primarily due to the amount and timing of our capital expenditures and the associated depreciation relative to 2023.
Other Expenses
Interest expense. Interest expense was $5.7 million and $5.3 million for the three months ended June 30, 2024 and 2023, respectively, an increase of $0.4 million or 8.2%. Interest expense was $11.1 million and $10.3 million for the six months ended June 30, 2024 and 2023, respectively, an increase of $0.8 million or 8.1%. The increase in interest expense was primarily due to a higher interest rate on our debt balance during the three and six months ended June 30, 2024 compared to the three and six months ended June 30, 2023. The average interest rate during the three months ended June 30, 2024 and 2023 was 11.83% and 11.49%, respectively. The average interest rate during the six months ended June 30, 2024 and 2023 was 11.84% and 11.27%, respectively.
Other income, net. Other income was $(0.1) million and $(0.4) million for the three months ended June 30, 2024 and 2023, respectively, a decrease of $0.3 million or (78.5)%. Other expenses (income) were $(0.1) million and $(0.6) million for the six months ended June 30, 2024 and 2023, respectively, a decrease of $0.5 million or (91.2)%. The decrease is primarily attributable to a gain recorded for the three months ended June 30, 2023 related to ROU assets that were subleased.
Liquidity and Capital Resources
General
To date, we have financed our operations principally through our IPO, private placements of our equity securities, revenues, and certain term loans (described below). As of June 30, 2024, we had $363.7 million in cash, cash equivalents and short-term investments.
We operate as a holding company in a highly regulated industry. Alignment Healthcare, Inc., our parent company, is dependent upon dividends and administrative expense reimbursements from our subsidiaries, most of which are subject to regulatory restrictions. We maintain significant levels of aggregate excess statutory capital and surplus in our state-regulated operating subsidiaries. As of June 30, 2024, our operating parent company (an indirect wholly owned subsidiary of our parent company) had $140.5 million in cash, cash equivalents and short-term investments.
We may incur operating losses in the future due to the investments we intend to continue to make in expanding our operations and sales and marketing, in further developing our technology and due to the general and administrative costs we expect to incur in connection with continuing to operate as a public company. As a result, we may require additional capital resources to execute strategic initiatives to grow our business.
We believe that our liquid assets will be sufficient to fund our operating and organic capital needs for at least the next 12 months. Our assessment of the period of time through which our financial resources will be adequate to support our operations is a forward-looking statement and involves risks and uncertainties. Our actual results could vary because of, and our future capital requirements will depend on, many factors, including our growth rate, the timing and extent of spending to expand our presence in existing markets, expand into new markets, increase our sales and marketing activities and develop our technology. Additionally, in the future we may enter into arrangements to acquire or invest in complementary businesses, services and technologies, including intellectual property rights, which may also increase our capital needs.
We have based this estimate on assumptions that may prove to be wrong, and we could use our available capital resources sooner than we currently expect. We may be required to seek additional equity or debt financing. In the event that additional financing is required from outside sources, we may not be able to raise it on terms acceptable to us or at all. If we are unable to raise additional capital when desired, or if we cannot expand our operations or otherwise capitalize on our business opportunities because we lack sufficient capital, our business, results of operations, and financial condition would be adversely affected.
Certain states in which we operate as a CMS-licensed Medicare Advantage company may require us to meet certain capital adequacy performance standards and tests. The National Association of Insurance Commissioners has adopted rules which, if implemented by the states, set minimum capitalization requirements for insurance companies, HMOs, and other entities bearing risk for healthcare coverage. The requirements take the form of risk-based capital (“RBC”) rules, which may vary from state to state. Certain states in which our health plans or risk bearing entities operate have adopted the RBC rules.
Other states in which our health plans or risk bearing entities operate have chosen not to adopt the RBC rules, but instead have designed and implemented their own rules regarding capital adequacy. As of June 30, 2024, our health plans or risk-bearing entities were in compliance with the minimum capital requirements.
Oxford Term Loan
On September 2, 2022 (the “Effective Date”), we, Alignment Healthcare USA, LLC, an indirect subsidiary of the Company (the “Borrower”) and certain of our other subsidiaries (together with the Company and the Borrower, the “Borrower Parties”) entered into a term loan agreement (the “Oxford Loan Agreement”) with Oxford Finance LLC (“Oxford”), as administrative agent, collateral agent and a lender, and the other lenders from time to time party thereto (collectively, the “Lenders”), pursuant to which the Lenders have agreed to lend the Borrower an aggregate principal amount of up to $250.0 million in a series of term loans (the “Term Loans”). Pursuant to the Oxford Loan Agreement, the Borrower received an initial Term Loan of $165.0 million on the Effective Date and had the option to borrow up to an additional $85.0 million of Term Loans (such additional Term Loans, the “Delayed Draw Term Loans”). On June 14, 2024, the Borrower borrowed $50.0 million in aggregate principal amount of the Delayed Draw Term Loans, prior to the expiration date for such amount of the Delayed Draw Term Loans of June 30, 2024, to avoid losing access to the capital, to enhance the Company's balance sheet and to provide for future flexibility. As of June 30, 2024 we had the option to borrow an additional $35.0 million in undrawn Delayed Draw Term Loans, which option expires on September 1, 2025.
Interest on the Term Loans is a variable rate equal to (i) the secured overnight financing rate administered by the Federal Reserve Bank of New York for a one-month tenor, subject to a floor of 1.00%, plus (ii) an applicable margin of 6.50%. All unpaid principal and accrued and unpaid interest with respect to each Term Loan is due and payable in full on September 1, 2027. The interest rate applied during the six months ended June 30, 2024 ranged from 11.82% to 11.85%.
The Term Loans are guaranteed by certain of our wholly owned subsidiaries and collateralized by all unrestricted assets.
For certain prepayments of the Term Loans prior to the second anniversary of the Effective Date, the Borrower will be required to pay a prepayment fee of 1.00% of the principal amount of the Term Loans being prepaid.
The Oxford Loan Agreement includes customary events of default, including, among others, payment defaults, breach of representations and warranties, covenant defaults, judgment defaults, insolvency and bankruptcy defaults, and change of control. The occurrence of an event of default could result in the acceleration of the obligations under the Oxford Loan Agreement, termination of the Term Loan commitments and the right to foreclose on the collateral securing the obligations. During the existence of an event of default, the outstanding Term Loans will accrue interest at a rate per annum equal to 2.00% plus the otherwise applicable interest rate. Additionally, in the event of any contemplated asset sale or series of asset sales yielding net proceeds in excess of $2.5 million, except those excluded per the Oxford Loan Agreement, we are required to prepay the aggregate outstanding principal balance of the Term Loans in an amount equal to the entire amount of the asset sale net proceeds, plus any accrued and unpaid interest.
The Oxford Loan Agreement includes financial covenants that require the Borrower Parties to (i) maintain minimum liquidity, as defined in the Loan Agreement, of $23.0 million and (ii) satisfy a maximum permitted ratio of debt to trailing twelve-month revenue, as set forth in the Loan Agreement. As of June 30, 2024, we were in compliance with the financial covenants.
Cash Flows
The following table presents a summary of our consolidated cash flows from operating, investing and financing activities for the periods indicated:
| | | | | | | | | | | |
| | Six Months Ended June 30, |
| (dollars in thousands) | 2024 | | 2023 |
| Net cash provided by operating activities | $ | 17,291 | | | $ | 122,287 | |
| Net cash provided by (used in) investing activities | 69,671 | | | (136,638) | |
| Net cash provided by financing activities | 49,153 | | | 60 | |
| Net change in cash | 136,115 | | | (14,291) | |
| Cash, cash equivalents and restricted cash at beginning of period | 204,954 | | | 411,299 | |
| Cash, cash equivalents and restricted cash at end of period | $ | 341,069 | | | $ | 397,008 | |
Operating Activities
For the six months ended June 30, 2024, net cash provided by operating activities was $17.3 million, a decrease of $105.0 million compared to net cash provided by operating activities of $122.3 million for the six months ended June 30, 2023. The decrease is mainly attributable to the timing of our monthly premium revenue payments from CMS. We typically receive our monthly premium payments from CMS on the first day of the month. However, as the first day of July 2023 did not occur on a business day, we received the July 2023 premium payments on the last day of June 2023. At June 30, 2023 we recorded deferred premium revenue of $147.5 million. Excluding deferred premium revenue, net cash provided by operating activities increased $42.5 million, mainly attributable to an increase in medical expenses payable as a result of the increased Health Plan membership growth during the six months ended June 30, 2024 compared to the six months ended June 30, 2023.
Investing Activities
For the six months ended June 30, 2024, net cash provided by investing activities was $69.7 million, an increase of $206.3 million compared to net cash used in investing activities of $136.6 million for the six months ended June 30, 2023. The increase primarily relates to the purchase of short-term treasury securities during the six months ended June 30, 2023.
Financing Activities
For the six months ended June 30, 2024, net cash provided by financing activities was $49.2 million, an increase of $49.1 million, compared to net cash provided by financing activities of $0.06 million for the six months ended June 30, 2023. The increase in net cash provided by financing activities is mainly attributable to the $50.0 million draw down of the Oxford Delayed Draw term loan that occurred during the three months ended June 30, 2024.
Material cash requirements from known contractual and other obligations
There have been no material changes to our contractual obligations disclosed in our Annual Report.
Off-Balance Sheet Arrangements
We did not have any off-balance sheet arrangements as of June 30, 2024.
Critical Accounting Estimates
The discussion and analysis of our financial condition and results of operations are based upon our condensed consolidated financial statements, which have been prepared in accordance with U.S. generally accepted accounting principles and include the accounts of our wholly-owned subsidiaries and three variable interest entities (“VIEs”) in California and North Carolina that meet the consolidation requirements for accounting purposes. All intercompany transactions have been eliminated in consolidation. Noncontrolling interest is presented within the equity section of the condensed consolidated balance sheets.
There have been no significant changes in our critical accounting estimate policies or methodologies to our condensed consolidated financial statements. For a description of our policies regarding our critical accounting policies, see "Management's Discussion and Analysis of Financial Condition and Results of Operations—Critical Accounting Estimates" in the Annual Report.
Recent Accounting Pronouncements
See Note 2 to our condensed consolidated financial statements, “Summary of Significant Accounting Policies—Recent Accounting Pronouncements Adopted” for more information.
Item 3. Quantitative and Qualitative Disclosures About Market Risk.
Market risk represents the risk of loss that may impact our financial position due to adverse changes in financial market prices and rates. Our market risk exposure is primarily a result of exposure due to potential changes in inflation. We do not hold financial instruments for trading purposes.
Interest Rate Risk
We are exposed to risks associated with market changes in interest rates through our term loan agreement. This agreement exposes us to variability in interest payments due to changes in SOFR interest rates. We manage our exposure to this market risk by monitoring available financing alternatives.
Inflation Risk
Based on our analysis of the periods presented, we believe that inflation has not had a material effect on our operating results. There can be no assurance that future inflation will not have an adverse impact on our operating results and financial condition.
Item 4. Controls and Procedures.
Evaluation of Disclosure Controls and Procedures:
Under the supervision and with the participation of our management, including the Chief Executive Officer and Chief Financial Officer, we have evaluated the effectiveness of our disclosure controls and procedures (as defined in Rules 13a-15(e) and 15d-15(e) under the Securities Exchange Act of 1934, as amended (the “Exchange Act”), as of the end of the period covered by this report. Based on that evaluation, the Chief Executive Officer and Chief Financial Officer have concluded that these disclosure controls and procedures were effective as of June 30, 2024.
Changes to our Internal Controls over Financial Reporting:
There were no material changes in our internal control over financial reporting during the three months ended June 30, 2024 that have materially affected, or are reasonably likely to materially affect, our internal control over financial reporting.
PART II—OTHER INFORMATION
Item 1. Legal Proceedings.
See Note 12, Commitments and Contingencies – Legal Proceedings, to Alignment Healthcare, Inc.'s Condensed Consolidated Financial Statements in Part I, Item 1 of this Quarterly Report.
Item 1A. Risk Factors.
There have been no material changes to the risk factors disclosed in the Annual Report.
Item 2. Unregistered Sales of Equity Securities and Use of Proceeds.
Unregistered Sales of Equity Securities
None.
Use of Proceeds
On March 25, 2021, the Company’s Registration Statement on Form S-1 (SEC File No. 333-253824) for the initial public offering of 27,200,000 shares of common stock was declared effective by the Securities and Exchange Commission. The Company’s common stock began trading on March 26, 2021 on Nasdaq under the ticker symbol “ALHC.” The IPO closed on March 30, 2021, with the Company selling 21,700,000 shares of common stock and certain selling stockholders selling 5,500,000 shares of common stock, in each case at a price to the public of $18.00 per share. On Tuesday, April 6, 2021, pursuant to a partial exercise of the underwriters’ over-allotment option, certain selling stockholders sold an additional 3,314,216 shares of common stock at the IPO price. In the aggregate, the IPO generated approximately $361.6 million in net proceeds for the Company, which amount is net of approximately $24.4 million in underwriters’ discounts and commissions and offering costs of approximately $4.6 million. The IPO commenced on March 25, 2021 and terminated upon the partial exercise of the underwriters’ over-allotment options as described above. The representatives of the several underwriters of the IPO were Goldman Sachs & Co. LLC and Morgan Stanley & Co. LLC.
There has been no material change in the use of proceeds described in the IPO prospectus filed with the SEC on March 29, 2021. We may also use a portion of our net proceeds to acquire or invest in complementary businesses, products, services or technologies.
Purchases of Equity Securities by the Issuer and Affiliated Purchasers
None.
Item 3. Defaults Upon Senior Securities.
None.
Item 4. Mine Safety Disclosures.
Not applicable.
Item 5. Other Information.
Rule 10b5-1 Plans
During the period covered by this Quarterly Report on Form 10-Q, no director or executive officer of the Company adopted or terminated a "Rule 10b5-1 trading arrangement" or "non-Rule 10b5-1 trading arrangement," as each term is defined in Item 408(a) of Regulation S-K.
Item 6. Exhibits.
| | | | | | | | |
Exhibit Number | | Description |
| 3.1 | | |
| 3.2 | | |
| 3.3 | | |
| 4.1 | | |
| 31.1* | | |
| 31.2* | | |
| 32.1** | | |
| 32.2** | | |
| 101.INS* | | Inline XBRL Instance Document – the instance document does not appear in the Interactive Data File because XBRL tags are embedded within the Inline XBRL document. |
| 101.SCH* | | Inline XBRL Taxonomy Extension Schema Document |
| 101.CAL* | | Inline XBRL Taxonomy Extension Calculation Linkbase Document |
| 101.DEF* | | Inline XBRL Taxonomy Extension Definition Linkbase Document |
| 101.LAB* | | Inline XBRL Taxonomy Extension Label Linkbase Document |
| 101.PRE* | | Inline XBRL Taxonomy Extension Presentation Linkbase Document |
| 104* | | Cover Page Interactive Data File (embedded within the Inline XBRL document) |
_________________________
*Filed herewith.
**Furnished herewith
+Indicates management contract or compensatory plan.
SIGNATURES
Pursuant to the requirements of the Securities Exchange Act of 1934, the registrant has duly caused this report to be signed on its behalf by the undersigned thereunto duly authorized.
| | | | | | | | |
| | Alignment Healthcare, Inc. |
| | | |
Date: August 1, 2024 | By: | /s/ John Kao |
| | | John Kao |
| | | President and Chief Executive Officer |
| | | |
Date: August 1, 2024 | By: | /s/ Thomas Freeman |
| | | Thomas Freeman |
| | | Chief Financial Officer |
Exhibit 31.1
CERTIFICATION PURSUANT TO
RULES 13a-14(a) AND 15d-14(a) UNDER THE SECURITIES EXCHANGE ACT OF 1934,
AS ADOPTED PURSUANT TO SECTION 302 OF THE SARBANES-OXLEY ACT OF 2002
I, John Kao, certify that:
1.I have reviewed this Quarterly Report on Form 10-Q of Alignment Healthcare, Inc.;
2.Based on my knowledge, this report does not contain any untrue statement of a material fact or omit to state a material fact necessary to make the statements made, in light of the circumstances under which such statements were made, not misleading with respect to the period covered by this report;
3.Based on my knowledge, the financial statements, and other financial information included in this report, fairly present in all material respects the financial condition, results of operations and cash flows of the registrant as of, and for, the periods presented in this report;
4.The registrant's other certifying officer(s) and I are responsible for establishing and maintaining disclosure controls and procedures (as defined in Exchange Act Rules 13a-15(e) and 15d-15(e)) and internal control over financial reporting (as defined in Exchange Act Rules 13a-15(f) and 15d-15(f)) for the registrant and have:
(a)Designed such disclosure controls and procedures, or caused such disclosure controls and procedures to be designed under our supervision, to ensure that material information relating to the registrant, including its consolidated subsidiaries, is made known to us by others within those entities, particularly during the period in which this report is being prepared;
(b)Designed such internal control over financial reporting, or caused such internal control over financial reporting to be designed under our supervision, to provide reasonable assurance regarding the reliability of financial reporting and the preparation of financial statements for external purposes in accordance with generally accepted accounting principles;
(c)Evaluated the effectiveness of the registrant's disclosure controls and procedures and presented in this report our conclusions about the effectiveness of the disclosure controls and procedures, as of the end of the period covered by this report based on such evaluation; and
(d)Disclosed in this report any change in the registrant's internal control over financial reporting that occurred during the registrant's most recent fiscal quarter (the registrant's fourth fiscal quarter in the case of an annual report) that has materially affected, or is reasonably likely to materially affect, the registrant's internal control over financial reporting; and
5.The registrant's other certifying officer(s) and I have disclosed, based on our most recent evaluation of internal control over financial reporting, to the registrant's auditors and the audit committee of the registrant's board of directors (or persons performing the equivalent functions):
(a)All significant deficiencies and material weaknesses in the design or operation of internal control over financial reporting which are reasonably likely to adversely affect the registrant's ability to record, process, summarize and report financial information; and
(b)Any fraud, whether or not material, that involves management or other employees who have a significant role in the registrant's internal control over financial reporting.
| | | | | | | | |
Date: August 1, 2024 | By: | /s/ John Kao |
| | | John Kao |
| | | President and Chief Executive Officer |
Exhibit 31.2
CERTIFICATION PURSUANT TO
RULES 13a-14(a) AND 15d-14(a) UNDER THE SECURITIES EXCHANGE ACT OF 1934,
AS ADOPTED PURSUANT TO SECTION 302 OF THE SARBANES-OXLEY ACT OF 2002
I, Thomas Freeman, certify that:
1.I have reviewed this Quarterly Report on Form 10-Q of Alignment Healthcare, Inc.;
2.Based on my knowledge, this report does not contain any untrue statement of a material fact or omit to state a material fact necessary to make the statements made, in light of the circumstances under which such statements were made, not misleading with respect to the period covered by this report;
3.Based on my knowledge, the financial statements, and other financial information included in this report, fairly present in all material respects the financial condition, results of operations and cash flows of the registrant as of, and for, the periods presented in this report;
4.The registrant's other certifying officer(s) and I are responsible for establishing and maintaining disclosure controls and procedures (as defined in Exchange Act Rules 13a-15(e) and 15d-15(e)) and internal control over financial reporting (as defined in Exchange Act Rules 13a-15(f) and 15d-15(f)) for the registrant and have:
(a)Designed such disclosure controls and procedures, or caused such disclosure controls and procedures to be designed under our supervision, to ensure that material information relating to the registrant, including its consolidated subsidiaries, is made known to us by others within those entities, particularly during the period in which this report is being prepared;
(b)Designed such internal control over financial reporting, or caused such internal control over financial reporting to be designed under our supervision, to provide reasonable assurance regarding the reliability of financial reporting and the preparation of financial statements for external purposes in accordance with generally accepted accounting principles;
(c)Evaluated the effectiveness of the registrant's disclosure controls and procedures and presented in this report our conclusions about the effectiveness of the disclosure controls and procedures, as of the end of the period covered by this report based on such evaluation; and
(d)Disclosed in this report any change in the registrant's internal control over financial reporting that occurred during the registrant's most recent fiscal quarter (the registrant's fourth fiscal quarter in the case of an annual report) that has materially affected, or is reasonably likely to materially affect, the registrant's internal control over financial reporting; and
5.The registrant's other certifying officer(s) and I have disclosed, based on our most recent evaluation of internal control over financial reporting, to the registrant's auditors and the audit committee of the registrant's board of directors (or persons performing the equivalent functions):
(a)All significant deficiencies and material weaknesses in the design or operation of internal control over financial reporting which are reasonably likely to adversely affect the registrant's ability to record, process, summarize and report financial information; and
(b)Any fraud, whether or not material, that involves management or other employees who have a significant role in the registrant's internal control over financial reporting.
| | | | | | | | |
Date: August 1, 2024 | By: | /s/ Thomas Freeman |
| | | Thomas Freeman |
| | | Chief Financial Officer |
Exhibit 32.1
CERTIFICATION PURSUANT TO
18 U.S.C. SECTION 1350, AS ADOPTED PURSUANT TO
SECTION 906 OF THE SARBANES-OXLEY ACT OF 2002
In connection with the Quarterly Report of Alignment Healthcare, Inc. (the “Company”) on Form 10-Q for the period ending June 30, 2024 as filed with the Securities and Exchange Commission on the date hereof (the “Report”), I, John Kao, Chief Executive Officer of the Company, hereby certify, pursuant to 18 U.S.C. § 1350, as adopted pursuant to § 906 of the Sarbanes-Oxley Act of 2002, that, to my knowledge:
(1)The Report fully complies with the requirements of section 13(a) or 15(d) of the Securities Exchange Act of 1934; and
(2)The information contained in the Report fairly presents, in all material respects, the financial condition and results of operations of the Company.
| | | | | | | | |
Date: August 1, 2024 | By: | /s/ John Kao |
| | | John Kao |
| | | President and Chief Executive Officer |
Exhibit 32.2
CERTIFICATION PURSUANT TO
18 U.S.C. SECTION 1350, AS ADOPTED PURSUANT TO
SECTION 906 OF THE SARBANES-OXLEY ACT OF 2002
In connection with the Quarterly Report of Alignment Healthcare, Inc. (the “Company”) on Form 10-Q for the period ending June 30, 2024 as filed with the Securities and Exchange Commission on the date hereof (the “Report”), I, Thomas Freeman, Chief Financial Officer of the Company, hereby certify, pursuant to 18 U.S.C. § 1350, as adopted pursuant to § 906 of the Sarbanes-Oxley Act of 2002, that, to my knowledge:
(1)The Report fully complies with the requirements of section 13(a) or 15(d) of the Securities Exchange Act of 1934; and
(2)The information contained in the Report fairly presents, in all material respects, the financial condition and results of operations of the Company.
| | | | | | | | |
Date: August 1, 2024 | By: | /s/ Thomas Freeman |
| | | Thomas Freeman |
| | | Chief Financial Officer |
Cover - shares
|
6 Months Ended |
|
Jun. 30, 2024 |
Jul. 29, 2024 |
| Cover [Abstract] |
|
|
| Document Type |
10-Q
|
|
| Document Quarterly Report |
true
|
|
| Document Period End Date |
Jun. 30, 2024
|
|
| Document Transition Report |
false
|
|
| Entity File Number |
001-40295
|
|
| Entity Registrant Name |
ALIGNMENT HEALTHCARE, INC.
|
|
| Entity Incorporation, State or Country Code |
DE
|
|
| Entity Tax Identification Number |
46-5596242
|
|
| Entity Address, Address Line One |
1100 W. Town and Country Road
|
|
| Entity Address, Address Line Two |
Suite 1600
|
|
| Entity Address, City or Town |
Orange
|
|
| Entity Address, State or Province |
CA
|
|
| Entity Address, Postal Zip Code |
92868
|
|
| City Area Code |
844
|
|
| Local Phone Number |
310-2247
|
|
| Title of 12(b) Security |
Common Stock, par value $0.001 per share
|
|
| Trading Symbol |
ALHC
|
|
| Security Exchange Name |
NASDAQ
|
|
| Entity Current Reporting Status |
Yes
|
|
| Entity Interactive Data Current |
Yes
|
|
| Entity Filer Category |
Large Accelerated Filer
|
|
| Entity Small Business |
false
|
|
| Entity Emerging Growth Company |
false
|
|
| Entity Shell Company |
false
|
|
| Entity Common Stock, Shares Outstanding (in shares) |
|
191,299,946
|
| Amendment Flag |
false
|
|
| Document Fiscal Period Focus |
Q2
|
|
| Current Fiscal Year End Date |
--12-31
|
|
| Entity Central Index Key |
0001832466
|
|
| Document Fiscal Year Focus |
2024
|
|
| X |
- DefinitionBoolean flag that is true when the XBRL content amends previously-filed or accepted submission.
| Name: |
dei_AmendmentFlag |
| Namespace Prefix: |
dei_ |
| Data Type: |
xbrli:booleanItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionEnd date of current fiscal year in the format --MM-DD.
| Name: |
dei_CurrentFiscalYearEndDate |
| Namespace Prefix: |
dei_ |
| Data Type: |
xbrli:gMonthDayItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionFiscal period values are FY, Q1, Q2, and Q3. 1st, 2nd and 3rd quarter 10-Q or 10-QT statements have value Q1, Q2, and Q3 respectively, with 10-K, 10-KT or other fiscal year statements having FY.
| Name: |
dei_DocumentFiscalPeriodFocus |
| Namespace Prefix: |
dei_ |
| Data Type: |
dei:fiscalPeriodItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionThis is focus fiscal year of the document report in YYYY format. For a 2006 annual report, which may also provide financial information from prior periods, fiscal 2006 should be given as the fiscal year focus. Example: 2006.
| Name: |
dei_DocumentFiscalYearFocus |
| Namespace Prefix: |
dei_ |
| Data Type: |
xbrli:gYearItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionFor the EDGAR submission types of Form 8-K: the date of the report, the date of the earliest event reported; for the EDGAR submission types of Form N-1A: the filing date; for all other submission types: the end of the reporting or transition period. The format of the date is YYYY-MM-DD.
| Name: |
dei_DocumentPeriodEndDate |
| Namespace Prefix: |
dei_ |
| Data Type: |
xbrli:dateItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionBoolean flag that is true only for a form used as an quarterly report. Reference 1: http://www.xbrl.org/2003/role/presentationRef
-Publisher SEC
-Name Form 10-Q
-Number 240
-Section 308
-Subsection a
| Name: |
dei_DocumentQuarterlyReport |
| Namespace Prefix: |
dei_ |
| Data Type: |
xbrli:booleanItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionBoolean flag that is true only for a form used as a transition report. Reference 1: http://www.xbrl.org/2003/role/presentationRef
-Publisher SEC
-Name Forms 10-K, 10-Q, 20-F
-Number 240
-Section 13
-Subsection a-1
| Name: |
dei_DocumentTransitionReport |
| Namespace Prefix: |
dei_ |
| Data Type: |
xbrli:booleanItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionThe type of document being provided (such as 10-K, 10-Q, 485BPOS, etc). The document type is limited to the same value as the supporting SEC submission type, or the word 'Other'.
| Name: |
dei_DocumentType |
| Namespace Prefix: |
dei_ |
| Data Type: |
dei:submissionTypeItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionAddress Line 1 such as Attn, Building Name, Street Name
| Name: |
dei_EntityAddressAddressLine1 |
| Namespace Prefix: |
dei_ |
| Data Type: |
xbrli:normalizedStringItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionAddress Line 2 such as Street or Suite number
| Name: |
dei_EntityAddressAddressLine2 |
| Namespace Prefix: |
dei_ |
| Data Type: |
xbrli:normalizedStringItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- Definition
+ References
+ Details
| Name: |
dei_EntityAddressCityOrTown |
| Namespace Prefix: |
dei_ |
| Data Type: |
xbrli:normalizedStringItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionCode for the postal or zip code
| Name: |
dei_EntityAddressPostalZipCode |
| Namespace Prefix: |
dei_ |
| Data Type: |
xbrli:normalizedStringItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionName of the state or province.
| Name: |
dei_EntityAddressStateOrProvince |
| Namespace Prefix: |
dei_ |
| Data Type: |
dei:stateOrProvinceItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionA unique 10-digit SEC-issued value to identify entities that have filed disclosures with the SEC. It is commonly abbreviated as CIK. Reference 1: http://www.xbrl.org/2003/role/presentationRef
-Publisher SEC
-Name Exchange Act
-Number 240
-Section 12
-Subsection b-2
| Name: |
dei_EntityCentralIndexKey |
| Namespace Prefix: |
dei_ |
| Data Type: |
dei:centralIndexKeyItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionIndicate number of shares or other units outstanding of each of registrant's classes of capital or common stock or other ownership interests, if and as stated on cover of related periodic report. Where multiple classes or units exist define each class/interest by adding class of stock items such as Common Class A [Member], Common Class B [Member] or Partnership Interest [Member] onto the Instrument [Domain] of the Entity Listings, Instrument.
| Name: |
dei_EntityCommonStockSharesOutstanding |
| Namespace Prefix: |
dei_ |
| Data Type: |
xbrli:sharesItemType |
| Balance Type: |
na |
| Period Type: |
instant |
|
| X |
- DefinitionIndicate 'Yes' or 'No' whether registrants (1) have filed all reports required to be filed by Section 13 or 15(d) of the Securities Exchange Act of 1934 during the preceding 12 months (or for such shorter period that registrants were required to file such reports), and (2) have been subject to such filing requirements for the past 90 days. This information should be based on the registrant's current or most recent filing containing the related disclosure.
| Name: |
dei_EntityCurrentReportingStatus |
| Namespace Prefix: |
dei_ |
| Data Type: |
dei:yesNoItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionIndicate if registrant meets the emerging growth company criteria. Reference 1: http://www.xbrl.org/2003/role/presentationRef
-Publisher SEC
-Name Exchange Act
-Number 240
-Section 12
-Subsection b-2
| Name: |
dei_EntityEmergingGrowthCompany |
| Namespace Prefix: |
dei_ |
| Data Type: |
xbrli:booleanItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionCommission file number. The field allows up to 17 characters. The prefix may contain 1-3 digits, the sequence number may contain 1-8 digits, the optional suffix may contain 1-4 characters, and the fields are separated with a hyphen.
| Name: |
dei_EntityFileNumber |
| Namespace Prefix: |
dei_ |
| Data Type: |
dei:fileNumberItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionIndicate whether the registrant is one of the following: Large Accelerated Filer, Accelerated Filer, Non-accelerated Filer. Definitions of these categories are stated in Rule 12b-2 of the Exchange Act. This information should be based on the registrant's current or most recent filing containing the related disclosure. Reference 1: http://www.xbrl.org/2003/role/presentationRef
-Publisher SEC
-Name Exchange Act
-Number 240
-Section 12
-Subsection b-2
| Name: |
dei_EntityFilerCategory |
| Namespace Prefix: |
dei_ |
| Data Type: |
dei:filerCategoryItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionTwo-character EDGAR code representing the state or country of incorporation.
| Name: |
dei_EntityIncorporationStateCountryCode |
| Namespace Prefix: |
dei_ |
| Data Type: |
dei:edgarStateCountryItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionBoolean flag that is true when the registrant has submitted electronically every Interactive Data File required to be submitted pursuant to Rule 405 of Regulation S-T during the preceding 12 months (or for such shorter period that the registrant was required to submit such files). Reference 1: http://www.xbrl.org/2003/role/presentationRef
-Publisher SEC
-Name Regulation S-T
-Number 232
-Section 405
| Name: |
dei_EntityInteractiveDataCurrent |
| Namespace Prefix: |
dei_ |
| Data Type: |
dei:yesNoItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionThe exact name of the entity filing the report as specified in its charter, which is required by forms filed with the SEC. Reference 1: http://www.xbrl.org/2003/role/presentationRef
-Publisher SEC
-Name Exchange Act
-Number 240
-Section 12
-Subsection b-2
| Name: |
dei_EntityRegistrantName |
| Namespace Prefix: |
dei_ |
| Data Type: |
xbrli:normalizedStringItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionBoolean flag that is true when the registrant is a shell company as defined in Rule 12b-2 of the Exchange Act. Reference 1: http://www.xbrl.org/2003/role/presentationRef
-Publisher SEC
-Name Exchange Act
-Number 240
-Section 12
-Subsection b-2
| Name: |
dei_EntityShellCompany |
| Namespace Prefix: |
dei_ |
| Data Type: |
xbrli:booleanItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionIndicates that the company is a Smaller Reporting Company (SRC). Reference 1: http://www.xbrl.org/2003/role/presentationRef
-Publisher SEC
-Name Exchange Act
-Number 240
-Section 12
-Subsection b-2
| Name: |
dei_EntitySmallBusiness |
| Namespace Prefix: |
dei_ |
| Data Type: |
xbrli:booleanItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionThe Tax Identification Number (TIN), also known as an Employer Identification Number (EIN), is a unique 9-digit value assigned by the IRS. Reference 1: http://www.xbrl.org/2003/role/presentationRef
-Publisher SEC
-Name Exchange Act
-Number 240
-Section 12
-Subsection b-2
| Name: |
dei_EntityTaxIdentificationNumber |
| Namespace Prefix: |
dei_ |
| Data Type: |
dei:employerIdItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionLocal phone number for entity.
| Name: |
dei_LocalPhoneNumber |
| Namespace Prefix: |
dei_ |
| Data Type: |
xbrli:normalizedStringItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionTitle of a 12(b) registered security. Reference 1: http://www.xbrl.org/2003/role/presentationRef
-Publisher SEC
-Name Exchange Act
-Number 240
-Section 12
-Subsection b
| Name: |
dei_Security12bTitle |
| Namespace Prefix: |
dei_ |
| Data Type: |
dei:securityTitleItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionName of the Exchange on which a security is registered. Reference 1: http://www.xbrl.org/2003/role/presentationRef
-Publisher SEC
-Name Exchange Act
-Number 240
-Section 12
-Subsection d1-1
| Name: |
dei_SecurityExchangeName |
| Namespace Prefix: |
dei_ |
| Data Type: |
dei:edgarExchangeCodeItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionTrading symbol of an instrument as listed on an exchange.
| Name: |
dei_TradingSymbol |
| Namespace Prefix: |
dei_ |
| Data Type: |
dei:tradingSymbolItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
v3.24.2.u1
Condensed Consolidated Balance Sheets - USD ($)
$ in Thousands |
Jun. 30, 2024 |
Dec. 31, 2023 |
| Current Assets: |
|
|
| Cash and cash equivalents |
$ 339,007
|
$ 202,904
|
| Accounts receivable (less allowance for credit losses of $95 at June 30, 2024 and $0 at December 31, 2023) |
183,214
|
119,749
|
| Investments - current |
24,701
|
115,914
|
| Prepaid expenses and other current assets |
52,191
|
44,970
|
| Total current assets |
599,113
|
483,537
|
| Property and equipment, net |
62,430
|
51,901
|
| Right of use asset, net |
8,085
|
9,959
|
| Goodwill |
34,826
|
34,826
|
| Intangible Assets, net |
5,201
|
5,252
|
| Other assets |
6,603
|
6,405
|
| Total assets |
716,258
|
591,880
|
| Current Liabilities: |
|
|
| Medical expenses payable |
315,369
|
205,399
|
| Accounts payable and accrued expenses |
23,336
|
23,511
|
| Accrued compensation |
32,834
|
34,112
|
| Total current liabilities |
371,539
|
263,022
|
| Long-term debt, net of debt issuance costs |
211,742
|
161,813
|
| Long-term portion of lease liabilities |
8,179
|
8,974
|
| Total liabilities |
591,460
|
433,809
|
| Commitments and Contingencies (Note 12) |
|
|
| Stockholders' Equity: |
|
|
| Preferred stock, $.001 par value; 100,000,000 shares authorized as of June 30, 2024 and December 31, 2023, respectively; no shares issued and outstanding as of June 30, 2024 and December 31, 2023 |
0
|
0
|
| Common stock, $.001 par value; 1,000,000,000 shares authorized as of June 30, 2024 and December 31, 2023; 191,236,747 and 188,951,643 shares issued and outstanding as of June 30, 2024 and December 31, 2023, respectively |
191
|
189
|
| Additional paid-in capital |
1,074,303
|
1,037,015
|
| Accumulated deficit |
(950,789)
|
(880,258)
|
| Total Alignment Healthcare, Inc. stockholders' equity |
123,705
|
156,946
|
| Noncontrolling interest |
1,093
|
1,125
|
| Total stockholders' equity |
124,798
|
158,071
|
| Total liabilities and stockholders' equity |
$ 716,258
|
$ 591,880
|
| X |
- DefinitionMedical expenses payable current
| Name: |
alhc_MedicalExpensesPayableCurrent |
| Namespace Prefix: |
alhc_ |
| Data Type: |
xbrli:monetaryItemType |
| Balance Type: |
credit |
| Period Type: |
instant |
|
| X |
- DefinitionSum of the carrying values as of the balance sheet date of obligations incurred through that date and due within one year (or the operating cycle, if longer), including liabilities incurred (and for which invoices have typically been received) and payable to vendors for goods and services received, taxes, interest, rent and utilities, accrued salaries and bonuses, payroll taxes and fringe benefits. Reference 1: http://fasb.org/us-gaap/role/ref/legacyRef
-Topic 210
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.5-02(20))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480566/210-10-S99-1
Reference 2: http://fasb.org/us-gaap/role/ref/legacyRef
-Topic 210
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.5-02(19))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480566/210-10-S99-1
| Name: |
us-gaap_AccountsPayableAndAccruedLiabilitiesCurrent |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:monetaryItemType |
| Balance Type: |
credit |
| Period Type: |
instant |
|
| X |
- DefinitionAmount, after allowance for credit loss, of right to consideration from customer for product sold and service rendered in normal course of business, classified as current. Reference 1: http://www.xbrl.org/2009/role/commonPracticeRef
-Topic 310
-SubTopic 10
-Name Accounting Standards Codification
-Section 45
-Paragraph 2
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147481990/310-10-45-2
| Name: |
us-gaap_AccountsReceivableNetCurrent |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:monetaryItemType |
| Balance Type: |
debit |
| Period Type: |
instant |
|
| X |
- DefinitionAmount of excess of issue price over par or stated value of stock and from other transaction involving stock or stockholder. Includes, but is not limited to, additional paid-in capital (APIC) for common and preferred stock. Reference 1: http://www.xbrl.org/2003/role/exampleRef
-Topic 852
-SubTopic 10
-Name Accounting Standards Codification
-Section 55
-Paragraph 10
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147481372/852-10-55-10
Reference 2: http://www.xbrl.org/2009/role/commonPracticeRef
-Topic 946
-SubTopic 210
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.6-04(18))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147479170/946-210-S99-1
Reference 3: http://fasb.org/us-gaap/role/ref/legacyRef
-Topic 210
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.5-02(30)(a)(1))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480566/210-10-S99-1
| Name: |
us-gaap_AdditionalPaidInCapital |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:monetaryItemType |
| Balance Type: |
credit |
| Period Type: |
instant |
|
| X |
- DefinitionAmount of asset recognized for present right to economic benefit. Reference 1: http://www.xbrl.org/2003/role/exampleRef
-Topic 280
-SubTopic 10
-Name Accounting Standards Codification
-Section 55
-Paragraph 48
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482785/280-10-55-48
Reference 2: http://www.xbrl.org/2003/role/exampleRef
-Topic 280
-SubTopic 10
-Name Accounting Standards Codification
-Section 55
-Paragraph 49
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482785/280-10-55-49
Reference 3: http://www.xbrl.org/2003/role/disclosureRef
-Topic 270
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 1
-Subparagraph (i)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482964/270-10-50-1
Reference 4: http://www.xbrl.org/2003/role/disclosureRef
-Topic 280
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 32
-Subparagraph (ee)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482810/280-10-50-32
Reference 5: http://fasb.org/us-gaap/role/ref/otherTransitionRef
-Topic 280
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 32
-Subparagraph (d)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482810/280-10-50-32
Reference 6: http://www.xbrl.org/2003/role/disclosureRef
-Topic 280
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 22
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482810/280-10-50-22
Reference 7: http://www.xbrl.org/2003/role/disclosureRef
-Topic 810
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 3
-Subparagraph (bb)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147481203/810-10-50-3
Reference 8: http://www.xbrl.org/2003/role/disclosureRef
-Topic 810
-SubTopic 10
-Name Accounting Standards Codification
-Section 45
-Paragraph 25
-Subparagraph (a)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147481231/810-10-45-25
Reference 9: http://www.xbrl.org/2003/role/disclosureRef
-Topic 235
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.4-08(g)(1)(ii))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480678/235-10-S99-1
Reference 10: http://www.xbrl.org/2003/role/disclosureRef
-Topic 323
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 3
-Subparagraph (c)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147481687/323-10-50-3
Reference 11: http://www.xbrl.org/2003/role/disclosureRef
-Topic 825
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 28
-Subparagraph (f)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482907/825-10-50-28
Reference 12: http://www.xbrl.org/2003/role/exampleRef
-Topic 852
-SubTopic 10
-Name Accounting Standards Codification
-Section 55
-Paragraph 10
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147481372/852-10-55-10
Reference 13: http://www.xbrl.org/2003/role/exampleRef
-Topic 946
-SubTopic 830
-Name Accounting Standards Codification
-Section 55
-Paragraph 12
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147479168/946-830-55-12
Reference 14: http://www.xbrl.org/2003/role/disclosureRef
-Topic 944
-SubTopic 210
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.7-03(a)(12))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147478777/944-210-S99-1
Reference 15: http://www.xbrl.org/2003/role/disclosureRef
-Topic 946
-SubTopic 210
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.6-04(8))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147479170/946-210-S99-1
Reference 16: http://www.xbrl.org/2003/role/disclosureRef
-Topic 210
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.5-02(18))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480566/210-10-S99-1
Reference 17: http://www.xbrl.org/2003/role/disclosureRef
-Topic 470
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1A
-Subparagraph (SX 210.13-01(a)(4)(i))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480097/470-10-S99-1A
Reference 18: http://www.xbrl.org/2009/role/commonPracticeRef
-Topic 470
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1A
-Subparagraph (SX 210.13-01(a)(4)(ii))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480097/470-10-S99-1A
Reference 19: http://www.xbrl.org/2009/role/commonPracticeRef
-Topic 470
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1A
-Subparagraph (SX 210.13-01(a)(4)(iii))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480097/470-10-S99-1A
Reference 20: http://www.xbrl.org/2003/role/disclosureRef
-Topic 470
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1A
-Subparagraph (SX 210.13-01(a)(4)(iii)(A))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480097/470-10-S99-1A
Reference 21: http://www.xbrl.org/2003/role/disclosureRef
-Topic 470
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1A
-Subparagraph (SX 210.13-01(a)(4)(iv))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480097/470-10-S99-1A
Reference 22: http://www.xbrl.org/2003/role/disclosureRef
-Topic 470
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1A
-Subparagraph (SX 210.13-01(a)(5))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480097/470-10-S99-1A
Reference 23: http://www.xbrl.org/2003/role/disclosureRef
-Topic 470
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1B
-Subparagraph (SX 210.13-02(a)(4)(i))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480097/470-10-S99-1B
Reference 24: http://www.xbrl.org/2003/role/disclosureRef
-Topic 470
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1B
-Subparagraph (SX 210.13-02(a)(4)(iii)(A))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480097/470-10-S99-1B
Reference 25: http://www.xbrl.org/2003/role/disclosureRef
-Topic 470
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1B
-Subparagraph (SX 210.13-02(a)(4)(iii)(B))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480097/470-10-S99-1B
Reference 26: http://www.xbrl.org/2003/role/disclosureRef
-Topic 470
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1B
-Subparagraph (SX 210.13-02(a)(4)(iv))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480097/470-10-S99-1B
Reference 27: http://www.xbrl.org/2003/role/disclosureRef
-Topic 470
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1B
-Subparagraph (SX 210.13-02(a)(5))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480097/470-10-S99-1B
Reference 28: http://www.xbrl.org/2009/role/commonPracticeRef
-Topic 852
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 7
-Subparagraph (a)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147481404/852-10-50-7
Reference 29: http://www.xbrl.org/2003/role/disclosureRef
-Topic 280
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 30
-Subparagraph (c)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482810/280-10-50-30
Reference 30: http://fasb.org/us-gaap/role/ref/legacyRef
-Topic 942
-SubTopic 210
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.9-03(11))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147478546/942-210-S99-1
| Name: |
us-gaap_Assets |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:monetaryItemType |
| Balance Type: |
debit |
| Period Type: |
instant |
|
| X |
- DefinitionAmount of asset recognized for present right to economic benefit, classified as current. Reference 1: http://www.xbrl.org/2003/role/disclosureRef
-Topic 810
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 3
-Subparagraph (bb)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147481203/810-10-50-3
Reference 2: http://www.xbrl.org/2003/role/disclosureRef
-Topic 810
-SubTopic 10
-Name Accounting Standards Codification
-Section 45
-Paragraph 25
-Subparagraph (a)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147481231/810-10-45-25
Reference 3: http://www.xbrl.org/2003/role/disclosureRef
-Topic 235
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.4-08(g)(1)(ii))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480678/235-10-S99-1
Reference 4: http://www.xbrl.org/2003/role/disclosureRef
-Topic 323
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 3
-Subparagraph (c)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147481687/323-10-50-3
Reference 5: http://www.xbrl.org/2003/role/disclosureRef
-Topic 825
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 28
-Subparagraph (f)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482907/825-10-50-28
Reference 6: http://www.xbrl.org/2003/role/exampleRef
-Topic 852
-SubTopic 10
-Name Accounting Standards Codification
-Section 55
-Paragraph 10
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147481372/852-10-55-10
Reference 7: http://www.xbrl.org/2003/role/disclosureRef
-Topic 210
-SubTopic 10
-Name Accounting Standards Codification
-Section 45
-Paragraph 1
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147483467/210-10-45-1
Reference 8: http://www.xbrl.org/2003/role/disclosureRef
-Topic 210
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.5-02(9))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480566/210-10-S99-1
Reference 9: http://www.xbrl.org/2003/role/disclosureRef
-Topic 470
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1A
-Subparagraph (SX 210.13-01(a)(4)(i))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480097/470-10-S99-1A
Reference 10: http://www.xbrl.org/2009/role/commonPracticeRef
-Topic 470
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1A
-Subparagraph (SX 210.13-01(a)(4)(ii))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480097/470-10-S99-1A
Reference 11: http://www.xbrl.org/2009/role/commonPracticeRef
-Topic 470
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1A
-Subparagraph (SX 210.13-01(a)(4)(iii))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480097/470-10-S99-1A
Reference 12: http://www.xbrl.org/2003/role/disclosureRef
-Topic 470
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1A
-Subparagraph (SX 210.13-01(a)(4)(iii)(A))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480097/470-10-S99-1A
Reference 13: http://www.xbrl.org/2003/role/disclosureRef
-Topic 470
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1A
-Subparagraph (SX 210.13-01(a)(4)(iv))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480097/470-10-S99-1A
Reference 14: http://www.xbrl.org/2003/role/disclosureRef
-Topic 470
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1A
-Subparagraph (SX 210.13-01(a)(5))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480097/470-10-S99-1A
Reference 15: http://www.xbrl.org/2003/role/disclosureRef
-Topic 470
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1B
-Subparagraph (SX 210.13-02(a)(4)(i))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480097/470-10-S99-1B
Reference 16: http://www.xbrl.org/2003/role/disclosureRef
-Topic 470
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1B
-Subparagraph (SX 210.13-02(a)(4)(iii)(A))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480097/470-10-S99-1B
Reference 17: http://www.xbrl.org/2003/role/disclosureRef
-Topic 470
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1B
-Subparagraph (SX 210.13-02(a)(4)(iii)(B))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480097/470-10-S99-1B
Reference 18: http://www.xbrl.org/2003/role/disclosureRef
-Topic 470
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1B
-Subparagraph (SX 210.13-02(a)(4)(iv))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480097/470-10-S99-1B
Reference 19: http://www.xbrl.org/2003/role/disclosureRef
-Topic 470
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1B
-Subparagraph (SX 210.13-02(a)(5))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480097/470-10-S99-1B
Reference 20: http://www.xbrl.org/2009/role/commonPracticeRef
-Topic 852
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 7
-Subparagraph (a)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147481404/852-10-50-7
| Name: |
us-gaap_AssetsCurrent |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:monetaryItemType |
| Balance Type: |
debit |
| Period Type: |
instant |
|
| X |
- References
+ Details
| Name: |
us-gaap_AssetsCurrentAbstract |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:stringItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionAmount of currency on hand as well as demand deposits with banks or financial institutions. Includes other kinds of accounts that have the general characteristics of demand deposits. Also includes short-term, highly liquid investments that are both readily convertible to known amounts of cash and so near their maturity that they present insignificant risk of changes in value because of changes in interest rates. Excludes cash and cash equivalents within disposal group and discontinued operation. Reference 1: http://www.xbrl.org/2003/role/disclosureRef
-Topic 210
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.5-02(1))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480566/210-10-S99-1
Reference 2: http://www.xbrl.org/2003/role/exampleRef
-Topic 210
-SubTopic 10
-Name Accounting Standards Codification
-Section 45
-Paragraph 1
-Subparagraph (a)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147483467/210-10-45-1
Reference 3: http://fasb.org/us-gaap/role/ref/legacyRef
-Name Accounting Standards Codification
-Topic 230
-SubTopic 10
-Section 45
-Paragraph 4
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482740/230-10-45-4
| Name: |
us-gaap_CashAndCashEquivalentsAtCarryingValue |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:monetaryItemType |
| Balance Type: |
debit |
| Period Type: |
instant |
|
| X |
- DefinitionRepresents the caption on the face of the balance sheet to indicate that the entity has entered into (1) purchase or supply arrangements that will require expending a portion of its resources to meet the terms thereof, and (2) is exposed to potential losses or, less frequently, gains, arising from (a) possible claims against a company's resources due to future performance under contract terms, and (b) possible losses or likely gains from uncertainties that will ultimately be resolved when one or more future events that are deemed likely to occur do occur or fail to occur. Reference 1: http://fasb.org/us-gaap/role/ref/legacyRef
-Topic 942
-SubTopic 210
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.9-03(17))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147478546/942-210-S99-1
Reference 2: http://fasb.org/us-gaap/role/ref/legacyRef
-Topic 210
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.5-02(25))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480566/210-10-S99-1
Reference 3: http://www.xbrl.org/2003/role/disclosureRef
-Topic 944
-SubTopic 210
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.7-03(a)(19))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147478777/944-210-S99-1
Reference 4: http://www.xbrl.org/2003/role/disclosureRef
-Topic 946
-SubTopic 210
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.6-04(15))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147479170/946-210-S99-1
| Name: |
us-gaap_CommitmentsAndContingencies |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:monetaryItemType |
| Balance Type: |
credit |
| Period Type: |
instant |
|
| X |
- DefinitionAggregate par or stated value of issued nonredeemable common stock (or common stock redeemable solely at the option of the issuer). This item includes treasury stock repurchased by the entity. Note: elements for number of nonredeemable common shares, par value and other disclosure concepts are in another section within stockholders' equity. Reference 1: http://fasb.org/us-gaap/role/ref/legacyRef
-Topic 210
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.5-02(29))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480566/210-10-S99-1
Reference 2: http://www.xbrl.org/2003/role/exampleRef
-Topic 852
-SubTopic 10
-Name Accounting Standards Codification
-Section 55
-Paragraph 10
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147481372/852-10-55-10
Reference 3: http://www.xbrl.org/2003/role/disclosureRef
-Topic 944
-SubTopic 210
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.7-03(a)(22))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147478777/944-210-S99-1
| Name: |
us-gaap_CommonStockValue |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:monetaryItemType |
| Balance Type: |
credit |
| Period Type: |
instant |
|
| X |
- DefinitionAmount, after accumulated impairment loss, of asset representing future economic benefit arising from other asset acquired in business combination or from joint venture formation or both, that is not individually identified and separately recognized. Reference 1: http://www.xbrl.org/2003/role/exampleRef
-Topic 280
-SubTopic 10
-Name Accounting Standards Codification
-Section 55
-Paragraph 49
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482785/280-10-55-49
Reference 2: http://www.xbrl.org/2003/role/exampleRef
-Topic 350
-SubTopic 20
-Name Accounting Standards Codification
-Section 55
-Paragraph 24
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482548/350-20-55-24
Reference 3: http://www.xbrl.org/2003/role/exampleRef
-Topic 820
-SubTopic 10
-Name Accounting Standards Codification
-Section 55
-Paragraph 100
-Subparagraph (d)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482078/820-10-55-100
Reference 4: http://www.xbrl.org/2003/role/exampleRef
-Topic 852
-SubTopic 10
-Name Accounting Standards Codification
-Section 55
-Paragraph 10
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147481372/852-10-55-10
Reference 5: http://www.xbrl.org/2003/role/disclosureRef
-Topic 210
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.5-02(15))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480566/210-10-S99-1
Reference 6: http://www.xbrl.org/2003/role/disclosureRef
-Topic 350
-SubTopic 20
-Name Accounting Standards Codification
-Section 45
-Paragraph 1
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482598/350-20-45-1
Reference 7: http://www.xbrl.org/2009/role/commonPracticeRef
-Topic 350
-SubTopic 20
-Name Accounting Standards Codification
-Section 50
-Paragraph 1
-Subparagraph (a)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482573/350-20-50-1
Reference 8: http://www.xbrl.org/2009/role/commonPracticeRef
-Topic 350
-SubTopic 20
-Name Accounting Standards Codification
-Section 50
-Paragraph 1
-Subparagraph (h)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482573/350-20-50-1
Reference 9: http://www.xbrl.org/2003/role/disclosureRef
-Topic 942
-SubTopic 210
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.9-03(10)(1))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147478546/942-210-S99-1
| Name: |
us-gaap_Goodwill |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:monetaryItemType |
| Balance Type: |
debit |
| Period Type: |
instant |
|
| X |
- DefinitionSum of the carrying amounts of all intangible assets, excluding goodwill, as of the balance sheet date, net of accumulated amortization and impairment charges. Reference 1: http://www.xbrl.org/2009/role/commonPracticeRef
-Topic 350
-SubTopic 30
-Name Accounting Standards Codification
-Section 50
-Paragraph 2
-Subparagraph (a)(1)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482665/350-30-50-2
Reference 2: http://www.xbrl.org/2009/role/commonPracticeRef
-Topic 350
-SubTopic 30
-Name Accounting Standards Codification
-Section 50
-Paragraph 2
-Subparagraph (b)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482665/350-30-50-2
Reference 3: http://www.xbrl.org/2003/role/disclosureRef
-Topic 350
-SubTopic 30
-Name Accounting Standards Codification
-Section 45
-Paragraph 1
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482686/350-30-45-1
| Name: |
us-gaap_IntangibleAssetsNetExcludingGoodwill |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:monetaryItemType |
| Balance Type: |
debit |
| Period Type: |
instant |
|
| X |
- DefinitionAmount of liability recognized for present obligation requiring transfer or otherwise providing economic benefit to others. Reference 1: http://fasb.org/us-gaap/role/ref/legacyRef
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.5-02(22))
-SubTopic 10
-Topic 210
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480566/210-10-S99-1
Reference 2: http://fasb.org/us-gaap/role/ref/legacyRef
-Topic 210
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.5-02(20))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480566/210-10-S99-1
Reference 3: http://fasb.org/us-gaap/role/ref/legacyRef
-Topic 210
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.5-02(24))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480566/210-10-S99-1
Reference 4: http://fasb.org/us-gaap/role/ref/legacyRef
-Topic 210
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.5-02(19))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480566/210-10-S99-1
Reference 5: http://fasb.org/us-gaap/role/ref/legacyRef
-Topic 210
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.5-02(25))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480566/210-10-S99-1
Reference 6: http://fasb.org/us-gaap/role/ref/legacyRef
-Topic 210
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.5-02(26))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480566/210-10-S99-1
Reference 7: http://fasb.org/us-gaap/role/ref/legacyRef
-Topic 210
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.5-02(23))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480566/210-10-S99-1
Reference 8: http://fasb.org/us-gaap/role/ref/legacyRef
-Topic 210
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.5-02(21))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480566/210-10-S99-1
Reference 9: http://www.xbrl.org/2003/role/disclosureRef
-Topic 810
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 3
-Subparagraph (c)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147481203/810-10-50-3
Reference 10: http://www.xbrl.org/2003/role/disclosureRef
-Topic 810
-SubTopic 10
-Name Accounting Standards Codification
-Section 45
-Paragraph 25
-Subparagraph (b)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147481231/810-10-45-25
Reference 11: http://www.xbrl.org/2003/role/disclosureRef
-Topic 810
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 3
-Subparagraph (bb)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147481203/810-10-50-3
Reference 12: http://www.xbrl.org/2003/role/disclosureRef
-Topic 235
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.4-08(g)(1)(ii))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480678/235-10-S99-1
Reference 13: http://www.xbrl.org/2003/role/disclosureRef
-Topic 323
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 3
-Subparagraph (c)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147481687/323-10-50-3
Reference 14: http://www.xbrl.org/2003/role/disclosureRef
-Topic 825
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 28
-Subparagraph (f)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482907/825-10-50-28
Reference 15: http://www.xbrl.org/2003/role/exampleRef
-Topic 946
-SubTopic 830
-Name Accounting Standards Codification
-Section 55
-Paragraph 12
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147479168/946-830-55-12
Reference 16: http://www.xbrl.org/2003/role/disclosureRef
-Topic 946
-SubTopic 210
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.6-04(14))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147479170/946-210-S99-1
Reference 17: http://www.xbrl.org/2003/role/disclosureRef
-Topic 470
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1A
-Subparagraph (SX 210.13-01(a)(4)(i))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480097/470-10-S99-1A
Reference 18: http://www.xbrl.org/2009/role/commonPracticeRef
-Topic 470
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1A
-Subparagraph (SX 210.13-01(a)(4)(ii))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480097/470-10-S99-1A
Reference 19: http://www.xbrl.org/2003/role/disclosureRef
-Topic 470
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1A
-Subparagraph (SX 210.13-01(a)(4)(iii)(A))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480097/470-10-S99-1A
Reference 20: http://www.xbrl.org/2003/role/disclosureRef
-Topic 470
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1A
-Subparagraph (SX 210.13-01(a)(4)(iv))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480097/470-10-S99-1A
Reference 21: http://www.xbrl.org/2003/role/disclosureRef
-Topic 470
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1A
-Subparagraph (SX 210.13-01(a)(5))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480097/470-10-S99-1A
Reference 22: http://www.xbrl.org/2003/role/disclosureRef
-Topic 470
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1B
-Subparagraph (SX 210.13-02(a)(4)(i))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480097/470-10-S99-1B
Reference 23: http://www.xbrl.org/2003/role/disclosureRef
-Topic 470
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1B
-Subparagraph (SX 210.13-02(a)(4)(iii)(A))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480097/470-10-S99-1B
Reference 24: http://www.xbrl.org/2003/role/disclosureRef
-Topic 470
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1B
-Subparagraph (SX 210.13-02(a)(4)(iii)(B))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480097/470-10-S99-1B
Reference 25: http://www.xbrl.org/2003/role/disclosureRef
-Topic 470
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1B
-Subparagraph (SX 210.13-02(a)(4)(iv))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480097/470-10-S99-1B
Reference 26: http://www.xbrl.org/2003/role/disclosureRef
-Topic 470
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1B
-Subparagraph (SX 210.13-02(a)(5))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480097/470-10-S99-1B
Reference 27: http://www.xbrl.org/2009/role/commonPracticeRef
-Topic 852
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 7
-Subparagraph (a)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147481404/852-10-50-7
Reference 28: http://www.xbrl.org/2009/role/commonPracticeRef
-Topic 852
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 7
-Subparagraph (b)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147481404/852-10-50-7
Reference 29: http://www.xbrl.org/2003/role/exampleRef
-Topic 280
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 30
-Subparagraph (d)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482810/280-10-50-30
| Name: |
us-gaap_Liabilities |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:monetaryItemType |
| Balance Type: |
credit |
| Period Type: |
instant |
|
| X |
- DefinitionAmount of liabilities and equity items, including the portion of equity attributable to noncontrolling interests, if any. Reference 1: http://www.xbrl.org/2003/role/exampleRef
-Topic 852
-SubTopic 10
-Name Accounting Standards Codification
-Section 55
-Paragraph 10
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147481372/852-10-55-10
Reference 2: http://www.xbrl.org/2003/role/disclosureRef
-Topic 944
-SubTopic 210
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.7-03(a)(25))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147478777/944-210-S99-1
Reference 3: http://www.xbrl.org/2009/role/commonPracticeRef
-Topic 235
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.4-08(g)(1)(ii))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480678/235-10-S99-1
Reference 4: http://www.xbrl.org/2009/role/commonPracticeRef
-Topic 323
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 3
-Subparagraph (c)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147481687/323-10-50-3
Reference 5: http://www.xbrl.org/2009/role/commonPracticeRef
-Topic 825
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 28
-Subparagraph (f)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482907/825-10-50-28
Reference 6: http://fasb.org/us-gaap/role/ref/legacyRef
-Topic 942
-SubTopic 210
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.9-03(23))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147478546/942-210-S99-1
Reference 7: http://fasb.org/us-gaap/role/ref/legacyRef
-Topic 210
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.5-02(32))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480566/210-10-S99-1
| Name: |
us-gaap_LiabilitiesAndStockholdersEquity |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:monetaryItemType |
| Balance Type: |
credit |
| Period Type: |
instant |
|
| X |
- DefinitionTotal obligations incurred as part of normal operations that are expected to be paid during the following twelve months or within one business cycle, if longer. Reference 1: http://fasb.org/us-gaap/role/ref/legacyRef
-Topic 210
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.5-02(21))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480566/210-10-S99-1
Reference 2: http://www.xbrl.org/2003/role/disclosureRef
-Topic 810
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 3
-Subparagraph (c)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147481203/810-10-50-3
Reference 3: http://www.xbrl.org/2003/role/disclosureRef
-Topic 810
-SubTopic 10
-Name Accounting Standards Codification
-Section 45
-Paragraph 25
-Subparagraph (b)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147481231/810-10-45-25
Reference 4: http://www.xbrl.org/2003/role/disclosureRef
-Topic 810
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 3
-Subparagraph (bb)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147481203/810-10-50-3
Reference 5: http://www.xbrl.org/2003/role/disclosureRef
-Topic 235
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.4-08(g)(1)(ii))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480678/235-10-S99-1
Reference 6: http://www.xbrl.org/2003/role/disclosureRef
-Topic 323
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 3
-Subparagraph (c)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147481687/323-10-50-3
Reference 7: http://www.xbrl.org/2003/role/disclosureRef
-Topic 825
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 28
-Subparagraph (f)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482907/825-10-50-28
Reference 8: http://www.xbrl.org/2003/role/exampleRef
-Topic 852
-SubTopic 10
-Name Accounting Standards Codification
-Section 55
-Paragraph 10
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147481372/852-10-55-10
Reference 9: http://www.xbrl.org/2003/role/disclosureRef
-Topic 210
-SubTopic 10
-Name Accounting Standards Codification
-Section 45
-Paragraph 5
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147483467/210-10-45-5
Reference 10: http://www.xbrl.org/2003/role/disclosureRef
-Topic 470
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1A
-Subparagraph (SX 210.13-01(a)(4)(i))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480097/470-10-S99-1A
Reference 11: http://www.xbrl.org/2009/role/commonPracticeRef
-Topic 470
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1A
-Subparagraph (SX 210.13-01(a)(4)(ii))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480097/470-10-S99-1A
Reference 12: http://www.xbrl.org/2003/role/disclosureRef
-Topic 470
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1A
-Subparagraph (SX 210.13-01(a)(4)(iii)(A))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480097/470-10-S99-1A
Reference 13: http://www.xbrl.org/2003/role/disclosureRef
-Topic 470
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1A
-Subparagraph (SX 210.13-01(a)(4)(iv))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480097/470-10-S99-1A
Reference 14: http://www.xbrl.org/2003/role/disclosureRef
-Topic 470
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1A
-Subparagraph (SX 210.13-01(a)(5))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480097/470-10-S99-1A
Reference 15: http://www.xbrl.org/2003/role/disclosureRef
-Topic 470
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1B
-Subparagraph (SX 210.13-02(a)(4)(i))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480097/470-10-S99-1B
Reference 16: http://www.xbrl.org/2003/role/disclosureRef
-Topic 470
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1B
-Subparagraph (SX 210.13-02(a)(4)(iii)(A))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480097/470-10-S99-1B
Reference 17: http://www.xbrl.org/2003/role/disclosureRef
-Topic 470
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1B
-Subparagraph (SX 210.13-02(a)(4)(iii)(B))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480097/470-10-S99-1B
Reference 18: http://www.xbrl.org/2003/role/disclosureRef
-Topic 470
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1B
-Subparagraph (SX 210.13-02(a)(4)(iv))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480097/470-10-S99-1B
Reference 19: http://www.xbrl.org/2003/role/disclosureRef
-Topic 470
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1B
-Subparagraph (SX 210.13-02(a)(5))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480097/470-10-S99-1B
Reference 20: http://www.xbrl.org/2009/role/commonPracticeRef
-Topic 852
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 7
-Subparagraph (a)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147481404/852-10-50-7
Reference 21: http://www.xbrl.org/2009/role/commonPracticeRef
-Topic 852
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 7
-Subparagraph (b)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147481404/852-10-50-7
| Name: |
us-gaap_LiabilitiesCurrent |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:monetaryItemType |
| Balance Type: |
credit |
| Period Type: |
instant |
|
| X |
- References
+ Details
| Name: |
us-gaap_LiabilitiesCurrentAbstract |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:stringItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionAmount, after deduction of unamortized premium (discount) and debt issuance cost, of long-term debt classified as noncurrent. Excludes lease obligation. Reference 1: http://www.xbrl.org/2003/role/disclosureRef
-Topic 210
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.5-02(22))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480566/210-10-S99-1
| Name: |
us-gaap_LongTermDebtNoncurrent |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:monetaryItemType |
| Balance Type: |
credit |
| Period Type: |
instant |
|
| X |
- DefinitionAmount of equity (deficit) attributable to noncontrolling interest. Excludes temporary equity. Reference 1: http://fasb.org/us-gaap/role/ref/legacyRef
-Topic 210
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.5-02(31))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480566/210-10-S99-1
Reference 2: http://www.xbrl.org/2003/role/disclosureRef
-Topic 235
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.4-08(g)(1)(ii))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480678/235-10-S99-1
Reference 3: http://www.xbrl.org/2003/role/disclosureRef
-Topic 323
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 3
-Subparagraph (c)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147481687/323-10-50-3
Reference 4: http://www.xbrl.org/2003/role/disclosureRef
-Topic 825
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 28
-Subparagraph (f)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482907/825-10-50-28
Reference 5: http://www.xbrl.org/2003/role/disclosureRef
-Topic 944
-SubTopic 210
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.7-03(a)(24))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147478777/944-210-S99-1
Reference 6: http://www.xbrl.org/2003/role/disclosureRef
-Topic 946
-SubTopic 210
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.6-04(19))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147479170/946-210-S99-1
Reference 7: http://www.xbrl.org/2003/role/disclosureRef
-Topic 470
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1A
-Subparagraph (SX 210.13-01(a)(4)(i))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480097/470-10-S99-1A
Reference 8: http://www.xbrl.org/2003/role/disclosureRef
-Topic 470
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1A
-Subparagraph (SX 210.13-01(a)(4)(iv))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480097/470-10-S99-1A
Reference 9: http://www.xbrl.org/2003/role/disclosureRef
-Topic 470
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1A
-Subparagraph (SX 210.13-01(a)(5))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480097/470-10-S99-1A
Reference 10: http://www.xbrl.org/2003/role/disclosureRef
-Topic 470
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1B
-Subparagraph (SX 210.13-02(a)(4)(i))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480097/470-10-S99-1B
Reference 11: http://www.xbrl.org/2003/role/disclosureRef
-Topic 470
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1B
-Subparagraph (SX 210.13-02(a)(4)(iv))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480097/470-10-S99-1B
Reference 12: http://www.xbrl.org/2003/role/disclosureRef
-Topic 470
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1B
-Subparagraph (SX 210.13-02(a)(5))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480097/470-10-S99-1B
Reference 13: http://fasb.org/us-gaap/role/ref/legacyRef
-Topic 942
-SubTopic 210
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.9-03(22))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147478546/942-210-S99-1
| Name: |
us-gaap_MinorityInterest |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:monetaryItemType |
| Balance Type: |
credit |
| Period Type: |
instant |
|
| X |
- DefinitionPresent value of lessee's discounted obligation for lease payments from operating lease, classified as noncurrent. Reference 1: http://www.xbrl.org/2003/role/disclosureRef
-Topic 842
-SubTopic 20
-Name Accounting Standards Codification
-Section 45
-Paragraph 1
-Subparagraph (b)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147479041/842-20-45-1
| Name: |
us-gaap_OperatingLeaseLiabilityNoncurrent |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:monetaryItemType |
| Balance Type: |
credit |
| Period Type: |
instant |
|
| X |
- DefinitionAmount of lessee's right to use underlying asset under operating lease. Reference 1: http://www.xbrl.org/2003/role/disclosureRef
-Topic 842
-SubTopic 20
-Name Accounting Standards Codification
-Section 45
-Paragraph 1
-Subparagraph (a)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147479041/842-20-45-1
| Name: |
us-gaap_OperatingLeaseRightOfUseAsset |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:monetaryItemType |
| Balance Type: |
debit |
| Period Type: |
instant |
|
| X |
- DefinitionAmount of noncurrent assets classified as other. Reference 1: http://www.xbrl.org/2003/role/disclosureRef
-Topic 210
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.5-02(17))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480566/210-10-S99-1
| Name: |
us-gaap_OtherAssetsNoncurrent |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:monetaryItemType |
| Balance Type: |
debit |
| Period Type: |
instant |
|
| X |
- DefinitionAggregate par or stated value of issued nonredeemable preferred stock (or preferred stock redeemable solely at the option of the issuer). This item includes treasury stock repurchased by the entity. Note: elements for number of nonredeemable preferred shares, par value and other disclosure concepts are in another section within stockholders' equity. Reference 1: http://fasb.org/us-gaap/role/ref/legacyRef
-Topic 210
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.5-02(28))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480566/210-10-S99-1
Reference 2: http://www.xbrl.org/2003/role/exampleRef
-Topic 852
-SubTopic 10
-Name Accounting Standards Codification
-Section 55
-Paragraph 10
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147481372/852-10-55-10
Reference 3: http://www.xbrl.org/2003/role/disclosureRef
-Topic 944
-SubTopic 210
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.7-03(a)(21))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147478777/944-210-S99-1
| Name: |
us-gaap_PreferredStockValue |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:monetaryItemType |
| Balance Type: |
credit |
| Period Type: |
instant |
|
| X |
- DefinitionAmount of asset related to consideration paid in advance for costs that provide economic benefits in future periods, and amount of other assets that are expected to be realized or consumed within one year or the normal operating cycle, if longer. Reference 1: http://www.xbrl.org/2009/role/commonPracticeRef
-Topic 210
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.5-02(9))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480566/210-10-S99-1
| Name: |
us-gaap_PrepaidExpenseAndOtherAssetsCurrent |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:monetaryItemType |
| Balance Type: |
debit |
| Period Type: |
instant |
|
| X |
- DefinitionAmount after accumulated depreciation, depletion and amortization of physical assets used in the normal conduct of business to produce goods and services and not intended for resale. Examples include, but are not limited to, land, buildings, machinery and equipment, office equipment, and furniture and fixtures. Reference 1: http://fasb.org/us-gaap/role/ref/legacyRef
-Name Accounting Standards Codification
-Section 50
-Paragraph 1
-SubTopic 10
-Topic 360
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482099/360-10-50-1
Reference 2: http://www.xbrl.org/2003/role/disclosureRef
-Topic 842
-SubTopic 20
-Name Accounting Standards Codification
-Section 50
-Paragraph 7A
-Subparagraph (a)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147478964/842-20-50-7A
Reference 3: http://www.xbrl.org/2003/role/exampleRef
-Topic 852
-SubTopic 10
-Name Accounting Standards Codification
-Section 55
-Paragraph 10
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147481372/852-10-55-10
Reference 4: http://www.xbrl.org/2003/role/disclosureRef
-Topic 944
-SubTopic 210
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.7-03(a)(8))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147478777/944-210-S99-1
Reference 5: http://www.xbrl.org/2003/role/disclosureRef
-Topic 942
-SubTopic 360
-Name Accounting Standards Codification
-Section 50
-Paragraph 1
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147478451/942-360-50-1
| Name: |
us-gaap_PropertyPlantAndEquipmentNet |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:monetaryItemType |
| Balance Type: |
debit |
| Period Type: |
instant |
|
| X |
- DefinitionAmount of accumulated undistributed earnings (deficit). Reference 1: http://fasb.org/us-gaap/role/ref/legacyRef
-Topic 210
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.5-02(30)(a)(3))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480566/210-10-S99-1
Reference 2: http://www.xbrl.org/2003/role/exampleRef
-Topic 852
-SubTopic 10
-Name Accounting Standards Codification
-Section 55
-Paragraph 10
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147481372/852-10-55-10
Reference 3: http://www.xbrl.org/2003/role/disclosureRef
-Topic 944
-SubTopic 40
-Name Accounting Standards Codification
-Section 65
-Paragraph 2
-Subparagraph (g)(2)(i)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480016/944-40-65-2
Reference 4: http://www.xbrl.org/2003/role/disclosureRef
-Topic 944
-SubTopic 40
-Name Accounting Standards Codification
-Section 65
-Paragraph 2
-Subparagraph (h)(2)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480016/944-40-65-2
Reference 5: http://www.xbrl.org/2003/role/disclosureRef
-Topic 946
-SubTopic 20
-Name Accounting Standards Codification
-Section 50
-Paragraph 11
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480990/946-20-50-11
Reference 6: http://www.xbrl.org/2003/role/disclosureRef
-Topic 944
-SubTopic 210
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.7-03(a)(23)(a)(4))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147478777/944-210-S99-1
Reference 7: http://www.xbrl.org/2003/role/disclosureRef
-Topic 946
-SubTopic 210
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.6-04(17))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147479170/946-210-S99-1
Reference 8: http://fasb.org/us-gaap/role/ref/legacyRef
-Topic 505
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.3-04)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480008/505-10-S99-1
| Name: |
us-gaap_RetainedEarningsAccumulatedDeficit |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:monetaryItemType |
| Balance Type: |
credit |
| Period Type: |
instant |
|
| X |
- DefinitionAmount of investments including trading securities, available-for-sale securities, held-to-maturity securities, and short-term investments classified as other and current. Reference 1: http://fasb.org/us-gaap/role/ref/legacyRef
-Topic 942
-SubTopic 210
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.9-03(4))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147478546/942-210-S99-1
Reference 2: http://fasb.org/us-gaap/role/ref/legacyRef
-Topic 942
-SubTopic 210
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.9-03(5))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147478546/942-210-S99-1
Reference 3: http://www.xbrl.org/2009/role/commonPracticeRef
-Topic 210
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.5-02(8))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480566/210-10-S99-1
| Name: |
us-gaap_ShortTermInvestments |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:monetaryItemType |
| Balance Type: |
debit |
| Period Type: |
instant |
|
| X |
- DefinitionAmount of equity (deficit) attributable to parent. Excludes temporary equity and equity attributable to noncontrolling interest. Reference 1: http://fasb.org/us-gaap/role/ref/legacyRef
-Topic 210
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.5-02(29))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480566/210-10-S99-1
Reference 2: http://fasb.org/us-gaap/role/ref/legacyRef
-Topic 210
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.5-02(30))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480566/210-10-S99-1
Reference 3: http://fasb.org/us-gaap/role/ref/legacyRef
-Topic 210
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.5-02(31))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480566/210-10-S99-1
Reference 4: http://www.xbrl.org/2003/role/exampleRef
-Topic 852
-SubTopic 10
-Name Accounting Standards Codification
-Section 55
-Paragraph 10
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147481372/852-10-55-10
Reference 5: http://www.xbrl.org/2003/role/exampleRef
-Topic 946
-SubTopic 830
-Name Accounting Standards Codification
-Section 55
-Paragraph 12
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147479168/946-830-55-12
Reference 6: http://www.xbrl.org/2003/role/disclosureRef
-Topic 946
-SubTopic 210
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.6-04(19))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147479170/946-210-S99-1
Reference 7: http://www.xbrl.org/2003/role/disclosureRef
-Topic 946
-SubTopic 210
-Name Accounting Standards Codification
-Section S99
-Paragraph 2
-Subparagraph (SX 210.6-05(4))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147479170/946-210-S99-2
Reference 8: http://www.xbrl.org/2009/role/commonPracticeRef
-Topic 946
-SubTopic 220
-Name Accounting Standards Codification
-Section S99
-Paragraph 3
-Subparagraph (SX 210.6-09(4)(b))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147479134/946-220-S99-3
Reference 9: http://www.xbrl.org/2003/role/disclosureRef
-Topic 946
-SubTopic 220
-Name Accounting Standards Codification
-Section S99
-Paragraph 3
-Subparagraph (SX 210.6-09(6))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147479134/946-220-S99-3
Reference 10: http://www.xbrl.org/2003/role/disclosureRef
-Topic 946
-SubTopic 220
-Name Accounting Standards Codification
-Section S99
-Paragraph 3
-Subparagraph (SX 210.6-09(7))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147479134/946-220-S99-3
Reference 11: http://www.xbrl.org/2009/role/commonPracticeRef
-Topic 235
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.4-08(g)(1)(ii))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480678/235-10-S99-1
Reference 12: http://www.xbrl.org/2009/role/commonPracticeRef
-Topic 323
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 3
-Subparagraph (c)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147481687/323-10-50-3
Reference 13: http://www.xbrl.org/2009/role/commonPracticeRef
-Topic 825
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 28
-Subparagraph (f)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482907/825-10-50-28
Reference 14: http://fasb.org/us-gaap/role/ref/legacyRef
-Topic 310
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 2
-Subparagraph (SAB Topic 4.E)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480418/310-10-S99-2
| Name: |
us-gaap_StockholdersEquity |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:monetaryItemType |
| Balance Type: |
credit |
| Period Type: |
instant |
|
| X |
- References
+ Details
| Name: |
us-gaap_StockholdersEquityAbstract |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:stringItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionAmount of equity (deficit) attributable to parent and noncontrolling interest. Excludes temporary equity. Reference 1: http://www.xbrl.org/2003/role/disclosureRef
-Topic 250
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 6
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147483443/250-10-50-6
Reference 2: http://www.xbrl.org/2003/role/disclosureRef
-Topic 805
-SubTopic 60
-Name Accounting Standards Codification
-Section 65
-Paragraph 1
-Subparagraph (g)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147476176/805-60-65-1
Reference 3: http://www.xbrl.org/2003/role/disclosureRef
-Topic 805
-SubTopic 60
-Name Accounting Standards Codification
-Section 65
-Paragraph 1
-Subparagraph (d)(1)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147476176/805-60-65-1
Reference 4: http://www.xbrl.org/2003/role/disclosureRef
-Topic 740
-SubTopic 323
-Name Accounting Standards Codification
-Section 65
-Paragraph 2
-Subparagraph (e)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147478666/740-323-65-2
Reference 5: http://www.xbrl.org/2003/role/disclosureRef
-Topic 740
-SubTopic 323
-Name Accounting Standards Codification
-Section 65
-Paragraph 2
-Subparagraph (g)(4)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147478666/740-323-65-2
Reference 6: http://www.xbrl.org/2003/role/disclosureRef
-Topic 740
-SubTopic 323
-Name Accounting Standards Codification
-Section 65
-Paragraph 2
-Subparagraph (d)(2)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147478666/740-323-65-2
Reference 7: http://www.xbrl.org/2003/role/disclosureRef
-Topic 740
-SubTopic 323
-Name Accounting Standards Codification
-Section 65
-Paragraph 2
-Subparagraph (d)(1)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147478666/740-323-65-2
Reference 8: http://www.xbrl.org/2003/role/disclosureRef
-Topic 848
-SubTopic 10
-Name Accounting Standards Codification
-Section 65
-Paragraph 2
-Subparagraph (a)(3)(iii)(03)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147483550/848-10-65-2
Reference 9: http://www.xbrl.org/2003/role/disclosureRef
-Topic 842
-SubTopic 10
-Name Accounting Standards Codification
-Section 65
-Paragraph 8
-Subparagraph (c)(3)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147479832/842-10-65-8
Reference 10: http://www.xbrl.org/2003/role/disclosureRef
-Topic 250
-SubTopic 10
-Name Accounting Standards Codification
-Section 45
-Paragraph 24
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147483421/250-10-45-24
Reference 11: http://www.xbrl.org/2003/role/disclosureRef
-Topic 250
-SubTopic 10
-Name Accounting Standards Codification
-Section 45
-Paragraph 23
-Subparagraph (b)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147483421/250-10-45-23
Reference 12: http://www.xbrl.org/2003/role/disclosureRef
-Topic 250
-SubTopic 10
-Name Accounting Standards Codification
-Section 45
-Paragraph 5
-Subparagraph (b)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147483421/250-10-45-5
Reference 13: http://www.xbrl.org/2003/role/disclosureRef
-Topic 326
-SubTopic 10
-Name Accounting Standards Codification
-Section 65
-Paragraph 5
-Subparagraph (c)(2)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147479654/326-10-65-5
Reference 14: http://www.xbrl.org/2003/role/disclosureRef
-Topic 815
-SubTopic 20
-Name Accounting Standards Codification
-Section 65
-Paragraph 6
-Subparagraph (e)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480528/815-20-65-6
Reference 15: http://www.xbrl.org/2003/role/disclosureRef
-Topic 815
-SubTopic 20
-Name Accounting Standards Codification
-Section 65
-Paragraph 6
-Subparagraph (h)(1)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480528/815-20-65-6
Reference 16: http://www.xbrl.org/2003/role/disclosureRef
-Topic 815
-SubTopic 20
-Name Accounting Standards Codification
-Section 65
-Paragraph 6
-Subparagraph (h)(1)(i)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480528/815-20-65-6
Reference 17: http://www.xbrl.org/2003/role/disclosureRef
-Topic 815
-SubTopic 20
-Name Accounting Standards Codification
-Section 65
-Paragraph 6
-Subparagraph (h)(1)(iii)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480528/815-20-65-6
Reference 18: http://www.xbrl.org/2003/role/disclosureRef
-Topic 815
-SubTopic 20
-Name Accounting Standards Codification
-Section 65
-Paragraph 6
-Subparagraph (h)(1)(iv)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480528/815-20-65-6
Reference 19: http://www.xbrl.org/2003/role/disclosureRef
-Topic 815
-SubTopic 20
-Name Accounting Standards Codification
-Section 65
-Paragraph 6
-Subparagraph (i)(3)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480528/815-20-65-6
Reference 20: http://www.xbrl.org/2003/role/disclosureRef
-Topic 105
-SubTopic 10
-Name Accounting Standards Codification
-Section 65
-Paragraph 6
-Subparagraph (c)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147479343/105-10-65-6
Reference 21: http://www.xbrl.org/2003/role/disclosureRef
-Topic 105
-SubTopic 10
-Name Accounting Standards Codification
-Section 65
-Paragraph 6
-Subparagraph (d)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147479343/105-10-65-6
Reference 22: http://www.xbrl.org/2003/role/disclosureRef
-Topic 944
-SubTopic 40
-Name Accounting Standards Codification
-Section 65
-Paragraph 2
-Subparagraph (f)(1)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480016/944-40-65-2
Reference 23: http://www.xbrl.org/2003/role/disclosureRef
-Topic 944
-SubTopic 40
-Name Accounting Standards Codification
-Section 65
-Paragraph 2
-Subparagraph (f)(2)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480016/944-40-65-2
Reference 24: http://www.xbrl.org/2003/role/disclosureRef
-Topic 740
-SubTopic 10
-Name Accounting Standards Codification
-Section 65
-Paragraph 8
-Subparagraph (d)(2)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482615/740-10-65-8
Reference 25: http://www.xbrl.org/2003/role/disclosureRef
-Topic 740
-SubTopic 10
-Name Accounting Standards Codification
-Section 65
-Paragraph 8
-Subparagraph (d)(3)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482615/740-10-65-8
Reference 26: http://www.xbrl.org/2003/role/disclosureRef
-Topic 326
-SubTopic 10
-Name Accounting Standards Codification
-Section 65
-Paragraph 4
-Subparagraph (d)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147479654/326-10-65-4
Reference 27: http://www.xbrl.org/2003/role/disclosureRef
-Topic 250
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 1
-Subparagraph (b)(3)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147483443/250-10-50-1
Reference 28: http://www.xbrl.org/2003/role/disclosureRef
-Topic 815
-SubTopic 40
-Name Accounting Standards Codification
-Section 65
-Paragraph 1
-Subparagraph (e)(3)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480175/815-40-65-1
Reference 29: http://www.xbrl.org/2003/role/disclosureRef
-Topic 250
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 7
-Subparagraph (b)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147483443/250-10-50-7
Reference 30: http://www.xbrl.org/2003/role/disclosureRef
-Topic 220
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 5
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482765/220-10-50-5
Reference 31: http://www.xbrl.org/2003/role/disclosureRef
-Topic 830
-SubTopic 30
-Name Accounting Standards Codification
-Section 50
-Paragraph 1
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147481674/830-30-50-1
Reference 32: http://www.xbrl.org/2003/role/disclosureRef
-Topic 830
-SubTopic 30
-Name Accounting Standards Codification
-Section 45
-Paragraph 17
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147481694/830-30-45-17
Reference 33: http://www.xbrl.org/2003/role/disclosureRef
-Topic 830
-SubTopic 30
-Name Accounting Standards Codification
-Section 45
-Paragraph 20
-Subparagraph (a)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147481694/830-30-45-20
Reference 34: http://www.xbrl.org/2003/role/exampleRef
-Topic 946
-SubTopic 830
-Name Accounting Standards Codification
-Section 55
-Paragraph 11
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147479168/946-830-55-11
Reference 35: http://www.xbrl.org/2003/role/disclosureRef
-Topic 946
-SubTopic 205
-Name Accounting Standards Codification
-Section 45
-Paragraph 3
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147478009/946-205-45-3
Reference 36: http://www.xbrl.org/2003/role/disclosureRef
-Topic 946
-SubTopic 505
-Name Accounting Standards Codification
-Section 50
-Paragraph 3
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147478448/946-505-50-3
Reference 37: http://www.xbrl.org/2003/role/disclosureRef
-Topic 946
-SubTopic 210
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.6-04(19))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147479170/946-210-S99-1
Reference 38: http://www.xbrl.org/2003/role/disclosureRef
-Topic 946
-SubTopic 210
-Name Accounting Standards Codification
-Section S99
-Paragraph 2
-Subparagraph (SX 210.6-05(4))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147479170/946-210-S99-2
Reference 39: http://www.xbrl.org/2009/role/commonPracticeRef
-Topic 946
-SubTopic 220
-Name Accounting Standards Codification
-Section S99
-Paragraph 3
-Subparagraph (SX 210.6-09(4)(b))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147479134/946-220-S99-3
Reference 40: http://www.xbrl.org/2003/role/disclosureRef
-Topic 946
-SubTopic 220
-Name Accounting Standards Codification
-Section S99
-Paragraph 3
-Subparagraph (SX 210.6-09(6))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147479134/946-220-S99-3
Reference 41: http://www.xbrl.org/2003/role/disclosureRef
-Topic 946
-SubTopic 220
-Name Accounting Standards Codification
-Section S99
-Paragraph 3
-Subparagraph (SX 210.6-09(7))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147479134/946-220-S99-3
Reference 42: http://www.xbrl.org/2003/role/disclosureRef
-Topic 505
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.3-04)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480008/505-10-S99-1
Reference 43: http://www.xbrl.org/2009/role/commonPracticeRef
-Topic 235
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.4-08(g)(1)(ii))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480678/235-10-S99-1
Reference 44: http://www.xbrl.org/2009/role/commonPracticeRef
-Topic 323
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 3
-Subparagraph (c)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147481687/323-10-50-3
Reference 45: http://www.xbrl.org/2009/role/commonPracticeRef
-Topic 825
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 28
-Subparagraph (f)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482907/825-10-50-28
Reference 46: http://fasb.org/us-gaap/role/ref/legacyRef
-Name Accounting Standards Codification
-Topic 810
-SubTopic 10
-Section 45
-Paragraph 15
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147481231/810-10-45-15
Reference 47: http://fasb.org/us-gaap/role/ref/legacyRef
-Name Accounting Standards Codification
-Topic 810
-SubTopic 10
-Section 45
-Paragraph 16
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147481231/810-10-45-16
Reference 48: http://fasb.org/us-gaap/role/ref/legacyRef
-Name Accounting Standards Codification
-Topic 810
-SubTopic 10
-Section 55
-Paragraph 4I
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147481175/810-10-55-4I
Reference 49: http://www.xbrl.org/2003/role/disclosureRef
-Topic 350
-SubTopic 60
-Name Accounting Standards Codification
-Section 65
-Paragraph 1
-Subparagraph (b)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147476166/350-60-65-1
| Name: |
us-gaap_StockholdersEquityIncludingPortionAttributableToNoncontrollingInterest |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:monetaryItemType |
| Balance Type: |
credit |
| Period Type: |
instant |
|
v3.24.2.u1
Condensed Consolidated Balance Sheets (Parenthetical) - USD ($)
$ in Thousands |
Jun. 30, 2024 |
Dec. 31, 2023 |
| Statement of Financial Position [Abstract] |
|
|
| Allowance for credit losses |
$ 95
|
$ 0
|
| Preferred stock par value (in dollars per share) |
$ 0.001
|
$ 0.001
|
| Preferred stock, shares authorized (in shares) |
100,000,000
|
100,000,000
|
| Preferred stock, shares issued (in shares) |
0
|
0
|
| Preferred stock, shares outstanding (in shares) |
0
|
0
|
| Common stock, par value (in dollars per share) |
$ 0.001
|
$ 0.001
|
| Common stock, shares authorized (in shares) |
1,000,000,000
|
1,000,000,000
|
| Common stock, shares issued (in shares) |
191,236,747
|
188,951,643
|
| Common stock, shares outstanding (in shares) |
191,236,747
|
188,951,643
|
| X |
- DefinitionAmount of allowance for credit loss on accounts receivable, classified as current. Reference 1: http://www.xbrl.org/2003/role/disclosureRef
-Topic 210
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.5-02(4))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480566/210-10-S99-1
Reference 2: http://www.xbrl.org/2003/role/disclosureRef
-Topic 326
-SubTopic 20
-Name Accounting Standards Codification
-Section 45
-Paragraph 1
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147479344/326-20-45-1
Reference 3: http://www.xbrl.org/2003/role/disclosureRef
-Topic 310
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 4
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147481962/310-10-50-4
| Name: |
us-gaap_AllowanceForDoubtfulAccountsReceivableCurrent |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:monetaryItemType |
| Balance Type: |
credit |
| Period Type: |
instant |
|
| X |
- DefinitionFace amount or stated value per share of common stock. Reference 1: http://fasb.org/us-gaap/role/ref/legacyRef
-Topic 210
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.5-02(29))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480566/210-10-S99-1
| Name: |
us-gaap_CommonStockParOrStatedValuePerShare |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
dtr-types:perShareItemType |
| Balance Type: |
na |
| Period Type: |
instant |
|
| X |
- DefinitionThe maximum number of common shares permitted to be issued by an entity's charter and bylaws. Reference 1: http://fasb.org/us-gaap/role/ref/legacyRef
-Topic 210
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.5-02(29))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480566/210-10-S99-1
Reference 2: http://www.xbrl.org/2003/role/disclosureRef
-Topic 946
-SubTopic 210
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.6-04(16)(a))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147479170/946-210-S99-1
| Name: |
us-gaap_CommonStockSharesAuthorized |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:sharesItemType |
| Balance Type: |
na |
| Period Type: |
instant |
|
| X |
- DefinitionTotal number of common shares of an entity that have been sold or granted to shareholders (includes common shares that were issued, repurchased and remain in the treasury). These shares represent capital invested by the firm's shareholders and owners, and may be all or only a portion of the number of shares authorized. Shares issued include shares outstanding and shares held in the treasury. Reference 1: http://fasb.org/us-gaap/role/ref/legacyRef
-Topic 210
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.5-02(29))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480566/210-10-S99-1
| Name: |
us-gaap_CommonStockSharesIssued |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:sharesItemType |
| Balance Type: |
na |
| Period Type: |
instant |
|
| X |
- DefinitionNumber of shares of common stock outstanding. Common stock represent the ownership interest in a corporation. Reference 1: http://fasb.org/us-gaap/role/ref/legacyRef
-Name Accounting Standards Codification
-Section 50
-Paragraph 2
-SubTopic 10
-Topic 505
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147481112/505-10-50-2
Reference 2: http://fasb.org/us-gaap/role/ref/legacyRef
-Topic 210
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.5-02(29))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480566/210-10-S99-1
Reference 3: http://www.xbrl.org/2003/role/disclosureRef
-Topic 946
-SubTopic 210
-Name Accounting Standards Codification
-Section S99
-Paragraph 2
-Subparagraph (SX 210.6-05(4))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147479170/946-210-S99-2
Reference 4: http://www.xbrl.org/2009/role/commonPracticeRef
-Topic 946
-SubTopic 220
-Name Accounting Standards Codification
-Section S99
-Paragraph 3
-Subparagraph (SX 210.6-09(4)(b))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147479134/946-220-S99-3
Reference 5: http://www.xbrl.org/2003/role/disclosureRef
-Topic 946
-SubTopic 210
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.6-04(16)(a))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147479170/946-210-S99-1
Reference 6: http://www.xbrl.org/2009/role/commonPracticeRef
-Topic 946
-SubTopic 220
-Name Accounting Standards Codification
-Section S99
-Paragraph 3
-Subparagraph (SX 210.6-09(7))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147479134/946-220-S99-3
| Name: |
us-gaap_CommonStockSharesOutstanding |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:sharesItemType |
| Balance Type: |
na |
| Period Type: |
instant |
|
| X |
- DefinitionFace amount or stated value per share of preferred stock nonredeemable or redeemable solely at the option of the issuer. Reference 1: http://fasb.org/us-gaap/role/ref/legacyRef
-Topic 210
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.5-02(28))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480566/210-10-S99-1
Reference 2: http://www.xbrl.org/2003/role/disclosureRef
-Topic 505
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 13
-Subparagraph (a)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147481112/505-10-50-13
| Name: |
us-gaap_PreferredStockParOrStatedValuePerShare |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
dtr-types:perShareItemType |
| Balance Type: |
na |
| Period Type: |
instant |
|
| X |
- DefinitionThe maximum number of nonredeemable preferred shares (or preferred stock redeemable solely at the option of the issuer) permitted to be issued by an entity's charter and bylaws. Reference 1: http://fasb.org/us-gaap/role/ref/legacyRef
-Topic 210
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.5-02(28))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480566/210-10-S99-1
Reference 2: http://www.xbrl.org/2003/role/disclosureRef
-Topic 946
-SubTopic 210
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.6-04(16)(a))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147479170/946-210-S99-1
| Name: |
us-gaap_PreferredStockSharesAuthorized |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:sharesItemType |
| Balance Type: |
na |
| Period Type: |
instant |
|
| X |
- DefinitionNumber of shares issued for nonredeemable preferred shares and preferred shares redeemable solely at option of issuer. Includes, but is not limited to, preferred shares issued, repurchased, and held as treasury shares. Excludes preferred shares classified as debt. Reference 1: http://fasb.org/us-gaap/role/ref/legacyRef
-Topic 210
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.5-02(28))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480566/210-10-S99-1
Reference 2: http://www.xbrl.org/2003/role/disclosureRef
-Topic 505
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 13
-Subparagraph (a)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147481112/505-10-50-13
| Name: |
us-gaap_PreferredStockSharesIssued |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:sharesItemType |
| Balance Type: |
na |
| Period Type: |
instant |
|
| X |
- DefinitionAggregate share number for all nonredeemable preferred stock (or preferred stock redeemable solely at the option of the issuer) held by stockholders. Does not include preferred shares that have been repurchased. Reference 1: http://fasb.org/us-gaap/role/ref/legacyRef
-Topic 210
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.5-02(28))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480566/210-10-S99-1
Reference 2: http://www.xbrl.org/2003/role/disclosureRef
-Topic 946
-SubTopic 210
-Name Accounting Standards Codification
-Section S99
-Paragraph 2
-Subparagraph (SX 210.6-05(4))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147479170/946-210-S99-2
Reference 3: http://www.xbrl.org/2009/role/commonPracticeRef
-Topic 946
-SubTopic 220
-Name Accounting Standards Codification
-Section S99
-Paragraph 3
-Subparagraph (SX 210.6-09(4)(b))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147479134/946-220-S99-3
Reference 4: http://www.xbrl.org/2003/role/disclosureRef
-Topic 946
-SubTopic 210
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.6-04(16)(a))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147479170/946-210-S99-1
Reference 5: http://www.xbrl.org/2009/role/commonPracticeRef
-Topic 946
-SubTopic 220
-Name Accounting Standards Codification
-Section S99
-Paragraph 3
-Subparagraph (SX 210.6-09(7))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147479134/946-220-S99-3
| Name: |
us-gaap_PreferredStockSharesOutstanding |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:sharesItemType |
| Balance Type: |
na |
| Period Type: |
instant |
|
| X |
- References
+ Details
| Name: |
us-gaap_StatementOfFinancialPositionAbstract |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:stringItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
v3.24.2.u1
Condensed Consolidated Statements of Operations - USD ($)
$ in Thousands |
3 Months Ended |
6 Months Ended |
Jun. 30, 2024 |
Jun. 30, 2023 |
Jun. 30, 2024 |
Jun. 30, 2023 |
| Revenues: |
|
|
|
|
| Earned premiums |
$ 674,094
|
$ 456,877
|
$ 1,295,650
|
$ 891,689
|
| Other Income |
7,192
|
5,502
|
14,237
|
9,845
|
| Total revenues |
681,286
|
462,379
|
1,309,887
|
901,534
|
| Expenses: |
|
|
|
|
| Medical expenses |
605,312
|
410,644
|
1,178,530
|
806,959
|
| Selling, general, and administrative expenses |
87,863
|
70,199
|
178,375
|
140,607
|
| Depreciation and amortization |
6,493
|
5,195
|
12,470
|
10,116
|
| Total expenses |
699,668
|
486,038
|
1,369,375
|
957,682
|
| Loss from operations |
(18,382)
|
(23,659)
|
(59,488)
|
(56,148)
|
| Other expenses: |
|
|
|
|
| Interest expense |
5,691
|
5,262
|
11,118
|
10,281
|
| Other income, net |
(92)
|
(428)
|
(50)
|
(566)
|
| Total other expenses |
(5,599)
|
(4,834)
|
(11,068)
|
(9,715)
|
| Loss before income taxes |
(23,981)
|
(28,493)
|
(70,556)
|
(65,863)
|
| Provision for income taxes |
22
|
1
|
22
|
2
|
| Net loss |
(24,003)
|
(28,494)
|
(70,578)
|
(65,865)
|
| Less: Net (income) loss attributable to noncontrolling interest |
(7)
|
17
|
47
|
104
|
| Net loss attributable to Alignment Healthcare, Inc. |
$ (24,010)
|
$ (28,477)
|
$ (70,531)
|
$ (65,761)
|
| Total weighted-average common shares outstanding - basic (in shares) |
190,891,787
|
185,991,460
|
189,948,725
|
184,560,652
|
| Total weighted-average common shares outstanding - diluted (in shares) |
190,891,787
|
185,991,460
|
189,948,725
|
184,560,652
|
| Net loss per share - basic (in dollars per share) |
$ (0.13)
|
$ (0.15)
|
$ (0.37)
|
$ (0.36)
|
| Net loss per share - diluted (in dollars per share) |
$ (0.13)
|
$ (0.15)
|
$ (0.37)
|
$ (0.36)
|
| X |
- DefinitionThe aggregate expense recognized in the current period that allocates the cost of tangible assets, intangible assets, or depleting assets to periods that benefit from use of the assets. Reference 1: http://fasb.org/us-gaap/role/ref/legacyRef
-Name Accounting Standards Codification
-Section 45
-Paragraph 28
-Subparagraph (b)
-SubTopic 10
-Topic 230
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482740/230-10-45-28
Reference 2: http://www.xbrl.org/2003/role/exampleRef
-Topic 280
-SubTopic 10
-Name Accounting Standards Codification
-Section 55
-Paragraph 48
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482785/280-10-55-48
Reference 3: http://www.xbrl.org/2003/role/exampleRef
-Topic 280
-SubTopic 10
-Name Accounting Standards Codification
-Section 55
-Paragraph 49
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482785/280-10-55-49
Reference 4: http://www.xbrl.org/2003/role/disclosureRef
-Topic 270
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 1
-Subparagraph (i)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482964/270-10-50-1
Reference 5: http://www.xbrl.org/2003/role/disclosureRef
-Topic 280
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 32
-Subparagraph (ee)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482810/280-10-50-32
Reference 6: http://www.xbrl.org/2003/role/disclosureRef
-Topic 280
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 22
-Subparagraph (e)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482810/280-10-50-22
| Name: |
us-gaap_DepreciationDepletionAndAmortization |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:monetaryItemType |
| Balance Type: |
debit |
| Period Type: |
duration |
|
| X |
- DefinitionThe amount of net income (loss) for the period per each share of common stock or unit outstanding during the reporting period. Reference 1: http://www.xbrl.org/2003/role/disclosureRef
-Topic 250
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 6
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147483443/250-10-50-6
Reference 2: http://www.xbrl.org/2003/role/exampleRef
-Topic 260
-SubTopic 10
-Name Accounting Standards Codification
-Section 55
-Paragraph 52
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482635/260-10-55-52
Reference 3: http://www.xbrl.org/2003/role/disclosureRef
-Topic 805
-SubTopic 60
-Name Accounting Standards Codification
-Section 65
-Paragraph 1
-Subparagraph (g)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147476176/805-60-65-1
Reference 4: http://www.xbrl.org/2003/role/disclosureRef
-Topic 740
-SubTopic 323
-Name Accounting Standards Codification
-Section 65
-Paragraph 2
-Subparagraph (g)(3)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147478666/740-323-65-2
Reference 5: http://www.xbrl.org/2003/role/disclosureRef
-Topic 250
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 3
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147483443/250-10-50-3
Reference 6: http://www.xbrl.org/2003/role/disclosureRef
-Topic 260
-SubTopic 10
-Name Accounting Standards Codification
-Section 55
-Paragraph 15
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482635/260-10-55-15
Reference 7: http://www.xbrl.org/2003/role/disclosureRef
-Topic 815
-SubTopic 40
-Name Accounting Standards Codification
-Section 65
-Paragraph 1
-Subparagraph (e)(4)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480175/815-40-65-1
Reference 8: http://www.xbrl.org/2003/role/disclosureRef
-Topic 815
-SubTopic 40
-Name Accounting Standards Codification
-Section 65
-Paragraph 1
-Subparagraph (f)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480175/815-40-65-1
Reference 9: http://www.xbrl.org/2003/role/disclosureRef
-Topic 250
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 11
-Subparagraph (a)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147483443/250-10-50-11
Reference 10: http://www.xbrl.org/2003/role/disclosureRef
-Topic 250
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 11
-Subparagraph (b)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147483443/250-10-50-11
Reference 11: http://www.xbrl.org/2003/role/disclosureRef
-Topic 250
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 7
-Subparagraph (a)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147483443/250-10-50-7
Reference 12: http://www.xbrl.org/2003/role/disclosureRef
-Topic 260
-SubTopic 10
-Name Accounting Standards Codification
-Section 45
-Paragraph 2
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482689/260-10-45-2
Reference 13: http://www.xbrl.org/2003/role/disclosureRef
-Topic 260
-SubTopic 10
-Name Accounting Standards Codification
-Section 45
-Paragraph 60B
-Subparagraph (d)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482689/260-10-45-60B
Reference 14: http://www.xbrl.org/2003/role/disclosureRef
-Topic 250
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 4
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147483443/250-10-50-4
Reference 15: http://www.xbrl.org/2003/role/disclosureRef
-Topic 260
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 1
-Subparagraph (a)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482662/260-10-50-1
Reference 16: http://www.xbrl.org/2003/role/disclosureRef
-Topic 260
-SubTopic 10
-Name Accounting Standards Codification
-Section 45
-Paragraph 10
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482689/260-10-45-10
Reference 17: http://www.xbrl.org/2003/role/disclosureRef
-Topic 220
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 2
-Subparagraph (SX 210.5-03(25))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147483621/220-10-S99-2
Reference 18: http://www.xbrl.org/2003/role/disclosureRef
-Topic 942
-SubTopic 220
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.9-04(27))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147478524/942-220-S99-1
Reference 19: http://www.xbrl.org/2003/role/disclosureRef
-Topic 944
-SubTopic 220
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.7-04(23))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147477250/944-220-S99-1
Reference 20: http://www.xbrl.org/2003/role/disclosureRef
-Topic 260
-SubTopic 10
-Name Accounting Standards Codification
-Section 45
-Paragraph 7
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482689/260-10-45-7
| Name: |
us-gaap_EarningsPerShareBasic |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
dtr-types:perShareItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionThe amount of net income (loss) for the period available to each share of common stock or common unit outstanding during the reporting period and to each share or unit that would have been outstanding assuming the issuance of common shares or units for all dilutive potential common shares or units outstanding during the reporting period. Reference 1: http://www.xbrl.org/2003/role/disclosureRef
-Topic 250
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 6
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147483443/250-10-50-6
Reference 2: http://www.xbrl.org/2003/role/exampleRef
-Topic 260
-SubTopic 10
-Name Accounting Standards Codification
-Section 55
-Paragraph 52
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482635/260-10-55-52
Reference 3: http://www.xbrl.org/2003/role/disclosureRef
-Topic 805
-SubTopic 60
-Name Accounting Standards Codification
-Section 65
-Paragraph 1
-Subparagraph (g)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147476176/805-60-65-1
Reference 4: http://www.xbrl.org/2003/role/disclosureRef
-Topic 740
-SubTopic 323
-Name Accounting Standards Codification
-Section 65
-Paragraph 2
-Subparagraph (g)(3)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147478666/740-323-65-2
Reference 5: http://www.xbrl.org/2003/role/disclosureRef
-Topic 250
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 3
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147483443/250-10-50-3
Reference 6: http://www.xbrl.org/2003/role/disclosureRef
-Topic 260
-SubTopic 10
-Name Accounting Standards Codification
-Section 55
-Paragraph 15
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482635/260-10-55-15
Reference 7: http://www.xbrl.org/2003/role/disclosureRef
-Topic 815
-SubTopic 40
-Name Accounting Standards Codification
-Section 65
-Paragraph 1
-Subparagraph (e)(4)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480175/815-40-65-1
Reference 8: http://www.xbrl.org/2003/role/disclosureRef
-Topic 815
-SubTopic 40
-Name Accounting Standards Codification
-Section 65
-Paragraph 1
-Subparagraph (f)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480175/815-40-65-1
Reference 9: http://www.xbrl.org/2003/role/disclosureRef
-Topic 250
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 11
-Subparagraph (a)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147483443/250-10-50-11
Reference 10: http://www.xbrl.org/2003/role/disclosureRef
-Topic 250
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 11
-Subparagraph (b)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147483443/250-10-50-11
Reference 11: http://www.xbrl.org/2003/role/disclosureRef
-Topic 250
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 7
-Subparagraph (a)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147483443/250-10-50-7
Reference 12: http://www.xbrl.org/2003/role/disclosureRef
-Topic 260
-SubTopic 10
-Name Accounting Standards Codification
-Section 45
-Paragraph 2
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482689/260-10-45-2
Reference 13: http://www.xbrl.org/2003/role/disclosureRef
-Topic 260
-SubTopic 10
-Name Accounting Standards Codification
-Section 45
-Paragraph 60B
-Subparagraph (d)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482689/260-10-45-60B
Reference 14: http://www.xbrl.org/2003/role/disclosureRef
-Topic 250
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 4
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147483443/250-10-50-4
Reference 15: http://www.xbrl.org/2003/role/disclosureRef
-Topic 260
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 1
-Subparagraph (a)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482662/260-10-50-1
Reference 16: http://www.xbrl.org/2003/role/disclosureRef
-Topic 220
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 2
-Subparagraph (SX 210.5-03(25))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147483621/220-10-S99-2
Reference 17: http://www.xbrl.org/2003/role/disclosureRef
-Topic 942
-SubTopic 220
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.9-04(27))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147478524/942-220-S99-1
Reference 18: http://www.xbrl.org/2003/role/disclosureRef
-Topic 944
-SubTopic 220
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.7-04(23))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147477250/944-220-S99-1
Reference 19: http://www.xbrl.org/2003/role/disclosureRef
-Topic 260
-SubTopic 10
-Name Accounting Standards Codification
-Section 45
-Paragraph 7
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482689/260-10-45-7
| Name: |
us-gaap_EarningsPerShareDiluted |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
dtr-types:perShareItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionAmount of interest expense classified as nonoperating. Reference 1: http://www.xbrl.org/2003/role/disclosureRef
-Topic 280
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 22
-Subparagraph (d)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482810/280-10-50-22
Reference 2: http://www.xbrl.org/2009/role/commonPracticeRef
-Topic 220
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 2
-Subparagraph (SX 210.5-03)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147483621/220-10-S99-2
| Name: |
us-gaap_InterestExpenseNonoperating |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:monetaryItemType |
| Balance Type: |
debit |
| Period Type: |
duration |
|
| X |
- DefinitionThe portion of profit or loss for the period, net of income taxes, which is attributable to the parent. Reference 1: http://www.xbrl.org/2003/role/disclosureRef
-Topic 250
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 6
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147483443/250-10-50-6
Reference 2: http://www.xbrl.org/2003/role/disclosureRef
-Topic 250
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 9
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147483443/250-10-50-9
Reference 3: http://www.xbrl.org/2003/role/disclosureRef
-Topic 805
-SubTopic 60
-Name Accounting Standards Codification
-Section 65
-Paragraph 1
-Subparagraph (g)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147476176/805-60-65-1
Reference 4: http://www.xbrl.org/2003/role/disclosureRef
-Topic 740
-SubTopic 323
-Name Accounting Standards Codification
-Section 65
-Paragraph 2
-Subparagraph (g)(3)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147478666/740-323-65-2
Reference 5: http://fasb.org/us-gaap/role/ref/legacyRef
-Topic 220
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 2
-Subparagraph (SX 210.5-03(20))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147483621/220-10-S99-2
Reference 6: http://www.xbrl.org/2003/role/disclosureRef
-Topic 235
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.4-08(g)(1)(ii))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480678/235-10-S99-1
Reference 7: http://www.xbrl.org/2003/role/disclosureRef
-Topic 323
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 3
-Subparagraph (c)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147481687/323-10-50-3
Reference 8: http://www.xbrl.org/2003/role/disclosureRef
-Topic 825
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 28
-Subparagraph (f)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482907/825-10-50-28
Reference 9: http://www.xbrl.org/2003/role/disclosureRef
-Topic 220
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 6
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482765/220-10-50-6
Reference 10: http://www.xbrl.org/2003/role/disclosureRef
-Topic 250
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 3
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147483443/250-10-50-3
Reference 11: http://www.xbrl.org/2003/role/disclosureRef
-Topic 250
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 1
-Subparagraph (b)(2)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147483443/250-10-50-1
Reference 12: http://www.xbrl.org/2003/role/disclosureRef
-Topic 815
-SubTopic 40
-Name Accounting Standards Codification
-Section 65
-Paragraph 1
-Subparagraph (f)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480175/815-40-65-1
Reference 13: http://www.xbrl.org/2003/role/disclosureRef
-Topic 250
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 8
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147483443/250-10-50-8
Reference 14: http://www.xbrl.org/2003/role/disclosureRef
-Topic 250
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 11
-Subparagraph (a)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147483443/250-10-50-11
Reference 15: http://www.xbrl.org/2003/role/disclosureRef
-Topic 250
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 11
-Subparagraph (b)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147483443/250-10-50-11
Reference 16: http://www.xbrl.org/2003/role/disclosureRef
-Topic 250
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 4
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147483443/250-10-50-4
Reference 17: http://www.xbrl.org/2003/role/exampleRef
-Topic 946
-SubTopic 830
-Name Accounting Standards Codification
-Section 55
-Paragraph 10
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147479168/946-830-55-10
Reference 18: http://www.xbrl.org/2003/role/disclosureRef
-Topic 946
-SubTopic 220
-Name Accounting Standards Codification
-Section 45
-Paragraph 7
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147479105/946-220-45-7
Reference 19: http://www.xbrl.org/2003/role/disclosureRef
-Topic 944
-SubTopic 220
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.7-04(18))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147477250/944-220-S99-1
Reference 20: http://www.xbrl.org/2003/role/disclosureRef
-Topic 946
-SubTopic 220
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.6-07(9))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147479134/946-220-S99-1
Reference 21: http://www.xbrl.org/2003/role/disclosureRef
-Topic 946
-SubTopic 220
-Name Accounting Standards Codification
-Section S99
-Paragraph 3
-Subparagraph (SX 210.6-09(1)(d))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147479134/946-220-S99-3
Reference 22: http://www.xbrl.org/2003/role/disclosureRef
-Topic 470
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1A
-Subparagraph (SX 210.13-01(a)(4)(i))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480097/470-10-S99-1A
Reference 23: http://www.xbrl.org/2009/role/commonPracticeRef
-Topic 470
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1A
-Subparagraph (SX 210.13-01(a)(4)(ii))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480097/470-10-S99-1A
Reference 24: http://www.xbrl.org/2003/role/disclosureRef
-Topic 470
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1A
-Subparagraph (SX 210.13-01(a)(4)(iii)(A))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480097/470-10-S99-1A
Reference 25: http://www.xbrl.org/2003/role/disclosureRef
-Topic 470
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1A
-Subparagraph (SX 210.13-01(a)(4)(iv))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480097/470-10-S99-1A
Reference 26: http://www.xbrl.org/2003/role/disclosureRef
-Topic 470
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1A
-Subparagraph (SX 210.13-01(a)(5))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480097/470-10-S99-1A
Reference 27: http://www.xbrl.org/2003/role/disclosureRef
-Topic 470
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1B
-Subparagraph (SX 210.13-02(a)(4)(i))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480097/470-10-S99-1B
Reference 28: http://www.xbrl.org/2003/role/disclosureRef
-Topic 470
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1B
-Subparagraph (SX 210.13-02(a)(4)(iii)(A))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480097/470-10-S99-1B
Reference 29: http://www.xbrl.org/2003/role/disclosureRef
-Topic 470
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1B
-Subparagraph (SX 210.13-02(a)(4)(iii)(B))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480097/470-10-S99-1B
Reference 30: http://www.xbrl.org/2003/role/disclosureRef
-Topic 470
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1B
-Subparagraph (SX 210.13-02(a)(4)(iv))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480097/470-10-S99-1B
Reference 31: http://www.xbrl.org/2003/role/disclosureRef
-Topic 470
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1B
-Subparagraph (SX 210.13-02(a)(5))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480097/470-10-S99-1B
Reference 32: http://www.xbrl.org/2003/role/disclosureRef
-Topic 260
-SubTopic 10
-Name Accounting Standards Codification
-Section 45
-Paragraph 60B
-Subparagraph (a)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482689/260-10-45-60B
Reference 33: http://www.xbrl.org/2003/role/disclosureRef
-Topic 205
-SubTopic 20
-Name Accounting Standards Codification
-Section 50
-Paragraph 7
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147483499/205-20-50-7
Reference 34: http://fasb.org/us-gaap/role/ref/legacyRef
-Topic 230
-SubTopic 10
-Name Accounting Standards Codification
-Section 45
-Paragraph 28
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482740/230-10-45-28
Reference 35: http://www.xbrl.org/2003/role/disclosureRef
-Topic 220
-SubTopic 10
-Name Accounting Standards Codification
-Section 45
-Paragraph 1A
-Subparagraph (a)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482790/220-10-45-1A
Reference 36: http://www.xbrl.org/2003/role/disclosureRef
-Topic 220
-SubTopic 10
-Name Accounting Standards Codification
-Section 45
-Paragraph 1B
-Subparagraph (a)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482790/220-10-45-1B
Reference 37: http://fasb.org/us-gaap/role/ref/legacyRef
-Topic 942
-SubTopic 220
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.9-04(22))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147478524/942-220-S99-1
| Name: |
us-gaap_NetIncomeLoss |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:monetaryItemType |
| Balance Type: |
credit |
| Period Type: |
duration |
|
| X |
- DefinitionAmount of Net Income (Loss) attributable to noncontrolling interest. Reference 1: http://www.xbrl.org/2003/role/disclosureRef
-Topic 250
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 6
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147483443/250-10-50-6
Reference 2: http://www.xbrl.org/2003/role/disclosureRef
-Topic 250
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 9
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147483443/250-10-50-9
Reference 3: http://www.xbrl.org/2003/role/disclosureRef
-Topic 250
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 8
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147483443/250-10-50-8
Reference 4: http://www.xbrl.org/2003/role/disclosureRef
-Topic 944
-SubTopic 220
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.7-04(17))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147477250/944-220-S99-1
Reference 5: http://www.xbrl.org/2009/role/commonPracticeRef
-Topic 220
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 6
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482765/220-10-50-6
Reference 6: http://fasb.org/us-gaap/role/ref/legacyRef
-Topic 810
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 1A
-Subparagraph (a)(2)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147481203/810-10-50-1A
Reference 7: http://fasb.org/us-gaap/role/ref/legacyRef
-Name Accounting Standards Codification
-Topic 810
-SubTopic 10
-Section 55
-Paragraph 4J
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147481175/810-10-55-4J
Reference 8: http://www.xbrl.org/2003/role/disclosureRef
-Topic 220
-SubTopic 10
-Name Accounting Standards Codification
-Section 45
-Paragraph 1A
-Subparagraph (a)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482790/220-10-45-1A
Reference 9: http://www.xbrl.org/2003/role/disclosureRef
-Topic 220
-SubTopic 10
-Name Accounting Standards Codification
-Section 45
-Paragraph 1B
-Subparagraph (a)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482790/220-10-45-1B
| Name: |
us-gaap_NetIncomeLossAttributableToNoncontrollingInterest |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:monetaryItemType |
| Balance Type: |
debit |
| Period Type: |
duration |
|
| X |
- DefinitionThe aggregate amount of income or expense from ancillary business-related activities (that is to say, excluding major activities considered part of the normal operations of the business). Reference 1: http://fasb.org/us-gaap/role/ref/legacyRef
-Topic 220
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 2
-Subparagraph (SX 210.5-03(7))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147483621/220-10-S99-2
| Name: |
us-gaap_NonoperatingIncomeExpense |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:monetaryItemType |
| Balance Type: |
credit |
| Period Type: |
duration |
|
| X |
- DefinitionGenerally recurring costs associated with normal operations except for the portion of these expenses which can be clearly related to production and included in cost of sales or services. Includes selling, general and administrative expense.
| Name: |
us-gaap_OperatingExpenses |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:monetaryItemType |
| Balance Type: |
debit |
| Period Type: |
duration |
|
| X |
- References
+ Details
| Name: |
us-gaap_OperatingExpensesAbstract |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:stringItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionThe net result for the period of deducting operating expenses from operating revenues. Reference 1: http://www.xbrl.org/2009/role/commonPracticeRef
-Topic 280
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 22
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482810/280-10-50-22
Reference 2: http://www.xbrl.org/2009/role/commonPracticeRef
-Topic 280
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 32
-Subparagraph (f)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482810/280-10-50-32
Reference 3: http://www.xbrl.org/2009/role/commonPracticeRef
-Topic 280
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 30
-Subparagraph (b)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482810/280-10-50-30
Reference 4: http://www.xbrl.org/2009/role/commonPracticeRef
-Topic 270
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 1
-Subparagraph (i)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482964/270-10-50-1
Reference 5: http://www.xbrl.org/2009/role/commonPracticeRef
-Topic 280
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 32
-Subparagraph (ee)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482810/280-10-50-32
Reference 6: http://fasb.org/us-gaap/role/ref/otherTransitionRef
-Topic 280
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 32
-Subparagraph (c)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482810/280-10-50-32
Reference 7: http://www.xbrl.org/2003/role/exampleRef
-Topic 280
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 31
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482810/280-10-50-31
| Name: |
us-gaap_OperatingIncomeLoss |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:monetaryItemType |
| Balance Type: |
credit |
| Period Type: |
duration |
|
| X |
- DefinitionAmount of revenue and income classified as other. Reference 1: http://www.xbrl.org/2003/role/disclosureRef
-Topic 946
-SubTopic 320
-Name Accounting Standards Codification
-Section S99
-Paragraph 6
-Subparagraph (SX 210.12-14(Column E)(2))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147477271/946-320-S99-6
Reference 2: http://www.xbrl.org/2003/role/disclosureRef
-Topic 946
-SubTopic 320
-Name Accounting Standards Codification
-Section S99
-Paragraph 6
-Subparagraph (SX 210.12-14(Column E)(Footnote 4))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147477271/946-320-S99-6
Reference 3: http://www.xbrl.org/2003/role/disclosureRef
-Topic 946
-SubTopic 320
-Name Accounting Standards Codification
-Section S99
-Paragraph 6
-Subparagraph (SX 210.12-14(Column E)(Footnote 6)(b))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147477271/946-320-S99-6
Reference 4: http://www.xbrl.org/2003/role/disclosureRef
-Topic 944
-SubTopic 220
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.7-04(4))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147477250/944-220-S99-1
Reference 5: http://www.xbrl.org/2003/role/disclosureRef
-Topic 946
-SubTopic 220
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.6-07(1)(c))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147479134/946-220-S99-1
| Name: |
us-gaap_OtherIncome |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:monetaryItemType |
| Balance Type: |
credit |
| Period Type: |
duration |
|
| X |
- DefinitionAmount of income (expense) related to nonoperating activities, classified as other. Reference 1: http://fasb.org/us-gaap/role/ref/legacyRef
-Topic 220
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 2
-Subparagraph (SX 210.5-03(9))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147483621/220-10-S99-2
| Name: |
us-gaap_OtherNonoperatingIncomeExpense |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:monetaryItemType |
| Balance Type: |
credit |
| Period Type: |
duration |
|
| X |
- References
+ Details
| Name: |
us-gaap_OtherNonoperatingIncomeExpenseAbstract |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:stringItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionAmount, after premiums ceded to other entities and premiums assumed by the entity, of premiums earned. Reference 1: http://www.xbrl.org/2003/role/disclosureRef
-Topic 944
-SubTopic 235
-Name Accounting Standards Codification
-Section S99
-Paragraph 2
-Subparagraph (SX 210.12-17(Column E))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147477965/944-235-S99-2
Reference 2: http://www.xbrl.org/2003/role/disclosureRef
-Topic 944
-SubTopic 605
-Name Accounting Standards Codification
-Section 50
-Paragraph 1
-Subparagraph (c)(3)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147479032/944-605-50-1
Reference 3: http://www.xbrl.org/2003/role/disclosureRef
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.9-04(13)(c))
-SubTopic 220
-Topic 942
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147478524/942-220-S99-1
Reference 4: http://www.xbrl.org/2003/role/disclosureRef
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.7-04(1))
-SubTopic 220
-Topic 944
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147477250/944-220-S99-1
| Name: |
us-gaap_PremiumsEarnedNet |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:monetaryItemType |
| Balance Type: |
credit |
| Period Type: |
duration |
|
| X |
- DefinitionThe consolidated profit or loss for the period, net of income taxes, including the portion attributable to the noncontrolling interest. Reference 1: http://www.xbrl.org/2003/role/disclosureRef
-Topic 250
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 6
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147483443/250-10-50-6
Reference 2: http://www.xbrl.org/2003/role/disclosureRef
-Topic 250
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 9
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147483443/250-10-50-9
Reference 3: http://www.xbrl.org/2003/role/disclosureRef
-Topic 805
-SubTopic 60
-Name Accounting Standards Codification
-Section 65
-Paragraph 1
-Subparagraph (g)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147476176/805-60-65-1
Reference 4: http://www.xbrl.org/2003/role/disclosureRef
-Topic 740
-SubTopic 323
-Name Accounting Standards Codification
-Section 65
-Paragraph 2
-Subparagraph (g)(3)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147478666/740-323-65-2
Reference 5: http://www.xbrl.org/2003/role/disclosureRef
-Topic 235
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.4-08(g)(1)(ii))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480678/235-10-S99-1
Reference 6: http://www.xbrl.org/2003/role/disclosureRef
-Topic 323
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 3
-Subparagraph (c)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147481687/323-10-50-3
Reference 7: http://www.xbrl.org/2003/role/disclosureRef
-Topic 825
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 28
-Subparagraph (f)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482907/825-10-50-28
Reference 8: http://www.xbrl.org/2003/role/disclosureRef
-Topic 250
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 1
-Subparagraph (b)(2)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147483443/250-10-50-1
Reference 9: http://www.xbrl.org/2003/role/disclosureRef
-Topic 815
-SubTopic 40
-Name Accounting Standards Codification
-Section 65
-Paragraph 1
-Subparagraph (f)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480175/815-40-65-1
Reference 10: http://www.xbrl.org/2003/role/disclosureRef
-Topic 250
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 8
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147483443/250-10-50-8
Reference 11: http://www.xbrl.org/2003/role/exampleRef
-Topic 946
-SubTopic 830
-Name Accounting Standards Codification
-Section 55
-Paragraph 11
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147479168/946-830-55-11
Reference 12: http://www.xbrl.org/2003/role/disclosureRef
-Topic 946
-SubTopic 205
-Name Accounting Standards Codification
-Section 45
-Paragraph 3
-Subparagraph (a)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147478009/946-205-45-3
Reference 13: http://www.xbrl.org/2003/role/disclosureRef
-Topic 946
-SubTopic 220
-Name Accounting Standards Codification
-Section 45
-Paragraph 7
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147479105/946-220-45-7
Reference 14: http://www.xbrl.org/2003/role/disclosureRef
-Topic 944
-SubTopic 220
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.7-04(16))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147477250/944-220-S99-1
Reference 15: http://www.xbrl.org/2003/role/disclosureRef
-Topic 946
-SubTopic 220
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.6-07(9))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147479134/946-220-S99-1
Reference 16: http://www.xbrl.org/2003/role/disclosureRef
-Topic 946
-SubTopic 220
-Name Accounting Standards Codification
-Section S99
-Paragraph 3
-Subparagraph (SX 210.6-09(1)(d))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147479134/946-220-S99-3
Reference 17: http://www.xbrl.org/2003/role/disclosureRef
-Topic 810
-SubTopic 10
-Name Accounting Standards Codification
-Section 45
-Paragraph 19
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147481231/810-10-45-19
Reference 18: http://www.xbrl.org/2009/role/commonPracticeRef
-Topic 220
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 6
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482765/220-10-50-6
Reference 19: http://www.xbrl.org/2003/role/disclosureRef
-Topic 470
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1A
-Subparagraph (SX 210.13-01(a)(4)(i))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480097/470-10-S99-1A
Reference 20: http://www.xbrl.org/2009/role/commonPracticeRef
-Topic 470
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1A
-Subparagraph (SX 210.13-01(a)(4)(ii))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480097/470-10-S99-1A
Reference 21: http://www.xbrl.org/2003/role/disclosureRef
-Topic 470
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1A
-Subparagraph (SX 210.13-01(a)(4)(iii)(A))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480097/470-10-S99-1A
Reference 22: http://www.xbrl.org/2003/role/disclosureRef
-Topic 470
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1A
-Subparagraph (SX 210.13-01(a)(4)(iv))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480097/470-10-S99-1A
Reference 23: http://www.xbrl.org/2003/role/disclosureRef
-Topic 470
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1A
-Subparagraph (SX 210.13-01(a)(5))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480097/470-10-S99-1A
Reference 24: http://www.xbrl.org/2003/role/disclosureRef
-Topic 470
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1B
-Subparagraph (SX 210.13-02(a)(4)(i))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480097/470-10-S99-1B
Reference 25: http://www.xbrl.org/2003/role/disclosureRef
-Topic 470
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1B
-Subparagraph (SX 210.13-02(a)(4)(iii)(A))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480097/470-10-S99-1B
Reference 26: http://www.xbrl.org/2003/role/disclosureRef
-Topic 470
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1B
-Subparagraph (SX 210.13-02(a)(4)(iii)(B))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480097/470-10-S99-1B
Reference 27: http://www.xbrl.org/2003/role/disclosureRef
-Topic 470
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1B
-Subparagraph (SX 210.13-02(a)(4)(iv))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480097/470-10-S99-1B
Reference 28: http://www.xbrl.org/2003/role/disclosureRef
-Topic 470
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1B
-Subparagraph (SX 210.13-02(a)(5))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480097/470-10-S99-1B
Reference 29: http://www.xbrl.org/2003/role/disclosureRef
-Topic 942
-SubTopic 235
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.9-05(b)(2))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147477314/942-235-S99-1
Reference 30: http://www.xbrl.org/2003/role/disclosureRef
-Topic 205
-SubTopic 20
-Name Accounting Standards Codification
-Section 50
-Paragraph 7
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147483499/205-20-50-7
Reference 31: http://www.xbrl.org/2003/role/exampleRef
-Topic 810
-SubTopic 10
-Name Accounting Standards Codification
-Section 55
-Paragraph 4J
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147481175/810-10-55-4J
Reference 32: http://www.xbrl.org/2003/role/exampleRef
-Topic 810
-SubTopic 10
-Name Accounting Standards Codification
-Section 55
-Paragraph 4K
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147481175/810-10-55-4K
Reference 33: http://www.xbrl.org/2003/role/disclosureRef
-Topic 220
-SubTopic 10
-Name Accounting Standards Codification
-Section 45
-Paragraph 1A
-Subparagraph (a)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482790/220-10-45-1A
Reference 34: http://www.xbrl.org/2003/role/disclosureRef
-Topic 220
-SubTopic 10
-Name Accounting Standards Codification
-Section 45
-Paragraph 1B
-Subparagraph (a)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482790/220-10-45-1B
Reference 35: http://www.xbrl.org/2003/role/disclosureRef
-Topic 230
-SubTopic 10
-Name Accounting Standards Codification
-Section 45
-Paragraph 2
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482740/230-10-45-2
Reference 36: http://www.xbrl.org/2003/role/disclosureRef
-Topic 810
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 1A
-Subparagraph (a)(1)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147481203/810-10-50-1A
Reference 37: http://www.xbrl.org/2003/role/disclosureRef
-Topic 810
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 1A
-Subparagraph (c)(1)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147481203/810-10-50-1A
| Name: |
us-gaap_ProfitLoss |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:monetaryItemType |
| Balance Type: |
credit |
| Period Type: |
duration |
|
| X |
- DefinitionAmount of revenue recognized from goods sold, services rendered, insurance premiums, or other activities that constitute an earning process. Includes, but is not limited to, investment and interest income before deduction of interest expense when recognized as a component of revenue, and sales and trading gain (loss). Reference 1: http://www.xbrl.org/2003/role/exampleRef
-Topic 280
-SubTopic 10
-Name Accounting Standards Codification
-Section 55
-Paragraph 48
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482785/280-10-55-48
Reference 2: http://www.xbrl.org/2003/role/disclosureRef
-Topic 280
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 41
-Subparagraph (a)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482810/280-10-50-41
Reference 3: http://www.xbrl.org/2003/role/disclosureRef
-Topic 270
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 1
-Subparagraph (i)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482964/270-10-50-1
Reference 4: http://www.xbrl.org/2003/role/disclosureRef
-Topic 280
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 32
-Subparagraph (ee)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482810/280-10-50-32
Reference 5: http://fasb.org/us-gaap/role/ref/otherTransitionRef
-Topic 280
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 32
-Subparagraph (b)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482810/280-10-50-32
Reference 6: http://fasb.org/us-gaap/role/ref/otherTransitionRef
-Topic 280
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 32
-Subparagraph (a)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482810/280-10-50-32
Reference 7: http://www.xbrl.org/2003/role/disclosureRef
-Topic 235
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.4-08(g)(1)(ii))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480678/235-10-S99-1
Reference 8: http://www.xbrl.org/2003/role/disclosureRef
-Topic 323
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 3
-Subparagraph (c)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147481687/323-10-50-3
Reference 9: http://www.xbrl.org/2003/role/disclosureRef
-Topic 825
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 28
-Subparagraph (f)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482907/825-10-50-28
Reference 10: http://www.xbrl.org/2003/role/disclosureRef
-Topic 470
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1A
-Subparagraph (SX 210.13-01(a)(4)(i))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480097/470-10-S99-1A
Reference 11: http://www.xbrl.org/2009/role/commonPracticeRef
-Topic 470
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1A
-Subparagraph (SX 210.13-01(a)(4)(ii))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480097/470-10-S99-1A
Reference 12: http://www.xbrl.org/2003/role/disclosureRef
-Topic 470
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1A
-Subparagraph (SX 210.13-01(a)(4)(iii)(A))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480097/470-10-S99-1A
Reference 13: http://www.xbrl.org/2003/role/disclosureRef
-Topic 470
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1A
-Subparagraph (SX 210.13-01(a)(4)(iv))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480097/470-10-S99-1A
Reference 14: http://www.xbrl.org/2003/role/disclosureRef
-Topic 470
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1A
-Subparagraph (SX 210.13-01(a)(5))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480097/470-10-S99-1A
Reference 15: http://www.xbrl.org/2003/role/disclosureRef
-Topic 470
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1B
-Subparagraph (SX 210.13-02(a)(4)(i))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480097/470-10-S99-1B
Reference 16: http://www.xbrl.org/2003/role/disclosureRef
-Topic 470
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1B
-Subparagraph (SX 210.13-02(a)(4)(iii)(A))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480097/470-10-S99-1B
Reference 17: http://www.xbrl.org/2003/role/disclosureRef
-Topic 470
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1B
-Subparagraph (SX 210.13-02(a)(4)(iii)(B))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480097/470-10-S99-1B
Reference 18: http://www.xbrl.org/2003/role/disclosureRef
-Topic 470
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1B
-Subparagraph (SX 210.13-02(a)(4)(iv))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480097/470-10-S99-1B
Reference 19: http://www.xbrl.org/2003/role/disclosureRef
-Topic 470
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1B
-Subparagraph (SX 210.13-02(a)(5))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480097/470-10-S99-1B
Reference 20: http://www.xbrl.org/2003/role/disclosureRef
-Topic 280
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 30
-Subparagraph (a)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482810/280-10-50-30
Reference 21: http://www.xbrl.org/2003/role/disclosureRef
-Topic 280
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 42
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482810/280-10-50-42
Reference 22: http://www.xbrl.org/2003/role/disclosureRef
-Topic 280
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 22
-Subparagraph (b)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482810/280-10-50-22
Reference 23: http://www.xbrl.org/2003/role/disclosureRef
-Topic 280
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 40
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482810/280-10-50-40
Reference 24: http://www.xbrl.org/2003/role/disclosureRef
-Topic 280
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 22
-Subparagraph (a)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482810/280-10-50-22
Reference 25: http://www.xbrl.org/2003/role/disclosureRef
-Topic 942
-SubTopic 235
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.9-05(b)(2))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147477314/942-235-S99-1
Reference 26: http://www.xbrl.org/2003/role/disclosureRef
-Topic 220
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 2
-Subparagraph (SX 210.5-03(1))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147483621/220-10-S99-2
| Name: |
us-gaap_Revenues |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:monetaryItemType |
| Balance Type: |
credit |
| Period Type: |
duration |
|
| X |
- References
+ Details
| Name: |
us-gaap_RevenuesAbstract |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:stringItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionThe aggregate total costs related to selling a firm's product and services, as well as all other general and administrative expenses. Direct selling expenses (for example, credit, warranty, and advertising) are expenses that can be directly linked to the sale of specific products. Indirect selling expenses are expenses that cannot be directly linked to the sale of specific products, for example telephone expenses, Internet, and postal charges. General and administrative expenses include salaries of non-sales personnel, rent, utilities, communication, etc. Reference 1: http://fasb.org/us-gaap/role/ref/legacyRef
-Topic 220
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 2
-Subparagraph (SX 210.5-03(4))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147483621/220-10-S99-2
| Name: |
us-gaap_SellingGeneralAndAdministrativeExpense |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:monetaryItemType |
| Balance Type: |
debit |
| Period Type: |
duration |
|
| X |
- DefinitionThe average number of shares or units issued and outstanding that are used in calculating diluted EPS or earnings per unit (EPU), determined based on the timing of issuance of shares or units in the period. Reference 1: http://www.xbrl.org/2003/role/disclosureRef
-Topic 260
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 1
-Subparagraph (a)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482662/260-10-50-1
Reference 2: http://www.xbrl.org/2003/role/disclosureRef
-Topic 260
-SubTopic 10
-Name Accounting Standards Codification
-Section 45
-Paragraph 16
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482689/260-10-45-16
| Name: |
us-gaap_WeightedAverageNumberOfDilutedSharesOutstanding |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:sharesItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionNumber of [basic] shares or units, after adjustment for contingently issuable shares or units and other shares or units not deemed outstanding, determined by relating the portion of time within a reporting period that common shares or units have been outstanding to the total time in that period. Reference 1: http://www.xbrl.org/2003/role/disclosureRef
-Topic 260
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 1
-Subparagraph (a)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482662/260-10-50-1
Reference 2: http://www.xbrl.org/2003/role/disclosureRef
-Topic 260
-SubTopic 10
-Name Accounting Standards Codification
-Section 45
-Paragraph 10
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482689/260-10-45-10
| Name: |
us-gaap_WeightedAverageNumberOfSharesOutstandingBasic |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:sharesItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
v3.24.2.u1
Condensed Consolidated Statements of Stockholders' Equity - USD ($)
$ in Thousands |
Total |
Common Stock |
Additional Paid-In Capital |
Accumulated Deficit |
Noncontrolling Interest |
| Beginning Balance (in shares) at Dec. 31, 2022 |
|
187,280,015
|
|
|
|
| Beginning Balance at Dec. 31, 2022 |
$ 239,302
|
$ 187
|
$ 970,180
|
$ (732,241)
|
$ 1,176
|
| Increase (Decrease) in Stockholders' Equity [Roll Forward] |
|
|
|
|
|
| Net loss |
(65,865)
|
|
|
(65,761)
|
(104)
|
| Issuance of common stock upon vesting of restricted stock units (in shares) |
|
1,247,972
|
|
|
|
| Issuance of common stock upon vesting of restricted stock units |
1
|
$ 1
|
|
|
|
| Forfeitures (in shares) |
|
(15,222)
|
|
|
|
| Equity-based compensation |
37,614
|
|
37,614
|
|
|
| Repurchase of noncontrolling interest attributable to subsidiary |
60
|
|
|
|
60
|
| Ending Balance (in shares) at Jun. 30, 2023 |
|
188,512,765
|
|
|
|
| Ending Balance at Jun. 30, 2023 |
211,112
|
$ 188
|
1,007,794
|
(798,002)
|
1,132
|
| Beginning Balance (in shares) at Mar. 31, 2023 |
|
188,475,278
|
|
|
|
| Beginning Balance at Mar. 31, 2023 |
223,940
|
$ 188
|
992,158
|
(769,525)
|
1,119
|
| Increase (Decrease) in Stockholders' Equity [Roll Forward] |
|
|
|
|
|
| Net loss |
(28,494)
|
$ 0
|
0
|
(28,477)
|
(17)
|
| Issuance of common stock upon vesting of restricted stock units (in shares) |
|
43,195
|
|
|
|
| Forfeitures (in shares) |
|
(5,708)
|
|
|
|
| Equity-based compensation |
15,636
|
|
15,636
|
|
|
| Noncontrolling interest attributable to subsidiary |
30
|
|
|
|
30
|
| Ending Balance (in shares) at Jun. 30, 2023 |
|
188,512,765
|
|
|
|
| Ending Balance at Jun. 30, 2023 |
$ 211,112
|
$ 188
|
1,007,794
|
(798,002)
|
1,132
|
| Beginning Balance (in shares) at Dec. 31, 2023 |
188,951,643
|
188,951,643
|
|
|
|
| Beginning Balance at Dec. 31, 2023 |
$ 158,071
|
$ 189
|
1,037,015
|
(880,258)
|
1,125
|
| Increase (Decrease) in Stockholders' Equity [Roll Forward] |
|
|
|
|
|
| Net loss |
(70,578)
|
|
|
(70,531)
|
(47)
|
| Issuance of common stock upon vesting of restricted stock units (in shares) |
|
2,357,723
|
|
|
|
| Issuance of common stock upon vesting of restricted stock units |
2
|
$ 2
|
|
|
|
| Forfeitures (in shares) |
|
(2,799)
|
|
|
|
| Shares withheld related to net restricted stock settlement (in shares) |
|
(69,820)
|
|
|
|
| Shares withheld related to net restricted stock settlement |
(350)
|
|
(350)
|
|
|
| Equity-based compensation |
37,638
|
|
37,638
|
|
|
| Noncontrolling interest attributable to subsidiary |
$ 15
|
|
|
|
15
|
| Ending Balance (in shares) at Jun. 30, 2024 |
191,236,747
|
191,236,747
|
|
|
|
| Ending Balance at Jun. 30, 2024 |
$ 124,798
|
$ 191
|
1,074,303
|
(950,789)
|
1,093
|
| Beginning Balance (in shares) at Mar. 31, 2024 |
|
191,156,569
|
|
|
|
| Beginning Balance at Mar. 31, 2024 |
132,017
|
$ 191
|
1,057,519
|
(926,779)
|
1,086
|
| Increase (Decrease) in Stockholders' Equity [Roll Forward] |
|
|
|
|
|
| Net loss |
(24,003)
|
|
|
(24,010)
|
7
|
| Issuance of common stock upon vesting of restricted stock units (in shares) |
|
80,178
|
|
|
|
| Equity-based compensation |
$ 16,784
|
|
16,784
|
|
|
| Ending Balance (in shares) at Jun. 30, 2024 |
191,236,747
|
191,236,747
|
|
|
|
| Ending Balance at Jun. 30, 2024 |
$ 124,798
|
$ 191
|
$ 1,074,303
|
$ (950,789)
|
$ 1,093
|
| X |
- DefinitionAmount of increase to additional paid-in capital (APIC) for recognition of cost for award under share-based payment arrangement. Reference 1: http://www.xbrl.org/2003/role/disclosureRef
-Topic 718
-SubTopic 10
-Name Accounting Standards Codification
-Section 35
-Paragraph 2
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480483/718-10-35-2
Reference 2: http://fasb.org/us-gaap/role/ref/legacyRef
-Name Accounting Standards Codification
-Topic 718
-SubTopic 20
-Section 55
-Paragraph 13
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147481089/718-20-55-13
Reference 3: http://fasb.org/us-gaap/role/ref/legacyRef
-Name Accounting Standards Codification
-Topic 718
-SubTopic 20
-Section 55
-Paragraph 12
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147481089/718-20-55-12
| Name: |
us-gaap_AdjustmentsToAdditionalPaidInCapitalSharebasedCompensationRequisiteServicePeriodRecognitionValue |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:monetaryItemType |
| Balance Type: |
credit |
| Period Type: |
duration |
|
| X |
- DefinitionNumber of shares of common stock outstanding. Common stock represent the ownership interest in a corporation. Reference 1: http://fasb.org/us-gaap/role/ref/legacyRef
-Name Accounting Standards Codification
-Section 50
-Paragraph 2
-SubTopic 10
-Topic 505
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147481112/505-10-50-2
Reference 2: http://fasb.org/us-gaap/role/ref/legacyRef
-Topic 210
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.5-02(29))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480566/210-10-S99-1
Reference 3: http://www.xbrl.org/2003/role/disclosureRef
-Topic 946
-SubTopic 210
-Name Accounting Standards Codification
-Section S99
-Paragraph 2
-Subparagraph (SX 210.6-05(4))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147479170/946-210-S99-2
Reference 4: http://www.xbrl.org/2009/role/commonPracticeRef
-Topic 946
-SubTopic 220
-Name Accounting Standards Codification
-Section S99
-Paragraph 3
-Subparagraph (SX 210.6-09(4)(b))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147479134/946-220-S99-3
Reference 5: http://www.xbrl.org/2003/role/disclosureRef
-Topic 946
-SubTopic 210
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.6-04(16)(a))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147479170/946-210-S99-1
Reference 6: http://www.xbrl.org/2009/role/commonPracticeRef
-Topic 946
-SubTopic 220
-Name Accounting Standards Codification
-Section S99
-Paragraph 3
-Subparagraph (SX 210.6-09(7))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147479134/946-220-S99-3
| Name: |
us-gaap_CommonStockSharesOutstanding |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:sharesItemType |
| Balance Type: |
na |
| Period Type: |
instant |
|
| X |
- DefinitionA roll forward is a reconciliation of a concept from the beginning of a period to the end of a period.
| Name: |
us-gaap_IncreaseDecreaseInStockholdersEquityRollForward |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:stringItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionDecrease in noncontrolling interest (for example, but not limited to, redeeming or purchasing the interests of noncontrolling shareholders, issuance of shares (interests) by the non-wholly owned subsidiary to the parent entity for other than cash, and a buyback of shares (interest) by the non-wholly owned subsidiary from the noncontrolling interests). Reference 1: http://fasb.org/us-gaap/role/ref/legacyRef
-Topic 505
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.3-04)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480008/505-10-S99-1
Reference 2: http://fasb.org/us-gaap/role/ref/legacyRef
-Topic 810
-SubTopic 10
-Name Accounting Standards Codification
-Section 45
-Paragraph 23
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147481231/810-10-45-23
Reference 3: http://fasb.org/us-gaap/role/ref/legacyRef
-Name Accounting Standards Codification
-Topic 810
-SubTopic 10
-Section 45
-Paragraph 24
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147481231/810-10-45-24
| Name: |
us-gaap_MinorityInterestDecreaseFromRedemptions |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:monetaryItemType |
| Balance Type: |
debit |
| Period Type: |
duration |
|
| X |
- DefinitionAmount of increase in noncontrolling interest from subsidiary issuance of equity interests to noncontrolling interest holders. Reference 1: http://fasb.org/us-gaap/role/ref/legacyRef
-Topic 810
-SubTopic 10
-Name Accounting Standards Codification
-Section 45
-Paragraph 23
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147481231/810-10-45-23
Reference 2: http://fasb.org/us-gaap/role/ref/legacyRef
-Name Accounting Standards Codification
-Topic 505
-SubTopic 10
-Section S99
-Paragraph 1
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480008/505-10-S99-1
Reference 3: http://fasb.org/us-gaap/role/ref/legacyRef
-Name Accounting Standards Codification
-Section 50
-Paragraph 1A
-Subparagraph (c)(2)
-SubTopic 10
-Topic 810
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147481203/810-10-50-1A
| Name: |
us-gaap_NoncontrollingInterestIncreaseFromSubsidiaryEquityIssuance |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:monetaryItemType |
| Balance Type: |
credit |
| Period Type: |
duration |
|
| X |
- DefinitionThe consolidated profit or loss for the period, net of income taxes, including the portion attributable to the noncontrolling interest. Reference 1: http://www.xbrl.org/2003/role/disclosureRef
-Topic 250
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 6
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147483443/250-10-50-6
Reference 2: http://www.xbrl.org/2003/role/disclosureRef
-Topic 250
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 9
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147483443/250-10-50-9
Reference 3: http://www.xbrl.org/2003/role/disclosureRef
-Topic 805
-SubTopic 60
-Name Accounting Standards Codification
-Section 65
-Paragraph 1
-Subparagraph (g)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147476176/805-60-65-1
Reference 4: http://www.xbrl.org/2003/role/disclosureRef
-Topic 740
-SubTopic 323
-Name Accounting Standards Codification
-Section 65
-Paragraph 2
-Subparagraph (g)(3)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147478666/740-323-65-2
Reference 5: http://www.xbrl.org/2003/role/disclosureRef
-Topic 235
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.4-08(g)(1)(ii))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480678/235-10-S99-1
Reference 6: http://www.xbrl.org/2003/role/disclosureRef
-Topic 323
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 3
-Subparagraph (c)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147481687/323-10-50-3
Reference 7: http://www.xbrl.org/2003/role/disclosureRef
-Topic 825
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 28
-Subparagraph (f)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482907/825-10-50-28
Reference 8: http://www.xbrl.org/2003/role/disclosureRef
-Topic 250
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 1
-Subparagraph (b)(2)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147483443/250-10-50-1
Reference 9: http://www.xbrl.org/2003/role/disclosureRef
-Topic 815
-SubTopic 40
-Name Accounting Standards Codification
-Section 65
-Paragraph 1
-Subparagraph (f)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480175/815-40-65-1
Reference 10: http://www.xbrl.org/2003/role/disclosureRef
-Topic 250
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 8
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147483443/250-10-50-8
Reference 11: http://www.xbrl.org/2003/role/exampleRef
-Topic 946
-SubTopic 830
-Name Accounting Standards Codification
-Section 55
-Paragraph 11
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147479168/946-830-55-11
Reference 12: http://www.xbrl.org/2003/role/disclosureRef
-Topic 946
-SubTopic 205
-Name Accounting Standards Codification
-Section 45
-Paragraph 3
-Subparagraph (a)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147478009/946-205-45-3
Reference 13: http://www.xbrl.org/2003/role/disclosureRef
-Topic 946
-SubTopic 220
-Name Accounting Standards Codification
-Section 45
-Paragraph 7
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147479105/946-220-45-7
Reference 14: http://www.xbrl.org/2003/role/disclosureRef
-Topic 944
-SubTopic 220
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.7-04(16))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147477250/944-220-S99-1
Reference 15: http://www.xbrl.org/2003/role/disclosureRef
-Topic 946
-SubTopic 220
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.6-07(9))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147479134/946-220-S99-1
Reference 16: http://www.xbrl.org/2003/role/disclosureRef
-Topic 946
-SubTopic 220
-Name Accounting Standards Codification
-Section S99
-Paragraph 3
-Subparagraph (SX 210.6-09(1)(d))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147479134/946-220-S99-3
Reference 17: http://www.xbrl.org/2003/role/disclosureRef
-Topic 810
-SubTopic 10
-Name Accounting Standards Codification
-Section 45
-Paragraph 19
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147481231/810-10-45-19
Reference 18: http://www.xbrl.org/2009/role/commonPracticeRef
-Topic 220
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 6
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482765/220-10-50-6
Reference 19: http://www.xbrl.org/2003/role/disclosureRef
-Topic 470
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1A
-Subparagraph (SX 210.13-01(a)(4)(i))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480097/470-10-S99-1A
Reference 20: http://www.xbrl.org/2009/role/commonPracticeRef
-Topic 470
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1A
-Subparagraph (SX 210.13-01(a)(4)(ii))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480097/470-10-S99-1A
Reference 21: http://www.xbrl.org/2003/role/disclosureRef
-Topic 470
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1A
-Subparagraph (SX 210.13-01(a)(4)(iii)(A))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480097/470-10-S99-1A
Reference 22: http://www.xbrl.org/2003/role/disclosureRef
-Topic 470
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1A
-Subparagraph (SX 210.13-01(a)(4)(iv))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480097/470-10-S99-1A
Reference 23: http://www.xbrl.org/2003/role/disclosureRef
-Topic 470
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1A
-Subparagraph (SX 210.13-01(a)(5))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480097/470-10-S99-1A
Reference 24: http://www.xbrl.org/2003/role/disclosureRef
-Topic 470
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1B
-Subparagraph (SX 210.13-02(a)(4)(i))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480097/470-10-S99-1B
Reference 25: http://www.xbrl.org/2003/role/disclosureRef
-Topic 470
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1B
-Subparagraph (SX 210.13-02(a)(4)(iii)(A))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480097/470-10-S99-1B
Reference 26: http://www.xbrl.org/2003/role/disclosureRef
-Topic 470
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1B
-Subparagraph (SX 210.13-02(a)(4)(iii)(B))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480097/470-10-S99-1B
Reference 27: http://www.xbrl.org/2003/role/disclosureRef
-Topic 470
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1B
-Subparagraph (SX 210.13-02(a)(4)(iv))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480097/470-10-S99-1B
Reference 28: http://www.xbrl.org/2003/role/disclosureRef
-Topic 470
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1B
-Subparagraph (SX 210.13-02(a)(5))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480097/470-10-S99-1B
Reference 29: http://www.xbrl.org/2003/role/disclosureRef
-Topic 942
-SubTopic 235
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.9-05(b)(2))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147477314/942-235-S99-1
Reference 30: http://www.xbrl.org/2003/role/disclosureRef
-Topic 205
-SubTopic 20
-Name Accounting Standards Codification
-Section 50
-Paragraph 7
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147483499/205-20-50-7
Reference 31: http://www.xbrl.org/2003/role/exampleRef
-Topic 810
-SubTopic 10
-Name Accounting Standards Codification
-Section 55
-Paragraph 4J
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147481175/810-10-55-4J
Reference 32: http://www.xbrl.org/2003/role/exampleRef
-Topic 810
-SubTopic 10
-Name Accounting Standards Codification
-Section 55
-Paragraph 4K
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147481175/810-10-55-4K
Reference 33: http://www.xbrl.org/2003/role/disclosureRef
-Topic 220
-SubTopic 10
-Name Accounting Standards Codification
-Section 45
-Paragraph 1A
-Subparagraph (a)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482790/220-10-45-1A
Reference 34: http://www.xbrl.org/2003/role/disclosureRef
-Topic 220
-SubTopic 10
-Name Accounting Standards Codification
-Section 45
-Paragraph 1B
-Subparagraph (a)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482790/220-10-45-1B
Reference 35: http://www.xbrl.org/2003/role/disclosureRef
-Topic 230
-SubTopic 10
-Name Accounting Standards Codification
-Section 45
-Paragraph 2
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482740/230-10-45-2
Reference 36: http://www.xbrl.org/2003/role/disclosureRef
-Topic 810
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 1A
-Subparagraph (a)(1)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147481203/810-10-50-1A
Reference 37: http://www.xbrl.org/2003/role/disclosureRef
-Topic 810
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 1A
-Subparagraph (c)(1)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147481203/810-10-50-1A
| Name: |
us-gaap_ProfitLoss |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:monetaryItemType |
| Balance Type: |
credit |
| Period Type: |
duration |
|
| X |
- DefinitionNumber of shares used to settle grantee's tax withholding obligation for award under share-based payment arrangement.
| Name: |
us-gaap_SharesPaidForTaxWithholdingForShareBasedCompensation |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:sharesItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionNumber of shares issued during the period related to Restricted Stock Awards, net of any shares forfeited. Reference 1: http://fasb.org/us-gaap/role/ref/legacyRef
-Name Accounting Standards Codification
-Section 50
-Paragraph 2
-SubTopic 10
-Topic 505
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147481112/505-10-50-2
Reference 2: http://fasb.org/us-gaap/role/ref/legacyRef
-Topic 210
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.5-02(28))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480566/210-10-S99-1
Reference 3: http://fasb.org/us-gaap/role/ref/legacyRef
-Topic 210
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.5-02(29))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480566/210-10-S99-1
Reference 4: http://fasb.org/us-gaap/role/ref/legacyRef
-Topic 505
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.3-04)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480008/505-10-S99-1
| Name: |
us-gaap_StockIssuedDuringPeriodSharesRestrictedStockAwardNetOfForfeitures |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:sharesItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionNumber of shares (or other type of equity) forfeited during the period.
| Name: |
us-gaap_StockIssuedDuringPeriodSharesShareBasedCompensationForfeited |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:sharesItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionValue of stock related to Restricted Stock Awards issued during the period, net of the stock value of such awards forfeited. Reference 1: http://fasb.org/us-gaap/role/ref/legacyRef
-Name Accounting Standards Codification
-Section 50
-Paragraph 2
-SubTopic 10
-Topic 505
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147481112/505-10-50-2
Reference 2: http://fasb.org/us-gaap/role/ref/legacyRef
-Topic 505
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.3-04)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480008/505-10-S99-1
| Name: |
us-gaap_StockIssuedDuringPeriodValueRestrictedStockAwardNetOfForfeitures |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:monetaryItemType |
| Balance Type: |
credit |
| Period Type: |
duration |
|
| X |
- DefinitionAmount of equity (deficit) attributable to parent and noncontrolling interest. Excludes temporary equity. Reference 1: http://www.xbrl.org/2003/role/disclosureRef
-Topic 250
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 6
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147483443/250-10-50-6
Reference 2: http://www.xbrl.org/2003/role/disclosureRef
-Topic 805
-SubTopic 60
-Name Accounting Standards Codification
-Section 65
-Paragraph 1
-Subparagraph (g)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147476176/805-60-65-1
Reference 3: http://www.xbrl.org/2003/role/disclosureRef
-Topic 805
-SubTopic 60
-Name Accounting Standards Codification
-Section 65
-Paragraph 1
-Subparagraph (d)(1)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147476176/805-60-65-1
Reference 4: http://www.xbrl.org/2003/role/disclosureRef
-Topic 740
-SubTopic 323
-Name Accounting Standards Codification
-Section 65
-Paragraph 2
-Subparagraph (e)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147478666/740-323-65-2
Reference 5: http://www.xbrl.org/2003/role/disclosureRef
-Topic 740
-SubTopic 323
-Name Accounting Standards Codification
-Section 65
-Paragraph 2
-Subparagraph (g)(4)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147478666/740-323-65-2
Reference 6: http://www.xbrl.org/2003/role/disclosureRef
-Topic 740
-SubTopic 323
-Name Accounting Standards Codification
-Section 65
-Paragraph 2
-Subparagraph (d)(2)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147478666/740-323-65-2
Reference 7: http://www.xbrl.org/2003/role/disclosureRef
-Topic 740
-SubTopic 323
-Name Accounting Standards Codification
-Section 65
-Paragraph 2
-Subparagraph (d)(1)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147478666/740-323-65-2
Reference 8: http://www.xbrl.org/2003/role/disclosureRef
-Topic 848
-SubTopic 10
-Name Accounting Standards Codification
-Section 65
-Paragraph 2
-Subparagraph (a)(3)(iii)(03)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147483550/848-10-65-2
Reference 9: http://www.xbrl.org/2003/role/disclosureRef
-Topic 842
-SubTopic 10
-Name Accounting Standards Codification
-Section 65
-Paragraph 8
-Subparagraph (c)(3)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147479832/842-10-65-8
Reference 10: http://www.xbrl.org/2003/role/disclosureRef
-Topic 250
-SubTopic 10
-Name Accounting Standards Codification
-Section 45
-Paragraph 24
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147483421/250-10-45-24
Reference 11: http://www.xbrl.org/2003/role/disclosureRef
-Topic 250
-SubTopic 10
-Name Accounting Standards Codification
-Section 45
-Paragraph 23
-Subparagraph (b)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147483421/250-10-45-23
Reference 12: http://www.xbrl.org/2003/role/disclosureRef
-Topic 250
-SubTopic 10
-Name Accounting Standards Codification
-Section 45
-Paragraph 5
-Subparagraph (b)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147483421/250-10-45-5
Reference 13: http://www.xbrl.org/2003/role/disclosureRef
-Topic 326
-SubTopic 10
-Name Accounting Standards Codification
-Section 65
-Paragraph 5
-Subparagraph (c)(2)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147479654/326-10-65-5
Reference 14: http://www.xbrl.org/2003/role/disclosureRef
-Topic 815
-SubTopic 20
-Name Accounting Standards Codification
-Section 65
-Paragraph 6
-Subparagraph (e)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480528/815-20-65-6
Reference 15: http://www.xbrl.org/2003/role/disclosureRef
-Topic 815
-SubTopic 20
-Name Accounting Standards Codification
-Section 65
-Paragraph 6
-Subparagraph (h)(1)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480528/815-20-65-6
Reference 16: http://www.xbrl.org/2003/role/disclosureRef
-Topic 815
-SubTopic 20
-Name Accounting Standards Codification
-Section 65
-Paragraph 6
-Subparagraph (h)(1)(i)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480528/815-20-65-6
Reference 17: http://www.xbrl.org/2003/role/disclosureRef
-Topic 815
-SubTopic 20
-Name Accounting Standards Codification
-Section 65
-Paragraph 6
-Subparagraph (h)(1)(iii)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480528/815-20-65-6
Reference 18: http://www.xbrl.org/2003/role/disclosureRef
-Topic 815
-SubTopic 20
-Name Accounting Standards Codification
-Section 65
-Paragraph 6
-Subparagraph (h)(1)(iv)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480528/815-20-65-6
Reference 19: http://www.xbrl.org/2003/role/disclosureRef
-Topic 815
-SubTopic 20
-Name Accounting Standards Codification
-Section 65
-Paragraph 6
-Subparagraph (i)(3)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480528/815-20-65-6
Reference 20: http://www.xbrl.org/2003/role/disclosureRef
-Topic 105
-SubTopic 10
-Name Accounting Standards Codification
-Section 65
-Paragraph 6
-Subparagraph (c)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147479343/105-10-65-6
Reference 21: http://www.xbrl.org/2003/role/disclosureRef
-Topic 105
-SubTopic 10
-Name Accounting Standards Codification
-Section 65
-Paragraph 6
-Subparagraph (d)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147479343/105-10-65-6
Reference 22: http://www.xbrl.org/2003/role/disclosureRef
-Topic 944
-SubTopic 40
-Name Accounting Standards Codification
-Section 65
-Paragraph 2
-Subparagraph (f)(1)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480016/944-40-65-2
Reference 23: http://www.xbrl.org/2003/role/disclosureRef
-Topic 944
-SubTopic 40
-Name Accounting Standards Codification
-Section 65
-Paragraph 2
-Subparagraph (f)(2)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480016/944-40-65-2
Reference 24: http://www.xbrl.org/2003/role/disclosureRef
-Topic 740
-SubTopic 10
-Name Accounting Standards Codification
-Section 65
-Paragraph 8
-Subparagraph (d)(2)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482615/740-10-65-8
Reference 25: http://www.xbrl.org/2003/role/disclosureRef
-Topic 740
-SubTopic 10
-Name Accounting Standards Codification
-Section 65
-Paragraph 8
-Subparagraph (d)(3)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482615/740-10-65-8
Reference 26: http://www.xbrl.org/2003/role/disclosureRef
-Topic 326
-SubTopic 10
-Name Accounting Standards Codification
-Section 65
-Paragraph 4
-Subparagraph (d)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147479654/326-10-65-4
Reference 27: http://www.xbrl.org/2003/role/disclosureRef
-Topic 250
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 1
-Subparagraph (b)(3)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147483443/250-10-50-1
Reference 28: http://www.xbrl.org/2003/role/disclosureRef
-Topic 815
-SubTopic 40
-Name Accounting Standards Codification
-Section 65
-Paragraph 1
-Subparagraph (e)(3)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480175/815-40-65-1
Reference 29: http://www.xbrl.org/2003/role/disclosureRef
-Topic 250
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 7
-Subparagraph (b)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147483443/250-10-50-7
Reference 30: http://www.xbrl.org/2003/role/disclosureRef
-Topic 220
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 5
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482765/220-10-50-5
Reference 31: http://www.xbrl.org/2003/role/disclosureRef
-Topic 830
-SubTopic 30
-Name Accounting Standards Codification
-Section 50
-Paragraph 1
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147481674/830-30-50-1
Reference 32: http://www.xbrl.org/2003/role/disclosureRef
-Topic 830
-SubTopic 30
-Name Accounting Standards Codification
-Section 45
-Paragraph 17
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147481694/830-30-45-17
Reference 33: http://www.xbrl.org/2003/role/disclosureRef
-Topic 830
-SubTopic 30
-Name Accounting Standards Codification
-Section 45
-Paragraph 20
-Subparagraph (a)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147481694/830-30-45-20
Reference 34: http://www.xbrl.org/2003/role/exampleRef
-Topic 946
-SubTopic 830
-Name Accounting Standards Codification
-Section 55
-Paragraph 11
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147479168/946-830-55-11
Reference 35: http://www.xbrl.org/2003/role/disclosureRef
-Topic 946
-SubTopic 205
-Name Accounting Standards Codification
-Section 45
-Paragraph 3
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147478009/946-205-45-3
Reference 36: http://www.xbrl.org/2003/role/disclosureRef
-Topic 946
-SubTopic 505
-Name Accounting Standards Codification
-Section 50
-Paragraph 3
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147478448/946-505-50-3
Reference 37: http://www.xbrl.org/2003/role/disclosureRef
-Topic 946
-SubTopic 210
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.6-04(19))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147479170/946-210-S99-1
Reference 38: http://www.xbrl.org/2003/role/disclosureRef
-Topic 946
-SubTopic 210
-Name Accounting Standards Codification
-Section S99
-Paragraph 2
-Subparagraph (SX 210.6-05(4))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147479170/946-210-S99-2
Reference 39: http://www.xbrl.org/2009/role/commonPracticeRef
-Topic 946
-SubTopic 220
-Name Accounting Standards Codification
-Section S99
-Paragraph 3
-Subparagraph (SX 210.6-09(4)(b))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147479134/946-220-S99-3
Reference 40: http://www.xbrl.org/2003/role/disclosureRef
-Topic 946
-SubTopic 220
-Name Accounting Standards Codification
-Section S99
-Paragraph 3
-Subparagraph (SX 210.6-09(6))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147479134/946-220-S99-3
Reference 41: http://www.xbrl.org/2003/role/disclosureRef
-Topic 946
-SubTopic 220
-Name Accounting Standards Codification
-Section S99
-Paragraph 3
-Subparagraph (SX 210.6-09(7))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147479134/946-220-S99-3
Reference 42: http://www.xbrl.org/2003/role/disclosureRef
-Topic 505
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.3-04)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480008/505-10-S99-1
Reference 43: http://www.xbrl.org/2009/role/commonPracticeRef
-Topic 235
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.4-08(g)(1)(ii))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480678/235-10-S99-1
Reference 44: http://www.xbrl.org/2009/role/commonPracticeRef
-Topic 323
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 3
-Subparagraph (c)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147481687/323-10-50-3
Reference 45: http://www.xbrl.org/2009/role/commonPracticeRef
-Topic 825
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 28
-Subparagraph (f)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482907/825-10-50-28
Reference 46: http://fasb.org/us-gaap/role/ref/legacyRef
-Name Accounting Standards Codification
-Topic 810
-SubTopic 10
-Section 45
-Paragraph 15
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147481231/810-10-45-15
Reference 47: http://fasb.org/us-gaap/role/ref/legacyRef
-Name Accounting Standards Codification
-Topic 810
-SubTopic 10
-Section 45
-Paragraph 16
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147481231/810-10-45-16
Reference 48: http://fasb.org/us-gaap/role/ref/legacyRef
-Name Accounting Standards Codification
-Topic 810
-SubTopic 10
-Section 55
-Paragraph 4I
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147481175/810-10-55-4I
Reference 49: http://www.xbrl.org/2003/role/disclosureRef
-Topic 350
-SubTopic 60
-Name Accounting Standards Codification
-Section 65
-Paragraph 1
-Subparagraph (b)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147476166/350-60-65-1
| Name: |
us-gaap_StockholdersEquityIncludingPortionAttributableToNoncontrollingInterest |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:monetaryItemType |
| Balance Type: |
credit |
| Period Type: |
instant |
|
v3.24.2.u1
Condensed Consolidated Statements of Cash Flows - USD ($)
$ in Thousands |
6 Months Ended |
Jun. 30, 2024 |
Jun. 30, 2023 |
| Operating Activities: |
|
|
| Net loss |
$ (70,578)
|
$ (65,865)
|
| Adjustments to reconcile net loss to net cash provided by operating activities: |
|
|
| Provision for credit loss |
95
|
51
|
| Loss (gain) on right of use assets |
143
|
(289)
|
| Depreciation and amortization |
12,568
|
10,246
|
| Amortization-investment discount |
(1,762)
|
(1,716)
|
| Amortization-debt issuance costs |
612
|
734
|
| Equity-based compensation |
37,638
|
37,614
|
| Non-cash lease expense |
930
|
1,348
|
| Changes in operating assets and liabilities: |
|
|
| Accounts receivable |
(63,560)
|
3,914
|
| Prepaid expenses and other current assets |
(7,221)
|
(35,077)
|
| Other assets |
92
|
(112)
|
| Medical expenses payable |
109,970
|
37,063
|
| Accounts payable and accrued expenses |
1,373
|
(8,996)
|
| Deferred premium revenue |
(310)
|
147,169
|
| Accrued compensation |
(1,278)
|
(1,632)
|
| Lease liabilities |
(1,421)
|
(2,165)
|
| Net cash provided by operating activities |
17,291
|
122,287
|
| Investing Activities: |
|
|
| Purchase of investments |
(40,000)
|
(156,943)
|
| Maturities of investments |
132,525
|
36,150
|
| Acquisition of property and equipment |
(22,854)
|
(15,845)
|
| Net cash provided by (used in) investing activities |
69,671
|
(136,638)
|
| Financing Activities: |
|
|
| Proceeds from long-term debt |
50,000
|
0
|
| Debt issuance costs |
(512)
|
0
|
| Payment of employment taxes related to release of restricted stock |
(350)
|
0
|
| Contributions from noncontrolling interest holders |
15
|
60
|
| Net cash provided by financing activities |
49,153
|
60
|
| Net increase (decrease) in cash |
136,115
|
(14,291)
|
| Cash, cash equivalents and restricted cash at beginning of period |
204,954
|
411,299
|
| Cash, cash equivalents and restricted cash at end of period |
341,069
|
397,008
|
| Supplemental disclosure of cash flow information: |
|
|
| Cash paid for interest |
10,247
|
8,986
|
| Supplemental non-cash investing and financing activities: |
|
|
| Acquisition of property in accounts payable |
122
|
42
|
| Reconciliation of cash, cash equivalents and restricted cash as shown in the statement of cash flows: |
|
|
| Cash and cash equivalents |
339,007
|
395,258
|
| Restricted cash in other assets |
2,062
|
1,750
|
| Total |
$ 341,069
|
$ 397,008
|
| X |
- Definition
+ References
+ Details
| Name: |
alhc_GainLossOnOperatingLeaseRightOfUseAsset |
| Namespace Prefix: |
alhc_ |
| Data Type: |
xbrli:monetaryItemType |
| Balance Type: |
credit |
| Period Type: |
duration |
|
| X |
- DefinitionIncrease decrease in accrued compensation.
| Name: |
alhc_IncreaseDecreaseInAccruedCompensation |
| Namespace Prefix: |
alhc_ |
| Data Type: |
xbrli:monetaryItemType |
| Balance Type: |
debit |
| Period Type: |
duration |
|
| X |
- DefinitionIncrease decrease in medical expenses payable.
| Name: |
alhc_IncreaseDecreaseInMedicalExpensesPayable |
| Namespace Prefix: |
alhc_ |
| Data Type: |
xbrli:monetaryItemType |
| Balance Type: |
debit |
| Period Type: |
duration |
|
| X |
- References
+ Details
| Name: |
us-gaap_AdjustmentsToReconcileNetIncomeLossToCashProvidedByUsedInOperatingActivitiesAbstract |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:stringItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionAmount of amortization expense attributable to debt issuance costs. Reference 1: http://fasb.org/us-gaap/role/ref/legacyRef
-Topic 220
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 2
-Subparagraph (SX 210.5-03(8))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147483621/220-10-S99-2
Reference 2: http://www.xbrl.org/2003/role/disclosureRef
-Topic 470
-SubTopic 20
-Name Accounting Standards Codification
-Section 50
-Paragraph 1F
-Subparagraph (b)(2)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147481139/470-20-50-1F
Reference 3: http://www.xbrl.org/2009/role/commonPracticeRef
-Topic 230
-SubTopic 10
-Name Accounting Standards Codification
-Section 45
-Paragraph 28
-Subparagraph (b)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482740/230-10-45-28
Reference 4: http://www.xbrl.org/2009/role/commonPracticeRef
-Topic 835
-SubTopic 30
-Name Accounting Standards Codification
-Section 45
-Paragraph 3
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482925/835-30-45-3
| Name: |
us-gaap_AmortizationOfFinancingCosts |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:monetaryItemType |
| Balance Type: |
debit |
| Period Type: |
duration |
|
| X |
- DefinitionFuture cash outflow to pay for purchases of fixed assets that have occurred. Reference 1: http://fasb.org/us-gaap/role/ref/legacyRef
-Name Accounting Standards Codification
-Topic 230
-SubTopic 10
-Section 50
-Paragraph 4
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482913/230-10-50-4
Reference 2: http://fasb.org/us-gaap/role/ref/legacyRef
-Name Accounting Standards Codification
-Topic 230
-SubTopic 10
-Section 50
-Paragraph 3
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482913/230-10-50-3
Reference 3: http://fasb.org/us-gaap/role/ref/legacyRef
-Name Accounting Standards Codification
-Topic 230
-SubTopic 10
-Section 50
-Paragraph 5
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482913/230-10-50-5
| Name: |
us-gaap_CapitalExpendituresIncurredButNotYetPaid |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:monetaryItemType |
| Balance Type: |
credit |
| Period Type: |
duration |
|
| X |
- DefinitionAmount of currency on hand as well as demand deposits with banks or financial institutions. Includes other kinds of accounts that have the general characteristics of demand deposits. Also includes short-term, highly liquid investments that are both readily convertible to known amounts of cash and so near their maturity that they present insignificant risk of changes in value because of changes in interest rates. Excludes cash and cash equivalents within disposal group and discontinued operation. Reference 1: http://www.xbrl.org/2003/role/disclosureRef
-Topic 210
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.5-02(1))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480566/210-10-S99-1
Reference 2: http://www.xbrl.org/2003/role/exampleRef
-Topic 210
-SubTopic 10
-Name Accounting Standards Codification
-Section 45
-Paragraph 1
-Subparagraph (a)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147483467/210-10-45-1
Reference 3: http://fasb.org/us-gaap/role/ref/legacyRef
-Name Accounting Standards Codification
-Topic 230
-SubTopic 10
-Section 45
-Paragraph 4
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482740/230-10-45-4
| Name: |
us-gaap_CashAndCashEquivalentsAtCarryingValue |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:monetaryItemType |
| Balance Type: |
debit |
| Period Type: |
instant |
|
| X |
- DefinitionAmount of cash and cash equivalents, and cash and cash equivalents restricted to withdrawal or usage. Excludes amount for disposal group and discontinued operations. Cash includes, but is not limited to, currency on hand, demand deposits with banks or financial institutions, and other accounts with general characteristics of demand deposits. Cash equivalents include, but are not limited to, short-term, highly liquid investments that are both readily convertible to known amounts of cash and so near their maturity that they present insignificant risk of changes in value because of changes in interest rates. Reference 1: http://www.xbrl.org/2003/role/disclosureRef
-Topic 230
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 8
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482913/230-10-50-8
Reference 2: http://fasb.org/us-gaap/role/ref/legacyRef
-Topic 230
-SubTopic 10
-Name Accounting Standards Codification
-Section 45
-Paragraph 24
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482740/230-10-45-24
Reference 3: http://fasb.org/us-gaap/role/ref/legacyRef
-Name Accounting Standards Codification
-Topic 230
-SubTopic 10
-Section 45
-Paragraph 4
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482740/230-10-45-4
| Name: |
us-gaap_CashCashEquivalentsRestrictedCashAndRestrictedCashEquivalents |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:monetaryItemType |
| Balance Type: |
debit |
| Period Type: |
instant |
|
| X |
- References
+ Details
| Name: |
us-gaap_CashCashEquivalentsRestrictedCashAndRestrictedCashEquivalentsAbstract |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:stringItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionAmount of increase (decrease) in cash, cash equivalents, and cash and cash equivalents restricted to withdrawal or usage; including effect from exchange rate change. Cash includes, but is not limited to, currency on hand, demand deposits with banks or financial institutions, and other accounts with general characteristics of demand deposits. Cash equivalents include, but are not limited to, short-term, highly liquid investments that are both readily convertible to known amounts of cash and so near their maturity that they present insignificant risk of changes in value because of changes in interest rates. Reference 1: http://fasb.org/us-gaap/role/ref/legacyRef
-Topic 230
-SubTopic 10
-Name Accounting Standards Codification
-Section 45
-Paragraph 24
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482740/230-10-45-24
Reference 2: http://fasb.org/us-gaap/role/ref/legacyRef
-Name Accounting Standards Codification
-Section 45
-Paragraph 1
-SubTopic 230
-Topic 830
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147477401/830-230-45-1
| Name: |
us-gaap_CashCashEquivalentsRestrictedCashAndRestrictedCashEquivalentsPeriodIncreaseDecreaseIncludingExchangeRateEffect |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:monetaryItemType |
| Balance Type: |
debit |
| Period Type: |
duration |
|
| X |
- References
+ Details
| Name: |
us-gaap_CashFlowNoncashInvestingAndFinancingActivitiesDisclosureAbstract |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:stringItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionThe current period expense charged against earnings on long-lived, physical assets not used in production, and which are not intended for resale, to allocate or recognize the cost of such assets over their useful lives; or to record the reduction in book value of an intangible asset over the benefit period of such asset; or to reflect consumption during the period of an asset that is not used in production. Reference 1: http://fasb.org/us-gaap/role/ref/legacyRef
-Name Accounting Standards Codification
-Section 45
-Paragraph 28
-Subparagraph (b)
-SubTopic 10
-Topic 230
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482740/230-10-45-28
Reference 2: http://fasb.org/us-gaap/role/ref/legacyRef
-Name Accounting Standards Codification
-Topic 360
-SubTopic 10
-Section 50
-Paragraph 1
-Subparagraph (a)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482099/360-10-50-1
| Name: |
us-gaap_DepreciationAndAmortization |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:monetaryItemType |
| Balance Type: |
debit |
| Period Type: |
duration |
|
| X |
- DefinitionThe increase (decrease) during the reporting period in amount due within one year (or one business cycle) from customers for the credit sale of goods and services. Reference 1: http://fasb.org/us-gaap/role/ref/legacyRef
-Name Accounting Standards Codification
-Section 45
-Paragraph 28
-Subparagraph (a)
-SubTopic 10
-Topic 230
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482740/230-10-45-28
| Name: |
us-gaap_IncreaseDecreaseInAccountsReceivable |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:monetaryItemType |
| Balance Type: |
credit |
| Period Type: |
duration |
|
| X |
- DefinitionAmount of increase (decrease) in obligation to transfer good or service to customer for which consideration has been received or is receivable. Reference 1: http://www.xbrl.org/2003/role/disclosureRef
-Topic 912
-SubTopic 310
-Name Accounting Standards Codification
-Section 45
-Paragraph 11
-Subparagraph (b)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147478345/912-310-45-11
Reference 2: http://www.xbrl.org/2009/role/commonPracticeRef
-Topic 230
-SubTopic 10
-Name Accounting Standards Codification
-Section 45
-Paragraph 28
-Subparagraph (a)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482740/230-10-45-28
| Name: |
us-gaap_IncreaseDecreaseInContractWithCustomerLiability |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:monetaryItemType |
| Balance Type: |
debit |
| Period Type: |
duration |
|
| X |
- References
+ Details
| Name: |
us-gaap_IncreaseDecreaseInOperatingCapitalAbstract |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:stringItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionAmount of increase (decrease) in obligation for operating lease. Reference 1: http://www.xbrl.org/2009/role/commonPracticeRef
-Topic 230
-SubTopic 10
-Name Accounting Standards Codification
-Section 45
-Paragraph 28
-Subparagraph (a)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482740/230-10-45-28
Reference 2: http://www.xbrl.org/2009/role/commonPracticeRef
-Name Accounting Standards Codification
-Section 50
-Paragraph 4
-Subparagraph (g)(1)
-SubTopic 20
-Topic 842
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147478964/842-20-50-4
| Name: |
us-gaap_IncreaseDecreaseInOperatingLeaseLiability |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:monetaryItemType |
| Balance Type: |
debit |
| Period Type: |
duration |
|
| X |
- DefinitionThe increase (decrease) during the reporting period in other obligations or expenses incurred but not yet paid. Reference 1: http://fasb.org/us-gaap/role/ref/legacyRef
-Name Accounting Standards Codification
-Section 45
-Paragraph 28
-Subparagraph (a)
-SubTopic 10
-Topic 230
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482740/230-10-45-28
| Name: |
us-gaap_IncreaseDecreaseInOtherAccountsPayableAndAccruedLiabilities |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:monetaryItemType |
| Balance Type: |
debit |
| Period Type: |
duration |
|
| X |
- DefinitionAmount of increase (decrease) in operating assets classified as other. Reference 1: http://fasb.org/us-gaap/role/ref/legacyRef
-Name Accounting Standards Codification
-Section 45
-Paragraph 28
-Subparagraph (a)
-SubTopic 10
-Topic 230
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482740/230-10-45-28
| Name: |
us-gaap_IncreaseDecreaseInOtherOperatingAssets |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:monetaryItemType |
| Balance Type: |
credit |
| Period Type: |
duration |
|
| X |
- DefinitionAmount of increase (decrease) in prepaid expenses, and assets classified as other. Reference 1: http://fasb.org/us-gaap/role/ref/legacyRef
-Name Accounting Standards Codification
-Section 45
-Paragraph 28
-Subparagraph (a)
-SubTopic 10
-Topic 230
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482740/230-10-45-28
| Name: |
us-gaap_IncreaseDecreaseInPrepaidDeferredExpenseAndOtherAssets |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:monetaryItemType |
| Balance Type: |
credit |
| Period Type: |
duration |
|
| X |
- DefinitionAmount of cash paid for interest, excluding capitalized interest, classified as operating activity. Includes, but is not limited to, payment to settle zero-coupon bond for accreted interest of debt discount and debt instrument with insignificant coupon interest rate in relation to effective interest rate of borrowing attributable to accreted interest of debt discount. Reference 1: http://www.xbrl.org/2003/role/disclosureRef
-Topic 230
-SubTopic 10
-Name Accounting Standards Codification
-Section 45
-Paragraph 17
-Subparagraph (d)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482740/230-10-45-17
Reference 2: http://www.xbrl.org/2003/role/disclosureRef
-Topic 230
-SubTopic 10
-Name Accounting Standards Codification
-Section 45
-Paragraph 25
-Subparagraph (e)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482740/230-10-45-25
Reference 3: http://www.xbrl.org/2003/role/disclosureRef
-Topic 230
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 2
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482913/230-10-50-2
| Name: |
us-gaap_InterestPaidNet |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:monetaryItemType |
| Balance Type: |
credit |
| Period Type: |
duration |
|
| X |
- DefinitionAmount of accretion of purchase discount on nonoperating securities. Reference 1: http://fasb.org/us-gaap/role/ref/legacyRef
-Topic 220
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 2
-Subparagraph (SX 210.5-03(8))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147483621/220-10-S99-2
| Name: |
us-gaap_InvestmentIncomeAmortizationOfDiscount |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:monetaryItemType |
| Balance Type: |
credit |
| Period Type: |
duration |
|
| X |
- DefinitionAmount of cash inflow (outflow) from financing activities, including discontinued operations. Financing activity cash flows include obtaining resources from owners and providing them with a return on, and a return of, their investment; borrowing money and repaying amounts borrowed, or settling the obligation; and obtaining and paying for other resources obtained from creditors on long-term credit. Reference 1: http://www.xbrl.org/2003/role/disclosureRef
-Topic 230
-SubTopic 10
-Name Accounting Standards Codification
-Section 45
-Paragraph 24
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482740/230-10-45-24
| Name: |
us-gaap_NetCashProvidedByUsedInFinancingActivities |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:monetaryItemType |
| Balance Type: |
debit |
| Period Type: |
duration |
|
| X |
- References
+ Details
| Name: |
us-gaap_NetCashProvidedByUsedInFinancingActivitiesAbstract |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:stringItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionAmount of cash inflow (outflow) from investing activities, including discontinued operations. Investing activity cash flows include making and collecting loans and acquiring and disposing of debt or equity instruments and property, plant, and equipment and other productive assets. Reference 1: http://www.xbrl.org/2003/role/disclosureRef
-Topic 230
-SubTopic 10
-Name Accounting Standards Codification
-Section 45
-Paragraph 24
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482740/230-10-45-24
| Name: |
us-gaap_NetCashProvidedByUsedInInvestingActivities |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:monetaryItemType |
| Balance Type: |
debit |
| Period Type: |
duration |
|
| X |
- References
+ Details
| Name: |
us-gaap_NetCashProvidedByUsedInInvestingActivitiesAbstract |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:stringItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionAmount of cash inflow (outflow) from operating activities, including discontinued operations. Operating activity cash flows include transactions, adjustments, and changes in value not defined as investing or financing activities. Reference 1: http://fasb.org/us-gaap/role/ref/legacyRef
-Topic 230
-SubTopic 10
-Name Accounting Standards Codification
-Section 45
-Paragraph 28
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482740/230-10-45-28
Reference 2: http://fasb.org/us-gaap/role/ref/legacyRef
-Topic 230
-SubTopic 10
-Name Accounting Standards Codification
-Section 45
-Paragraph 24
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482740/230-10-45-24
Reference 3: http://fasb.org/us-gaap/role/ref/legacyRef
-Topic 230
-SubTopic 10
-Name Accounting Standards Codification
-Section 45
-Paragraph 25
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482740/230-10-45-25
| Name: |
us-gaap_NetCashProvidedByUsedInOperatingActivities |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:monetaryItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- References
+ Details
| Name: |
us-gaap_NetCashProvidedByUsedInOperatingActivitiesAbstract |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:stringItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionAmount of periodic reduction over lease term of carrying amount of right-of-use asset from operating lease. Reference 1: http://www.xbrl.org/2009/role/commonPracticeRef
-Topic 230
-SubTopic 10
-Name Accounting Standards Codification
-Section 45
-Paragraph 28
-Subparagraph (b)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482740/230-10-45-28
| Name: |
us-gaap_OperatingLeaseRightOfUseAssetAmortizationExpense |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:monetaryItemType |
| Balance Type: |
debit |
| Period Type: |
duration |
|
| X |
- DefinitionThe cash outflow paid to third parties in connection with debt origination, which will be amortized over the remaining maturity period of the associated long-term debt. Reference 1: http://fasb.org/us-gaap/role/ref/legacyRef
-Name Accounting Standards Codification
-Topic 230
-SubTopic 10
-Section 45
-Paragraph 15
-Subparagraph (e)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482740/230-10-45-15
| Name: |
us-gaap_PaymentsOfDebtIssuanceCosts |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:monetaryItemType |
| Balance Type: |
credit |
| Period Type: |
duration |
|
| X |
- DefinitionThe cash outflow associated with the purchase of all investments (debt, security, other) during the period. Reference 1: http://fasb.org/us-gaap/role/ref/legacyRef
-Topic 230
-SubTopic 10
-Name Accounting Standards Codification
-Section 45
-Paragraph 13
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482740/230-10-45-13
| Name: |
us-gaap_PaymentsToAcquireInvestments |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:monetaryItemType |
| Balance Type: |
credit |
| Period Type: |
duration |
|
| X |
- DefinitionThe cash outflow associated with the acquisition of long-lived, physical assets that are used in the normal conduct of business to produce goods and services and not intended for resale; includes cash outflows to pay for construction of self-constructed assets. Reference 1: http://fasb.org/us-gaap/role/ref/legacyRef
-Topic 230
-SubTopic 10
-Name Accounting Standards Codification
-Section 45
-Paragraph 13
-Subparagraph (c)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482740/230-10-45-13
| Name: |
us-gaap_PaymentsToAcquirePropertyPlantAndEquipment |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:monetaryItemType |
| Balance Type: |
credit |
| Period Type: |
duration |
|
| X |
- DefinitionThe cash inflow from a debt initially having maturity due after one year or beyond the operating cycle, if longer. Reference 1: http://www.xbrl.org/2003/role/disclosureRef
-Topic 946
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 3
-Subparagraph (SX 210.6-03(i)(1))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147479886/946-10-S99-3
Reference 2: http://fasb.org/us-gaap/role/ref/legacyRef
-Name Accounting Standards Codification
-Topic 230
-SubTopic 10
-Section 45
-Paragraph 14
-Subparagraph (b)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482740/230-10-45-14
| Name: |
us-gaap_ProceedsFromIssuanceOfLongTermDebt |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:monetaryItemType |
| Balance Type: |
debit |
| Period Type: |
duration |
|
| X |
- DefinitionThe cash inflow from maturities, prepayments, calls and collections of all investments, including securities and other assets, having ready marketability and intended by management to be liquidated, if necessary, beyond the current operating cycle. Reference 1: http://www.xbrl.org/2009/role/commonPracticeRef
-Name Accounting Standards Codification
-Section 45
-Paragraph 12
-SubTopic 10
-Topic 230
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482740/230-10-45-12
| Name: |
us-gaap_ProceedsFromMaturitiesPrepaymentsAndCallsOfLongtermInvestments |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:monetaryItemType |
| Balance Type: |
debit |
| Period Type: |
duration |
|
| X |
- DefinitionAmount of cash inflow from a noncontrolling interest. Includes, but is not limited to, purchase of additional shares or other increase in noncontrolling interest ownership. Reference 1: http://fasb.org/us-gaap/role/ref/legacyRef
-Name Accounting Standards Codification
-Topic 230
-SubTopic 10
-Section 45
-Paragraph 14
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482740/230-10-45-14
| Name: |
us-gaap_ProceedsFromMinorityShareholders |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:monetaryItemType |
| Balance Type: |
debit |
| Period Type: |
duration |
|
| X |
- DefinitionThe consolidated profit or loss for the period, net of income taxes, including the portion attributable to the noncontrolling interest. Reference 1: http://www.xbrl.org/2003/role/disclosureRef
-Topic 250
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 6
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147483443/250-10-50-6
Reference 2: http://www.xbrl.org/2003/role/disclosureRef
-Topic 250
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 9
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147483443/250-10-50-9
Reference 3: http://www.xbrl.org/2003/role/disclosureRef
-Topic 805
-SubTopic 60
-Name Accounting Standards Codification
-Section 65
-Paragraph 1
-Subparagraph (g)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147476176/805-60-65-1
Reference 4: http://www.xbrl.org/2003/role/disclosureRef
-Topic 740
-SubTopic 323
-Name Accounting Standards Codification
-Section 65
-Paragraph 2
-Subparagraph (g)(3)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147478666/740-323-65-2
Reference 5: http://www.xbrl.org/2003/role/disclosureRef
-Topic 235
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.4-08(g)(1)(ii))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480678/235-10-S99-1
Reference 6: http://www.xbrl.org/2003/role/disclosureRef
-Topic 323
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 3
-Subparagraph (c)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147481687/323-10-50-3
Reference 7: http://www.xbrl.org/2003/role/disclosureRef
-Topic 825
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 28
-Subparagraph (f)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482907/825-10-50-28
Reference 8: http://www.xbrl.org/2003/role/disclosureRef
-Topic 250
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 1
-Subparagraph (b)(2)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147483443/250-10-50-1
Reference 9: http://www.xbrl.org/2003/role/disclosureRef
-Topic 815
-SubTopic 40
-Name Accounting Standards Codification
-Section 65
-Paragraph 1
-Subparagraph (f)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480175/815-40-65-1
Reference 10: http://www.xbrl.org/2003/role/disclosureRef
-Topic 250
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 8
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147483443/250-10-50-8
Reference 11: http://www.xbrl.org/2003/role/exampleRef
-Topic 946
-SubTopic 830
-Name Accounting Standards Codification
-Section 55
-Paragraph 11
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147479168/946-830-55-11
Reference 12: http://www.xbrl.org/2003/role/disclosureRef
-Topic 946
-SubTopic 205
-Name Accounting Standards Codification
-Section 45
-Paragraph 3
-Subparagraph (a)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147478009/946-205-45-3
Reference 13: http://www.xbrl.org/2003/role/disclosureRef
-Topic 946
-SubTopic 220
-Name Accounting Standards Codification
-Section 45
-Paragraph 7
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147479105/946-220-45-7
Reference 14: http://www.xbrl.org/2003/role/disclosureRef
-Topic 944
-SubTopic 220
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.7-04(16))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147477250/944-220-S99-1
Reference 15: http://www.xbrl.org/2003/role/disclosureRef
-Topic 946
-SubTopic 220
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.6-07(9))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147479134/946-220-S99-1
Reference 16: http://www.xbrl.org/2003/role/disclosureRef
-Topic 946
-SubTopic 220
-Name Accounting Standards Codification
-Section S99
-Paragraph 3
-Subparagraph (SX 210.6-09(1)(d))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147479134/946-220-S99-3
Reference 17: http://www.xbrl.org/2003/role/disclosureRef
-Topic 810
-SubTopic 10
-Name Accounting Standards Codification
-Section 45
-Paragraph 19
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147481231/810-10-45-19
Reference 18: http://www.xbrl.org/2009/role/commonPracticeRef
-Topic 220
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 6
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482765/220-10-50-6
Reference 19: http://www.xbrl.org/2003/role/disclosureRef
-Topic 470
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1A
-Subparagraph (SX 210.13-01(a)(4)(i))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480097/470-10-S99-1A
Reference 20: http://www.xbrl.org/2009/role/commonPracticeRef
-Topic 470
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1A
-Subparagraph (SX 210.13-01(a)(4)(ii))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480097/470-10-S99-1A
Reference 21: http://www.xbrl.org/2003/role/disclosureRef
-Topic 470
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1A
-Subparagraph (SX 210.13-01(a)(4)(iii)(A))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480097/470-10-S99-1A
Reference 22: http://www.xbrl.org/2003/role/disclosureRef
-Topic 470
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1A
-Subparagraph (SX 210.13-01(a)(4)(iv))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480097/470-10-S99-1A
Reference 23: http://www.xbrl.org/2003/role/disclosureRef
-Topic 470
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1A
-Subparagraph (SX 210.13-01(a)(5))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480097/470-10-S99-1A
Reference 24: http://www.xbrl.org/2003/role/disclosureRef
-Topic 470
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1B
-Subparagraph (SX 210.13-02(a)(4)(i))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480097/470-10-S99-1B
Reference 25: http://www.xbrl.org/2003/role/disclosureRef
-Topic 470
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1B
-Subparagraph (SX 210.13-02(a)(4)(iii)(A))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480097/470-10-S99-1B
Reference 26: http://www.xbrl.org/2003/role/disclosureRef
-Topic 470
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1B
-Subparagraph (SX 210.13-02(a)(4)(iii)(B))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480097/470-10-S99-1B
Reference 27: http://www.xbrl.org/2003/role/disclosureRef
-Topic 470
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1B
-Subparagraph (SX 210.13-02(a)(4)(iv))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480097/470-10-S99-1B
Reference 28: http://www.xbrl.org/2003/role/disclosureRef
-Topic 470
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1B
-Subparagraph (SX 210.13-02(a)(5))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480097/470-10-S99-1B
Reference 29: http://www.xbrl.org/2003/role/disclosureRef
-Topic 942
-SubTopic 235
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.9-05(b)(2))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147477314/942-235-S99-1
Reference 30: http://www.xbrl.org/2003/role/disclosureRef
-Topic 205
-SubTopic 20
-Name Accounting Standards Codification
-Section 50
-Paragraph 7
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147483499/205-20-50-7
Reference 31: http://www.xbrl.org/2003/role/exampleRef
-Topic 810
-SubTopic 10
-Name Accounting Standards Codification
-Section 55
-Paragraph 4J
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147481175/810-10-55-4J
Reference 32: http://www.xbrl.org/2003/role/exampleRef
-Topic 810
-SubTopic 10
-Name Accounting Standards Codification
-Section 55
-Paragraph 4K
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147481175/810-10-55-4K
Reference 33: http://www.xbrl.org/2003/role/disclosureRef
-Topic 220
-SubTopic 10
-Name Accounting Standards Codification
-Section 45
-Paragraph 1A
-Subparagraph (a)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482790/220-10-45-1A
Reference 34: http://www.xbrl.org/2003/role/disclosureRef
-Topic 220
-SubTopic 10
-Name Accounting Standards Codification
-Section 45
-Paragraph 1B
-Subparagraph (a)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482790/220-10-45-1B
Reference 35: http://www.xbrl.org/2003/role/disclosureRef
-Topic 230
-SubTopic 10
-Name Accounting Standards Codification
-Section 45
-Paragraph 2
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482740/230-10-45-2
Reference 36: http://www.xbrl.org/2003/role/disclosureRef
-Topic 810
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 1A
-Subparagraph (a)(1)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147481203/810-10-50-1A
Reference 37: http://www.xbrl.org/2003/role/disclosureRef
-Topic 810
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 1A
-Subparagraph (c)(1)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147481203/810-10-50-1A
| Name: |
us-gaap_ProfitLoss |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:monetaryItemType |
| Balance Type: |
credit |
| Period Type: |
duration |
|
| X |
- DefinitionAmount of expense (reversal of expense) for expected credit loss on accounts receivable. Reference 1: http://www.xbrl.org/2003/role/disclosureRef
-Topic 326
-SubTopic 20
-Name Accounting Standards Codification
-Section 50
-Paragraph 13
-Subparagraph (b)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147479319/326-20-50-13
Reference 2: http://www.xbrl.org/2003/role/disclosureRef
-Topic 220
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 2
-Subparagraph (SX 210.5-03(5))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147483621/220-10-S99-2
| Name: |
us-gaap_ProvisionForDoubtfulAccounts |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:monetaryItemType |
| Balance Type: |
debit |
| Period Type: |
duration |
|
| X |
- DefinitionAmount of cash and cash equivalents restricted as to withdrawal or usage. Cash includes, but is not limited to, currency on hand, demand deposits with banks or financial institutions, and other accounts with general characteristics of demand deposits. Cash equivalents include, but are not limited to, short-term, highly liquid investments that are both readily convertible to known amounts of cash and so near their maturity that they present insignificant risk of changes in value because of changes in interest rates. Reference 1: http://www.xbrl.org/2003/role/disclosureRef
-Topic 210
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.5-02(1))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480566/210-10-S99-1
Reference 2: http://www.xbrl.org/2003/role/disclosureRef
-Topic 944
-SubTopic 210
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.7-03(a)(2))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147478777/944-210-S99-1
Reference 3: http://www.xbrl.org/2003/role/disclosureRef
-Topic 230
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 8
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482913/230-10-50-8
Reference 4: http://fasb.org/us-gaap/role/ref/legacyRef
-Topic 942
-SubTopic 210
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.9-03(1)(a))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147478546/942-210-S99-1
Reference 5: http://fasb.org/us-gaap/role/ref/legacyRef
-Name Accounting Standards Codification
-Topic 230
-SubTopic 10
-Section 45
-Paragraph 4
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482740/230-10-45-4
| Name: |
us-gaap_RestrictedCashAndCashEquivalents |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:monetaryItemType |
| Balance Type: |
debit |
| Period Type: |
instant |
|
| X |
- DefinitionAmount of noncash expense for share-based payment arrangement. Reference 1: http://fasb.org/us-gaap/role/ref/legacyRef
-Name Accounting Standards Codification
-Section 45
-Paragraph 28
-Subparagraph (a)
-SubTopic 10
-Topic 230
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482740/230-10-45-28
| Name: |
us-gaap_ShareBasedCompensation |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:monetaryItemType |
| Balance Type: |
debit |
| Period Type: |
duration |
|
v3.24.2.u1
Organization
|
6 Months Ended |
Jun. 30, 2024 |
|---|
| Organization, Consolidation and Presentation of Financial Statements [Abstract] |
|
| Organization |
Organization Alignment Healthcare, Inc. (collectively, “we” or “us” or “our” or the “Company”), is a next generation, consumer-centric health care platform that is purpose-built to provide seniors with high quality, affordable care with a vastly improved consumer experience. Enabled by our innovative technology and care delivery model, the Company focuses on improving outcomes in the Medicare Advantage sector. The Company’s operations primarily consist of Medicare Advantage Plans in the states of California, North Carolina, Nevada, Arizona, Florida and Texas.
|
| X |
- References
+ Details
| Name: |
us-gaap_OrganizationConsolidationAndPresentationOfFinancialStatementsAbstract |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:stringItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionThe entire disclosure for organization, consolidation and basis of presentation of financial statements disclosure. Reference 1: http://www.xbrl.org/2003/role/disclosureRef
-Topic 946
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 1
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480424/946-10-50-1
Reference 2: http://www.xbrl.org/2003/role/disclosureRef
-Topic 946
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 2
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480424/946-10-50-2
Reference 3: http://fasb.org/us-gaap/role/ref/legacyRef
-Topic 810
-Name Accounting Standards Codification
-Publisher FASB
-URI https://asc.fasb.org/810/tableOfContent
Reference 4: http://fasb.org/us-gaap/role/ref/legacyRef
-Topic 205
-Name Accounting Standards Codification
-Publisher FASB
-URI https://asc.fasb.org/205/tableOfContent
| Name: |
us-gaap_OrganizationConsolidationAndPresentationOfFinancialStatementsDisclosureTextBlock |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
dtr-types:textBlockItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
v3.24.2.u1
Summary of Significant Accounting Policies
|
6 Months Ended |
Jun. 30, 2024 |
|---|
| Accounting Policies [Abstract] |
|
| Summary of Significant Accounting Policies |
Summary of Significant Accounting Policies Basis of Presentation The accompanying condensed consolidated financial statements and accompanying notes have been prepared in accordance with accounting principles generally accepted in the United States of America (“U.S. GAAP”). The balance sheet as of December 31, 2023, included herein, was derived from audited financial statements, but does not include all disclosures required by GAAP. In accordance with the rules and regulations of the U.S. Securities and Exchange Commission ("SEC"), the Company has omitted certain footnote disclosures that would substantially duplicate the disclosures contained in its annual audited consolidated financial statements. Therefore, these condensed consolidated financial statements should be read in conjunction with the Company's Annual Report on Form 10-K for the year-ended December 31, 2023 as filed with the SEC. Furthermore, the condensed consolidated financial statements include the accounts of the Company, our subsidiaries, and three immaterial variable interest entities in which we are the primary beneficiary. All intercompany transactions have been eliminated in consolidation. Noncontrolling interest is presented within the equity section of the condensed consolidated balance sheets. We have no components of other comprehensive income (loss), and accordingly, comprehensive income (loss) is the same as the net income (loss) for all periods presented. Use of Estimates The preparation of the condensed consolidated financial statements requires management to make estimates and judgments that affect the amounts reported in the condensed consolidated financial statements. Our significant estimates include, but are not limited to, the determination of medical expenses payable; the impact of risk adjustment provisions related to our Medicare contracts; collectability of receivables; valuation of related impairment recognition of long-lived assets, including goodwill and intangible assets; equity-based compensation expense; and contingent liabilities. Estimates and judgments are based upon historical information and on various other assumptions that are believed to be reasonable under the circumstances. Actual results could differ materially from those estimates and the impact of any change in estimates is included in earnings in the period in which the estimate is adjusted. Segments We have determined that our chief executive officer is the chief operating decision maker (“CODM”) who regularly reviews financial operating results on a consolidated basis for purposes of allocating resources and evaluating financial performance. We operate and manage the business as one reportable segment and one operating segment, which is to provide healthcare services to our seniors. Factors used in determining the reportable segment include the nature of operating activities, our organizational and reporting structure, and the type of information reviewed by the CODM to allocate resources and evaluate financial performance. All of our assets are located in the United States. Fair Value Measurements Fair value is the price that would be received to sell an asset or paid to transfer a liability in an orderly transaction between market participants at the measurement date. Our current assets and current liabilities approximate fair value because of the short-term nature of these financial instruments. Financial instruments measured at fair value on a recurring basis were based upon a three-tier hierarchy as follows: Level 1 - Quoted prices in active markets for identical assets or liabilities Level 2 - Other inputs that are observable for the asset or liability, either directly or indirectly, for substantially the full term of the asset or liability Level 3 - Unobservable inputs that reflect management’s best estimate of what market participants would use in pricing the asset or liability at the measurement date The fair value of cash, cash equivalents, restricted cash and U.S. Treasury bills was determined based on Level 1 inputs. The fair value of certificate of deposits, which are recorded in other assets in the condensed consolidated balance sheets, was determined based on Level 2 inputs. There were no assets or liabilities measured at fair value using Level 3 inputs as of June 30, 2024 and December 31, 2023. Our long-term debt was reported at carrying value. Revenue and Accounts Receivable Earned premium revenue consisted of premium revenue and capitation revenue for the three and six months ended June 30, 2024 and 2023 were as follows: | | | | | | | | | | | | | | | | | | | | | | | | | Three Months Ended
June 30, | | Six Months Ended
June 30, | | 2024 | | 2023 | | 2024 | | 2023 | | Premium | $ | 673,532 | | | $ | 424,704 | | | $ | 1,293,254 | | | $ | 824,444 | | | Capitation | 562 | | | 32,173 | | | 2,396 | | | 67,245 | | | Total | $ | 674,094 | | | $ | 456,877 | | | $ | 1,295,650 | | | $ | 891,689 | |
Premium revenue is derived monthly from the federal government based on our contracts with the Centers for Medicare and Medicaid Services (“CMS”). In accordance with these arrangements, we assume the responsibility for the outcomes and the economic risk of funding our members’ health care, supplemental benefits and related administration costs. We recognize premium revenue in the month that members are entitled to receive health care services, and premiums collected in advance are deferred. The monthly reimbursement includes a fixed payment per member per month (“PMPM”), which is adjusted based on certain risk factors derived from medical diagnoses and conditions of our members. The adjustments are estimated by projecting the ultimate annual premium and are recognized ratably during the year, with adjustments each period to reflect changes in the estimated ultimate premium. Premiums are also recorded net of estimated uncollectible amounts and retroactive membership adjustments. Capitation revenue consists primarily of capitated fees for medical care services provided by us under arrangements with third-party payors. In 2023, capitation revenue consisted primarily of revenue from CMS related to our participation in the CMS "ACO Realizing Equity, Access, and Community Health Model” or “ACO REACH” model, as discussed below. Under those arrangements with third-party payors, we receive a PMPM payment for a defined member population, and we are responsible for providing health care services to the member population over the contract period. We are solely responsible for the cost of health care services related to the member population and in some cases, we are financially responsible for the supplemental benefits provided by us to the members. We act as a principal in arranging for and controlling the services provided by our provider network and we are at risk for arranging and providing health care services. The premium and capitation payments we receive monthly from CMS for our members are determined from our annual bid or similarly from third-party payors under our capitation arrangement. These payments represent revenues for providing health care coverage, including Medicare Part D benefits. Under the Medicare Part D program, our members and the members of the third-party payors receive standard drug benefits. We may also provide enhanced benefits at our own expense. We recognize premium or capitation revenue for providing this insurance coverage in the month that members are entitled to receive health care services and any premium or capitation collected in advance is deferred. Our CMS payment related to Medicare Part D is subject to risk sharing through the Medicare Part D risk corridor provisions. We also participate in the CMS ACO REACH program, formerly the Direct Contracting Model ("DCE"). CMS serves as the claim adjudicator for institutional and specialists care, and directly pays for such fee for service claims. The ACO REACH entity ("ACO") is responsible for the cost of health care services related to the patient population attributed to the ACO by participating in 100% savings/losses via the risk share model and in some cases, are financially responsible for the supplemental benefits provided to the patients. In 2024, we entered into a management services and risk management agreement with a third-party healthcare company. The third party will be responsible for arranging and controlling the health care services provided to the ACO members, and for providing certain management and support services with respect to ACO operations. The third party will also assume specified upside and downside financial risk relative to the ACO’s performance. As a result of this arrangement, revenue is recorded on a net basis within other revenue on the condensed consolidated statement of operations for the three and six months ended June 30, 2024. Revenue recognized by the ACO for the three and six months ended June 30, 2024 was $(744) and $241, respectively. Prior to 2024, the ACO acted as a principal in arranging for and controlling services provided directly by their contracts with primary care physicians, as well as services provided by preferred institutional care providers and specialists. Capitation payments for the ACO program were determined from an annual benchmark established by CMS. These payments, which were adjusted for variable considerations, represented revenue for providing health care services, including primary care as well as institutional and specialist care. The ACO recognized capitation revenue for providing these services in the period in which the performance obligations were satisfied by transferring services to the members. Revenue recognized by the ACO for the three and six months ended June 30, 2023 was $30,113 and $62,227, respectively. Interest income earned on our cash deposits and short-term investments is included within other revenue on the condensed consolidated statements of operations. Interest income for the three and six months ended June 30, 2024 was $5,602 and $11,045, respectively. Interest income for the three and six months ended June 30, 2023 was $4,727 and $8,444, respectively. Revenue Adjustments Payments by CMS to health plans are determined via a competitive bidding process with CMS and are based upon the cost of care in a local market and the average utilization of services by the member enrolled. These payments are subject to periodic adjustments under CMS’ “risk adjustment model,” which compensates health plans based on the health severity and certain demographic factors of each individual member. Members diagnosed with certain conditions are paid at a higher monthly payment than members who are healthier. Under this risk adjustment model, CMS calculates the risk adjustment payment using diagnosis data from hospital inpatient, hospital outpatient, and physician treatment settings. The Company and health care providers collect, capture, and submit the necessary and available diagnosis data to CMS within prescribed deadlines. Both premium and capitation revenues (including Medicare Part D) are subject to adjustments under the risk adjustment model. Throughout the year, we estimate risk adjustment payments based upon the diagnosis data submitted and expected to be submitted to CMS. Those estimated risk adjustment payments are recorded as an adjustment to premium and capitation revenue. Our risk adjustment data is also subject to review by the government, including audit by regulators. Our recognized premium revenue for our Medicare Advantage Plans in California, North Carolina, Nevada, Arizona, Texas and Florida are each subject to a minimum annual medical loss ratio (“MLR”) of 85%. The MLR represents medical costs as a percentage of premium revenue. The Code of Federal Regulations defines what constitutes medical costs and premium revenue, including certain additional expenses related to improving the quality of care provided, and the exclusion of certain taxes and fees, in each case as permitted or required by CMS and applicable regulatory requirements. If the minimum MLR is not met, we are required to remit a portion of the premiums back to the federal government. The amount remitted, if any, is recognized as an adjustment to premium revenues in the condensed consolidated statements of operations. The amounts payable under this provision were immaterial at June 30, 2024 and December 31, 2023. Medicare Part D payments are also subject to a federal risk corridor program, which limits a health plan’s overall losses or profit if actual spending for basic Medicare Part D benefits is much higher or lower than what was anticipated. Risk corridor is recorded within premium revenue. The risk corridor provisions compare costs targeted in our bids or third-party payors’ bids to actual prescription drug costs, limited to actual costs that would have been incurred under the standard coverage as defined by CMS. Variances exceeding certain thresholds may result in CMS or third-party payors making additional payments to us or require us to refund a portion of the premiums we received. We estimate and recognize an adjustment to premium revenue related to these provisions based upon pharmacy claims experience. We record a receivable or payable at the contract level and classify the amount as current or long-term in our condensed consolidated balance sheet based on the timing of expected settlement. Variable consideration estimates related to ACO contract revenue are based on the most likely outcome method and that a significant reversal in the amount of cumulative revenue recognized would not occur. Receivables, including risk adjusted premium due from the government or through third-party payors, pharmacy rebates, and other receivables, are shown net of allowances for credit losses and retroactive membership adjustments. Property and Equipment—Net Depreciation expense is computed using the straight-line method generally based on the following estimated useful lives: | | | | | | | Description | Estimated Service Lives (years) | | Computer and equipment | 5 | | Office equipment and furniture | 5-7 | | Software | 3-5 | | Leasehold improvements | 15 (or lease term, if shorter) |
Depreciation expense related to property and equipment used to service our members or at our clinics are included within medical expenses in the condensed consolidated statements of operations. Medical Expenses Medical expenses include claim payments, capitation payments, pharmacy costs net of rebates, allocations of certain centralized expenses, internal care delivery expenses and various other costs incurred to provide health insurance coverage and care to members, as well as estimates of future payments to hospitals and others for medical care and other supplemental benefits provided. We have contracts with a network of hospitals, physicians, and other providers and compensate those providers and ancillary organizations based on contractual arrangements or CMS Medicare compensation guidelines. We pay these contracting providers either through fee-for-service arrangement in which the provider is paid negotiated rates for specific services provided or a capitation payment, which represent monthly contractual fees disbursed for each member regardless of medical services provided to the member. We are responsible for the entirety of the cost of health care services related to the member population, in addition to supplemental benefits provided by us to our seniors. In 2023, we also recorded claims expenses related to our institutional and specialist care related to our ACO program with CMS as we acted as the principal in the transaction. As discussed above, beginning in 2024, claims expense related to the ACO program is netted against ACO revenue as we act as the agent in these transactions. Capitation-related expenses are recorded on an accrual basis during the coverage period. Expenses related to fee-for-service contracts are recorded in the period in which the related services are dispensed. Pharmacy costs represent payments for members’ prescription drug benefits, net of rebates from drug manufacturers. Receivables for such pharmacy rebates are included in accounts receivable in the condensed consolidated balance sheet. In August 2022, the Inflation Reduction Act ("IRA") was signed into law. The law intends to increase tax revenue and reduce Medicare costs through lower prescription drug prices, inflation rebates, and capping annual Medicare Part D out of pocket expenses. The provisions of the law are set to take effect over the next seven years. There was no material impact on our consolidated financial statements at June 30, 2024, and we do not anticipate a material impact to operations for the remainder of fiscal year 2024. We are in the process of evaluating the impact the IRA will have on our business for fiscal years beyond 2024. Medical Expenses Payable Medical expenses payable includes estimates of our obligations for medical care services that have been rendered on behalf of our members and the members of the third-party payors, but for which claims have either not yet been received or processed, loss adjustment expense reserve for the expected costs of settling these claims, and for liabilities related to physician, hospital, and other medical cost disputes. We develop estimates for medical expenses incurred but not yet paid (“IBNP”), which includes an estimate for claims incurred but not reported (“IBNR”) and a payable for adjudicated claims. IBNR is estimated using an actuarial process that is consistently applied and centrally controlled. Medical expenses payable also includes an estimate for the costs necessary to process unpaid claims at the end of each period. We estimate the IBNR liability using actuarial methods that are commonly used by health insurance actuaries and meet Actuarial Standards of Practice. These actuarial methods consider factors, such as cost trends and completion factors that are assessed based on historical data for payment patterns, product mix, seasonality, utilization of health care services, and other relevant factors. Each period, we re-examine previously established IBNR estimates based on actual claim submissions and other changes in facts and circumstances. As the IBNR estimates recorded in prior periods develop, we adjust the amount of the estimates and include the changes in estimates in medical expenses in the period in which the change is identified. Actuarial Standards of Practice generally require that the IBNP estimates be adequate to cover obligations under moderately adverse conditions. Moderately adverse conditions are situations in which the actual claims are expected to be higher than the otherwise estimated value of such claims at the time of estimate. In many situations, the claims amount ultimately settled will be different than the estimate that satisfies the Actuarial Standards of Practice. We include in our IBNP an estimate for medical claims liability under moderately adverse conditions, which represents the risk of adverse deviation of the estimates in our actuarial method of reserving. We believe that medical expenses payable is adequate to cover future claims payments required. However, such estimates are based on knowledge of current events and anticipated future events. Therefore, the actual liability could differ materially from the amounts provided. We reassess the profitability of contracts for providing coverage to members when current operating results or forecasts indicate probable future losses. A premium deficiency reserve is established in current operations to the extent that the sum of expected future costs, claim adjustment expenses, and maintenance costs exceed related future premiums under contracts without consideration of investment income. For purposes of determining premium deficiencies, contracts are grouped in a manner consistent with the method of acquiring, servicing, and measuring the profitability of such contracts. Losses recognized as a premium deficiency result in a beneficial effect in subsequent periods as operating losses under these contracts are charged to the liability previously established. Part D Subsidies We also receive advance payments each month from CMS related to Catastrophic Reinsurance, Coverage Gap Discount, and the Low-Income Member Cost Sharing Subsidy (“Subsidies”). Reinsurance subsidies represent funding from CMS for our portion of prescription drug costs, which exceed the member’s out-of-pocket threshold or the catastrophic coverage level. Low-income cost subsidies represent funding from CMS for all or a portion of the deductible, the coinsurance and co-payment amounts above the out-of-pocket threshold for low-income beneficiaries. Additionally, the Health Care Reform Law mandates consumer discounts of 75% on brand-name prescription drugs for Part D plan participants in the coverage gap. The majority of the discounts are funded by the pharmaceutical manufacturers, while we fund a smaller portion and administer the application of the total discount. These Subsidies represent cost reimbursements under the Medicare Part D program and are recorded as deposits or payables. These Subsidies received in excess of, or less than, actual subsidized benefits paid are refundable to or recoverable from CMS through an annual reconciliation process following the end of the contract year. Shared Risk Reserve Arrangements We established a fund (also referred to as “a pool”) for risk and profit-sharing with various independent physician associations (“IPAs”). The pool enables us and our IPAs to share in the financial responsibility and/or upside associated with providing covered medical expenses to our members. The risk pool is based on a contractually agreed upon medical budget, typically based upon a percentage of revenue. If actual medical expenses are less than the budgeted amount, this results in a surplus. Conversely, if actual medical expenses are greater than the budgeted amount, this results in a deficit. We will distribute the surplus, or a portion thereof, to each IPA based upon contractual terms. Deficits are charged to shared risk providers’ risk pool as per the contractual term and evaluated for collectability at each reporting period. We record risk-sharing receivables and payables on a gross basis on the condensed consolidated balance sheet. Throughout the year, we evaluate expected losses on risk-sharing receivables and record the resulting expected losses to the reserve. We systematically build and release reserves based on adequacy and its assessment of expected losses on a monthly basis. Credit loss associated with risk share deficit receivables are recorded within medical expense in the condensed consolidated statements of operations. As of June 30, 2024 and December 31, 2023, we recorded a valuation allowance for substantially all of the risk-sharing receivable balance due to collection risk related to the balance. The risk-sharing payable is included within medical expenses payable on the condensed consolidated balance sheet. Concentrations of Credit Risk Financial instruments that potentially subject us to concentrations of credit risk consist primarily of cash deposits and current and restricted investments with financial institutions. Accounts at each financial institution are insured by the Federal Deposit Insurance Corporation (“FDIC”) up to certain limits. At June 30, 2024 and December 31, 2023, there was $362,396 and $316,977, respectively, in excess of FDIC-insured limits. Equity-Based Compensation Equity-based compensation expense is measured and recognized based on the grant date fair value of the awards. The grant date fair value of stock options is estimated using the Black-Scholes option pricing model. The grant date fair value of restricted stock units (“RSUs”) and restricted stock awards (“RSAs”) is estimated based on the fair value of our underlying common stock on the date of grant. The Black-Scholes option pricing model requires the use of highly subjective assumptions, including the award’s expected term, the fair value of the underlying common stock, the expected volatility of the price of the common stock, risk-free interest rates, and the expected dividend yield of the common stock. The assumptions used to determine the fair value of the stock-based awards are management’s best estimates and involve inherent uncertainties and the application of judgment. The expected term represents the period the stock-based awards are expected to be outstanding. As we do not have sufficient historical experience for determining the expected term of the stock option awards granted, we utilize the simplified method available under U.S. GAAP. As we do not have a substantial trading history, volatility assumptions were developed using a combination of the Company's historical volatility and the historical volatilities of a set of peer companies, adjusted for debt-equity leverage. Equity-based compensation expense for awards with service-based vesting only is recognized on a graded vesting schedule over the requisite service period of the awards, which is generally four years. Equity-based compensation expense for RSU awards with performance-based vesting is recognized over the requisite service period on a graded vesting schedule and is only recognized when the Company concludes that it is probable that the performance condition(s) will be achieved. At each reporting period, the Company reassesses the probability of achieving the performance criteria. Determining whether the performance criteria will be achieved involves judgment, and the estimate of share-based compensation expense may be revised periodically based on changes in the probability of achieving the performance criteria. Revisions are reflected in the period in which the estimate is changed. We account for forfeitures as they occur. Equity-based compensation is recorded within selling, general and administrative expenses, and medical expenses based on the function of the applicable employee and non-employee. Noncontrolling interest In October 2022, the Company acquired a subsidiary and recorded a noncontrolling interest for the portion of equity ownership not attributable to Alignment Healthcare, Inc. The noncontrolling interest in the subsidiary was initially recognized at estimated fair value on October 1, 2022 and is presented within total equity in the Company's condensed consolidated balance sheet. The net (income) loss attributable to this noncontrolling interest was $(7) and $47, respectively, for the three and six months ended June 30, 2024. The net loss attributable to this noncontrolling interest was $17 and $104, respectively, for the three and six months ended June 30, 2023. Net Loss per Share Net loss per share is calculated based on net loss attributable to Alignment Healthcare, Inc.'s stockholders. The following table sets forth the computation of basic and diluted net loss per share for the three and six months ended June 30, 2024 and 2023: | | | | | | | | | | | | | | | | | | | | | | | | | | Three Months Ended
June 30, | | Six Months Ended
June 30, | | | 2024 | | 2023 | | 2024 | | 2023 | | Numerator: | | | | | | | | | Net loss | $ | (24,003) | | | $ | (28,494) | | | $ | (70,578) | | | $ | (65,865) | | | Less: Net (income) loss attributable to noncontrolling interests | (7) | | | 17 | | | 47 | | | 104 | | | Net loss attributable to Alignment Healthcare, Inc. | $ | (24,010) | | | $ | (28,477) | | | $ | (70,531) | | | $ | (65,761) | | | Denominator: | | | | | | | | | Total weighted-average common shares outstanding - basic and diluted | 191,431,917 | | 188,496,252 | | 190,514,927 | | 188,029,447 | | Less: Restricted shares of common stock | (540,130) | | (2,504,792) | | (566,202) | | (3,468,795) | | Total weighted-average common shares outstanding, net of restricted shares of common stock - basic and diluted | 190,891,787 | | 185,991,460 | | 189,948,725 | | 184,560,652 | | Net loss per share: | | | | | | | | | Net loss per share - basic and diluted | $ | (0.13) | | | $ | (0.15) | | | $ | (0.37) | | | $ | (0.36) | |
Basic net loss per share is the same as diluted net loss per share for periods presented as the inclusion of all potentially dilutive shares would have been anti-dilutive. In addition to the restricted shares of common stock, we also excluded the following potential common shares, presented based on amounts outstanding at each period end, from the computation of diluted net loss per share as of June 30, 2024 and 2023: | | | | | | | | | | | | | | June 30, | | | 2024 | | 2023 | | Stock options | 8,949,589 | | 10,566,529 | | Restricted stock units | 22,196,478 | | 10,145,593 | | Total | 31,146,067 | | 20,712,122 |
Recent Accounting Pronouncements Issued In November 2023, the FASB issued a new accounting standard around segment disclosures. The new standard requires a public entity to disclose significant segment expenses and other segment items on an annual and interim basis and provide, in interim periods, all disclosures about a reportable segment’s profit or loss and assets that are currently required annually. Additionally, it requires a public entity to disclose the title and position of the Chief Operating Decision Maker. The ASU does not change how a public entity identifies its operating segments, aggregates them, or applies the quantitative thresholds to determine its reportable segments. The new standard is effective for fiscal years beginning after December 15, 2023, and interim periods within fiscal years beginning after December 15, 2024, with early adoption permitted. A public entity should apply the amendments in this ASU retrospectively to all prior periods presented in the financial statements. We expect this ASU to only impact our disclosures with no impacts to our results of operations, cash flows and financial condition.
|
| X |
- References
+ Details
| Name: |
us-gaap_AccountingPoliciesAbstract |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:stringItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionThe entire disclosure for all significant accounting policies of the reporting entity. Reference 1: http://www.xbrl.org/2003/role/disclosureRef
-Topic 235
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 1
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147483426/235-10-50-1
Reference 2: http://fasb.org/us-gaap/role/ref/legacyRef
-Topic 235
-Name Accounting Standards Codification
-Publisher FASB
-URI https://asc.fasb.org/235/tableOfContent
| Name: |
us-gaap_SignificantAccountingPoliciesTextBlock |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
dtr-types:textBlockItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
v3.24.2.u1
Fair Value
|
6 Months Ended |
Jun. 30, 2024 |
|---|
| Fair Value Disclosures [Abstract] |
|
| Fair Value |
Fair Value The following tables present the carrying value and fair value of these financial instruments as of June 30, 2024 and December 31, 2023: | | | | | | | | | | | | | | | | | | | | | | | | | June 30, 2024 | | | | Fair Value | | Carrying
Value | | Level 1 | | Level 2 | | Level 3 | | U.S. Treasury bills | $ | 44,628 | | | $ | 44,577 | | | $ | — | | | $ | — | | | Certificate of deposits | 2,336 | | | — | | | 2,336 | | | — | | | Total | $ | 46,964 | | | $ | 44,577 | | | $ | 2,336 | | | $ | — | |
| | | | | | | | | | | | | | | | | | | | | | | | | December 31, 2023 | | | | Fair Value | | Carrying
Value | | Level 1 | | Level 2 | | Level 3 | | U.S. Treasury bills | $ | 117,337 | | | $ | 117,310 | | | $ | — | | | $ | — | | | Certificate of deposits | 1,755 | | | — | | | 1,755 | | | — | | | Total | $ | 119,092 | | | $ | 117,310 | | | $ | 1,755 | | | $ | — | |
The carrying value of long-term debt represents the outstanding balance, net of unamortized debt issuance costs. As of June 30, 2024 and December 31, 2023, the fair value of our long-term debt approximates the carrying value. Our nonfinancial assets and liabilities, which include goodwill, intangible assets, property, and equipment, are not required to be measured at fair value on a recurring basis. However, on a periodic basis, or whenever events or changes in circumstances indicate that their carrying value may not be recoverable, we assess these assets for impairment. There was no such impairment as of June 30, 2024 and December 31, 2023. U.S. Treasury Securities Investments As of June 30, 2024 and December 31, 2023, the Company had $24,651 and $115,914, respectively, of investments in U.S. Treasury bills which were classified as held to maturity and carried at amortized cost. These investments are included in short-term investments in the condensed consolidated balance sheets as the original maturities are greater than three months and less than twelve months. The Company has the intent and ability to hold these securities to maturity and gross unrecognized losses were $0. As of June 30, 2024 and December 31, 2023, the Company had $18,602 and $22,232, respectively, of investments in U.S. Treasury bill money market funds with an original maturity of less than three months. These investments are considered cash equivalents and are included in cash and cash equivalents in the condensed consolidated balances sheets. Restricted Investments Restricted investments are composed of investments in U.S. Treasury bills and certificates of deposits and are included within other assets in the condensed consolidated balance sheets. As of June 30, 2024 and December 31, 2023, the Company had $1,375 and $1,423 of restricted investments in U.S. Treasury bills and $2,336 and $1,755 of restricted investments in certificates of deposits, respectively. The Company has the intent and ability to hold these investments until maturity; therefore, these investments are stated at amortized cost. Restricted investments are required to be maintained at a financial institution within certain states. As of June 30, 2024 and December 31, 2023, these investments had maturities with less than 12 months. Due to the nature of the state's requirements, these assets are classified as noncurrent assets regardless of the contractual maturity date.
|
| X |
- References
+ Details
| Name: |
us-gaap_FairValueDisclosuresAbstract |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:stringItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionThe entire disclosure for the fair value of financial instruments (as defined), including financial assets and financial liabilities (collectively, as defined), and the measurements of those instruments as well as disclosures related to the fair value of non-financial assets and liabilities. Such disclosures about the financial instruments, assets, and liabilities would include: (1) the fair value of the required items together with their carrying amounts (as appropriate); (2) for items for which it is not practicable to estimate fair value, disclosure would include: (a) information pertinent to estimating fair value (including, carrying amount, effective interest rate, and maturity, and (b) the reasons why it is not practicable to estimate fair value; (3) significant concentrations of credit risk including: (a) information about the activity, region, or economic characteristics identifying a concentration, (b) the maximum amount of loss the entity is exposed to based on the gross fair value of the related item, (c) policy for requiring collateral or other security and information as to accessing such collateral or security, and (d) the nature and brief description of such collateral or security; (4) quantitative information about market risks and how such risks are managed; (5) for items measured on both a recurring and nonrecurring basis information regarding the inputs used to develop the fair value measurement; and (6) for items presented in the financial statement for which fair value measurement is elected: (a) information necessary to understand the reasons for the election, (b) discussion of the effect of fair value changes on earnings, (c) a description of [similar groups] items for which the election is made and the relation thereof to the balance sheet, the aggregate carrying value of items included in the balance sheet that are not eligible for the election; (7) all other required (as defined) and desired information. Reference 1: http://www.xbrl.org/2003/role/exampleRef
-Topic 820
-SubTopic 10
-Name Accounting Standards Codification
-Section 55
-Paragraph 107
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482078/820-10-55-107
Reference 2: http://www.xbrl.org/2003/role/exampleRef
-Topic 820
-SubTopic 10
-Name Accounting Standards Codification
-Section 55
-Paragraph 100
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482078/820-10-55-100
Reference 3: http://www.xbrl.org/2003/role/disclosureRef
-Topic 820
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 2
-Subparagraph (c)(3)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482106/820-10-50-2
Reference 4: http://www.xbrl.org/2003/role/disclosureRef
-Topic 820
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 6A
-Subparagraph (a)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482106/820-10-50-6A
Reference 5: http://www.xbrl.org/2003/role/disclosureRef
-Topic 820
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 2E
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482106/820-10-50-2E
Reference 6: http://www.xbrl.org/2003/role/disclosureRef
-Topic 820
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 6A
-Subparagraph (h)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482106/820-10-50-6A
Reference 7: http://www.xbrl.org/2003/role/disclosureRef
-Topic 820
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 6A
-Subparagraph (f)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482106/820-10-50-6A
Reference 8: http://www.xbrl.org/2003/role/disclosureRef
-Topic 820
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 6A
-Subparagraph (e)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482106/820-10-50-6A
Reference 9: http://www.xbrl.org/2003/role/disclosureRef
-Topic 820
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 6A
-Subparagraph (d)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482106/820-10-50-6A
Reference 10: http://www.xbrl.org/2003/role/disclosureRef
-Topic 820
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 2
-Subparagraph (h)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482106/820-10-50-2
Reference 11: http://www.xbrl.org/2003/role/disclosureRef
-Topic 820
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 2
-Subparagraph (g)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482106/820-10-50-2
Reference 12: http://www.xbrl.org/2003/role/disclosureRef
-Topic 940
-SubTopic 820
-Name Accounting Standards Codification
-Section 50
-Paragraph 1
-Subparagraph (a)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147478119/940-820-50-1
| Name: |
us-gaap_FairValueDisclosuresTextBlock |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
dtr-types:textBlockItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
v3.24.2.u1
Accounts Receivable
|
6 Months Ended |
Jun. 30, 2024 |
|---|
| Accounts Receivable, after Allowance for Credit Loss [Abstract] |
|
| Accounts Receivable |
Accounts Receivable Accounts receivable consisted of the following as of June 30, 2024 and December 31, 2023: | | | | | | | | | | | | | | June 30,
2024 | | December 31,
2023 | | Government receivables | $ | 78,529 | | | $ | 35,529 | | | Pharmacy rebate receivables | 94,695 | | | 75,894 | | | Other receivables | 10,085 | | | 8,326 | | | Total accounts receivable | 183,309 | | | 119,749 | | | Allowance for credit losses | (95) | | | — | | | Accounts receivable, net | $ | 183,214 | | | $ | 119,749 | |
The allowance for expected credit losses for accounts receivable is based primarily on past collections experience relative to the length of time receivables are past due. However, when available evidence reasonably supports an assumption that future economic conditions will differ from current and historical payment collections, an adjustment is reflected in the allowance for expected credit losses. We record pharmacy rebates and other receivables based on contractual terms and expected collections and our estimation process for contractual allowances for such balances generally results in an allowance for balances outstanding greater than 90 days or if expected credit risks are known. Receivables and any associated allowance are written off only when all collection attempts have failed and such amounts are determined unrecoverable. We regularly review the adequacy of these allowances based on a variety of factors, including age of the outstanding receivable and collection history. When circumstances related to specific collection patterns change, estimates of the recoverability of receivables are adjusted. Because substantially all of our receivable amounts are readily determinable and a large portion of our creditors are governmental authorities, our allowance for credit losses is insignificant. We recorded a credit loss related to accounts receivable of $95 and $50 during the three months ended June 30, 2024 and 2023, respectively, and $95 and $51 during the six months ended June 30, 2024 and 2023. The amounts were recorded in selling general, and administrative expenses in the condensed consolidated statements of operations.
|
| X |
- References
+ Details
| Name: |
us-gaap_AccountsReceivableNetAbstract |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:stringItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionThe entire disclosure for claims held for amounts due to entity, excluding financing receivables. Examples include, but are not limited to, trade accounts receivables, notes receivables, loans receivables. Includes disclosure for allowance for credit losses. Reference 1: http://www.xbrl.org/2009/role/commonPracticeRef
-Topic 310
-SubTopic 10
-Name Accounting Standards Codification
-Publisher FASB
-URI https://asc.fasb.org/310-10/tableOfContent
Reference 2: http://www.xbrl.org/2003/role/disclosureRef
-Topic 835
-SubTopic 30
-Name Accounting Standards Codification
-Section 45
-Paragraph 2
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482925/835-30-45-2
| Name: |
us-gaap_LoansNotesTradeAndOtherReceivablesDisclosureTextBlock |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
dtr-types:textBlockItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
v3.24.2.u1
Property and Equipment
|
6 Months Ended |
Jun. 30, 2024 |
|---|
| Property, Plant and Equipment [Abstract] |
|
| Property and Equipment |
Property and Equipment Property and equipment consisted of the following as of June 30, 2024 and December 31, 2023: | | | | | | | | | | | | | June 30,
2024 | | December 31,
2023 | | Computers and equipment | $ | 12,235 | | | $ | 11,447 | | | Office equipment and furniture | 4,397 | | | 4,396 | | | Software | 165,697 | | | 148,864 | | | Leasehold improvements | 6,347 | | | 6,347 | | | Construction in progress | 9,887 | | | 4,532 | | | Subtotal | 198,563 | | | 175,586 | | | Less accumulated depreciation | (136,133) | | | (123,685) | | | Property and equipment-net | $ | 62,430 | | | $ | 51,901 | |
Depreciation expense for the three months ended June 30, 2024 and 2023 was $6,516 and $5,190, respectively, of which $46 and $69, respectively, were included in medical expenses. Depreciation expense for the six months ended June 30, 2024 and 2023 was $12,517 and $10,075, respectively, of which $98 and $130, respectively, were included in medical expenses.
|
| X |
- References
+ Details
| Name: |
us-gaap_PropertyPlantAndEquipmentAbstract |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:stringItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionThe entire disclosure for long-lived, physical asset used in normal conduct of business and not intended for resale. Includes, but is not limited to, work of art, historical treasure, and similar asset classified as collections. Reference 1: http://fasb.org/us-gaap/role/ref/legacyRef
-Topic 360
-Name Accounting Standards Codification
-Publisher FASB
-URI https://asc.fasb.org/360/tableOfContent
Reference 2: http://www.xbrl.org/2003/role/disclosureRef
-Name Accounting Standards Codification
-Section 50
-Paragraph 6
-SubTopic 360
-Topic 958
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147477798/958-360-50-6
Reference 3: http://www.xbrl.org/2003/role/disclosureRef
-Name Accounting Standards Codification
-Section 50
-Paragraph 1
-Subparagraph (d)
-SubTopic 360
-Topic 958
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147477798/958-360-50-1
Reference 4: http://www.xbrl.org/2003/role/disclosureRef
-Name Accounting Standards Codification
-Section 50
-Paragraph 7
-SubTopic 360
-Topic 958
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147477798/958-360-50-7
| Name: |
us-gaap_PropertyPlantAndEquipmentDisclosureTextBlock |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
dtr-types:textBlockItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
v3.24.2.u1
Goodwill and Intangible Assets
|
6 Months Ended |
Jun. 30, 2024 |
|---|
| Goodwill and Intangible Assets Disclosure [Abstract] |
|
| Goodwill and Intangible Assets |
Goodwill and Intangible Assets Intangible assets consisted of the following as of June 30, 2024 and December 31, 2023: | | | | | | | | | | | | | | | | | | | | | | | | | June 30, 2024 | | Gross Carrying Value | | Accumulated Amortization | | Net Carrying Value | | Weighted Average Life | | Goodwill | $ | 34,826 | | | $ | — | | | $ | 34,826 | | | — | | License (indefinite lived) | 4,967 | | | — | | | 4,967 | | | — | | Plan member relationships | 2,700 | | | (2,700) | | | — | | | 9 years | | Other | 1,050 | | | (816) | | | 234 | | | 2 - 10 years | | Total | $ | 43,543 | | | $ | (3,516) | | | $ | 40,027 | | | |
| | | | | | | | | | | | | | | | | | | | | | | | | December 31, 2023 | | Gross Carrying Value | | Accumulated Amortization | | Net Carrying Value | | Weighted Average Life | | Goodwill | $ | 34,826 | | | $ | — | | | $ | 34,826 | | | — | | License (indefinite lived) | 4,967 | | | — | | | 4,967 | | | — | | Plan member relationships | 2,700 | | | (2,700) | | | — | | | 9 years | | Other | 1,050 | | | (765) | | | 285 | | | 2 - 10 years | | Total | $ | 43,543 | | | $ | (3,465) | | | $ | 40,078 | | | |
Amortization expense relating to intangible assets for the three months ended June 30, 2024 and 2023, was $23 and $74, respectively. Amortization expense relating to intangible assets for the six months ended June 30, 2024 and 2023, $51 and $171, respectively. Estimated amortization expense relating to intangible assets for each of the next five years ending December 31, is as follows: | | | | | | | Remainder of 2024 | $ | 31 | | | 2025 | 60 | | | 2026 | 60 | | | 2027 | 60 | | | 2028 | 23 | | | | | $ | 234 | |
There were no impairment charges related to goodwill and intangible assets for the three and six months ended June 30, 2024 and 2023.
|
| X |
- References
+ Details
| Name: |
us-gaap_GoodwillAndIntangibleAssetsDisclosureAbstract |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:stringItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionThe entire disclosure for goodwill and intangible assets. Reference 1: http://www.xbrl.org/2009/role/commonPracticeRef
-Topic 350
-SubTopic 30
-Name Accounting Standards Codification
-Publisher FASB
-URI https://asc.fasb.org/350-30/tableOfContent
Reference 2: http://www.xbrl.org/2009/role/commonPracticeRef
-Topic 350
-SubTopic 20
-Name Accounting Standards Codification
-Publisher FASB
-URI https://asc.fasb.org/350-20/tableOfContent
| Name: |
us-gaap_GoodwillAndIntangibleAssetsDisclosureTextBlock |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
dtr-types:textBlockItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
v3.24.2.u1
Medical Expenses Payable
|
6 Months Ended |
Jun. 30, 2024 |
|---|
| Insurance [Abstract] |
|
| Medical Expenses Payable |
Medical Expenses Payable The following table is a detail of medical expenses payable as of June 30, 2024 and December 31, 2023: | | | | | | | | | | | | | | June 30,
2024 | | December 31,
2023 | | Claims incurred but not paid | $ | 156,379 | | | $ | 95,664 | | | Capitation and risk-sharing payable | 69,316 | | | 50,894 | | | Other | 89,674 | | | 58,841 | | | Medical expenses payable | $ | 315,369 | | | $ | 205,399 | |
Each period, we re-examine previously established outstanding claims reserve estimates based on actual claims submissions and other changes in facts and circumstances. As more complete claim information becomes available, we adjust the amount of the estimates and include the changes in estimates in claim costs in the period in which the change is identified. Substantially, all of the total claims paid by us are known and settled within the first year from the date of service, and substantially, all remaining claim amounts are paid within a three-year period. The following table presents components of the change in medical expenses payable as of June 30, 2024 and 2023: | | | | | | | | | | | | | June 30,
2024 | | June 30,
2023 | | Claims incurred but not paid - beginning balance | $ | 95,664 | | | $ | 88,813 | | | Incurred related to: | | | | | Current year | 407,156 | | | 235,027 | | | Prior years | (7,257) | | | (7,168) | | | Total incurred, net of reinsurance | 399,899 | | | 227,859 | | | Payments related to: | | | | | Current year | 263,824 | | | 156,152 | | | Prior years | 75,360 | | | 68,632 | | | Total payments, net of reinsurance | 339,184 | | | 224,784 | | | Claims incurred but not paid - ending balance | 156,379 | | | 91,888 | | | Capitation payable, risk-sharing payable, and other | 158,990 | | | 115,310 | | | Total medical expenses payable | $ | 315,369 | | | $ | 207,198 | |
|
| X |
- References
+ Details
| Name: |
us-gaap_InsuranceAbstract |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:stringItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionThe entire disclosure for insurance products considered to be short-duration contracts because the contract provides insurance protection for a fixed period of short duration and enables the insurer to cancel the contract or to adjust the provisions of the contract at the end of any contract period, such as adjusting the amount of premiums charged or coverage provided, and on contracts on which amounts are paid but insurance risk is not transferred. Reference 1: http://www.xbrl.org/2003/role/disclosureRef
-Topic 944
-SubTopic 40
-Name Accounting Standards Codification
-Section 50
-Paragraph 4D
-Subparagraph (b)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480081/944-40-50-4D
Reference 2: http://fasb.org/us-gaap/role/ref/legacyRef
-Topic 944
-Name Accounting Standards Codification
-Publisher FASB
-URI https://asc.fasb.org/944/tableOfContent
| Name: |
us-gaap_ShortDurationInsuranceAndDepositContractsTextBlock |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
dtr-types:textBlockItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
v3.24.2.u1
Long-Term Debt
|
6 Months Ended |
Jun. 30, 2024 |
|---|
| Debt Disclosure [Abstract] |
|
| Long-Term Debt |
Long-Term Debt Long-term debt is recorded at carrying value in the condensed consolidated balance sheets. The carrying value of long-term debt outstanding, net of unamortized debt issuance costs, consisted of the following as of June 30, 2024 and December 31, 2023: | | | | | | | | | | | | | June 30,
2024 | | December 31,
2023 | | Long-term debt | $ | 215,000 | | | $ | 165,000 | | | Less unamortized debt issuance costs | (3,258) | | | (3,187) | | | Long-term debt-net of amortization | 211,742 | | | 161,813 | | | Less current portion of long-term debt | — | | | — | | | Long-term debt - net of current portion | $ | 211,742 | | | $ | 161,813 | |
Oxford Term Loan On September 2, 2022 (the "Effective Date"), Alignment Healthcare USA, LLC entered into a senior secured term loan agreement (the “Oxford Loan Agreement”) with Oxford Finance LLC (“Oxford”), as administrative agent, collateral agent and a lender, and the other lenders from time to time party thereto (collectively, the “Lenders”), pursuant to which the Lenders have agreed to lend an aggregate principal amount of up to $250,000 in a series of term loans (the “Term Loans”). Pursuant to the Oxford Loan Agreement, we received an initial Term Loan of $165,000 on the Effective Date and had the option to borrow up to an additional $85,000 of Term Loans (such additional Term Loans, the “Delayed Draw Term Loans”). On June 14, 2024, we borrowed $50,000 in aggregate principal amount of the Delayed Draw Term Loans prior to the expiration date for such amount of the Delayed Draw Term Loans of June 30, 2024. As of June 30, 2024 we have the option to borrow an additional $35,000 in undrawn Delayed Draw Term Loans, which expires on September 1, 2025.
Interest on the Term Loans is a variable rate equal to (i) the secured overnight financing rate ("SOFR") administered by the Federal Reserve Bank of New York for a one-month tenor, subject to a floor of 1.00%, plus (ii) an applicable margin of 6.50%. All unpaid principal and accrued and unpaid interest with respect to each Term Loan is due and payable in full on September 1, 2027. The interest rate applied during the six months ended June 30, 2024 ranged from 11.82% to 11.85%. The initial Term Loan was subject to a commitment fee of $1,650 and an origination fee of $1,650. The Delayed Draw Term Loans are subject to a commitment fee of $850. We incurred additional debt issuance costs of $1,096 related to attorney fees and other third-party costs. We also incurred an origination fee of $500 related to the $50,000 draw down of the Delayed Draw Term Loans. The commitment and origination fees are included within debt issuance costs and were deferred and will be amortized to interest expense over the debt term using the straight line method, which is materially consistent with the effective interest method. The debt issuance costs related to the initial Term Loan are presented in the condensed consolidated balance sheet as a direct deduction from the carrying value of the term loan. The debt issuance costs related to the Delayed Draw Term Loan are presented in the condensed consolidated balance sheet as other assets. The Term Loans are jointly and severally guaranteed by Alignment Healthcare, Inc. and certain of our wholly owned subsidiaries and collateralized by all unrestricted assets. For certain prepayments of the Term Loans prior to the second anniversary of the Effective Date, we will be required to pay a prepayment fee of 1.00% of the principal amount of the Term Loans being prepaid. The Oxford Loan Agreement includes customary events of default, including, among others, payment defaults, breach of representations and warranties, covenant defaults, judgment defaults, insolvency and bankruptcy defaults, and change of control. The occurrence of an event of default could result in the acceleration of the obligations under the Oxford Loan Agreement, termination of the Term Loan commitments and the right to foreclose on the collateral securing the obligations. During the existence of an event of default, the outstanding Term Loans will accrue interest at a rate per annum equal to 2.00% plus the otherwise applicable interest rate. Additionally, in the event of any contemplated asset sale or series of asset sales yielding net proceeds in excess of $2,500, except those excluded per the Oxford Loan Agreement, we are required to prepay the aggregate outstanding principal balance of the Term Loans in an amount equal to the entire amount of the asset sale net proceeds, plus any accrued and unpaid interest. The Oxford Loan Agreement includes financial covenants that require the Borrower Parties to (i) maintain minimum liquidity, as defined in the Loan Agreement, of $23,000 and (ii) satisfy a maximum permitted ratio of debt to trailing twelve-month revenue, as set forth in the Loan Agreement. As of June 30, 2024 and December 31, 2023, we were in compliance with the Oxford financial covenants. Future maturities under the term loan for each of the next five years ending December 31, are as follows: | | | | | | | Amount | | Remainder of 2024 | $ | — | | | 2025 | 2,150 | | | 2026 | 2,150 | | | 2027 | 210,700 | | | 2028 | — | | | $ | 215,000 | |
|
| X |
- References
+ Details
| Name: |
us-gaap_DebtDisclosureAbstract |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:stringItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionThe entire disclosure for long-term debt. Reference 1: http://fasb.org/us-gaap/role/ref/legacyRef
-Topic 470
-Name Accounting Standards Codification
-Publisher FASB
-URI https://asc.fasb.org/470/tableOfContent
| Name: |
us-gaap_LongTermDebtTextBlock |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
dtr-types:textBlockItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
v3.24.2.u1
Income Taxes
|
6 Months Ended |
Jun. 30, 2024 |
|---|
| Income Tax Disclosure [Abstract] |
|
| Income Taxes |
Income Taxes For the three and six months ended June 30, 2024, we recorded income tax expense of $22 and $22, respectively. For the three and six months ended June 30, 2023, we recorded income tax expense of $1 and $2, respectively. The increase in tax for the three and six months ended June 30, 2024 when compared to the three and six months ended June 30, 2023, is primarily attributable to an increase in state taxes. Our future effective tax rate may vary from the statutory tax rate primarily due to changes in our valuation allowance, state taxes, and excess executive compensation. We have federal and state cumulative net operating losses ("NOLs") as of June 30, 2024 and December 31, 2023. Given the history of losses, and after consideration for the risk associated with estimates of future taxable income, we established a full valuation allowance against net deferred tax assets at June 30, 2024 and 2023. Under the Tax Cuts and Jobs Act (“TCJA”), federal NOLs generated after 2017 will be carried forward indefinitely but are limited to an 80% deduction of taxable income. NOLs generated prior to 2018 have a 20-year carryforward period and can be used to offset 100% of taxable income. An exception to the TCJA federal NOL rule applies to certain of our subsidiaries and requires all NOLs generated from those entities to have a 20-year carryforward period and offset 100% of taxable income. For the year ended December 31, 2023 federal and state NOL carryforwards were $504,097 and $498,933, respectively. $312,446 of the total federal net operating loss carryforwards have an indefinite life while the remaining federal and state net operating loss carryforwards begin to expire in 2033 if not utilized. On June 27, 2024, California Senate Bill 167 (“SB 167”) was enacted into law, suspending California NOL utilization for taxpayers with more than $1 million of taxable income, effective for tax years 2024, 2025, and 2026. SB 167 includes an extended carryover period for the suspended NOLs with an additional year carryforward for each year of suspension. The Company will continue to monitor this legislation and its impact on our deferred tax assets. An “ownership change” as defined under Section 382 of the Internal Revenue Code ("IRC"), could potentially limit the ability to utilize certain tax attributes including the Company’s substantial NOLs. Ownership change is generally defined as any significant change in ownership of more than 50% of its stock over a three-year testing period. If, as a result of current or future transactions involving our common stock, we undergo cumulative ownership changes which exceed 50% over a testing period, our ability to utilize our NOL carryforwards would be subject to additional limitations under IRC Section 382. We continue to monitor changes in ownership with respect to these income tax provisions.
|
| X |
- DefinitionThe entire disclosure for income tax. Reference 1: http://www.xbrl.org/2003/role/disclosureRef
-Topic 740
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 12
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482685/740-10-50-12
Reference 2: http://www.xbrl.org/2003/role/exampleRef
-Topic 740
-SubTopic 10
-Name Accounting Standards Codification
-Section 55
-Paragraph 231
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482663/740-10-55-231
Reference 3: http://www.xbrl.org/2003/role/disclosureRef
-Topic 740
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 12C
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482685/740-10-50-12C
Reference 4: http://www.xbrl.org/2003/role/disclosureRef
-Topic 740
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 12B
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482685/740-10-50-12B
Reference 5: http://www.xbrl.org/2003/role/disclosureRef
-Topic 740
-SubTopic 270
-Name Accounting Standards Codification
-Section 50
-Paragraph 1
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147477891/740-270-50-1
Reference 6: http://www.xbrl.org/2003/role/disclosureRef
-Topic 740
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SAB Topic 6.I.5.Q1)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147479360/740-10-S99-1
Reference 7: http://www.xbrl.org/2003/role/disclosureRef
-Topic 946
-SubTopic 20
-Name Accounting Standards Codification
-Section 50
-Paragraph 13
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480990/946-20-50-13
Reference 8: http://www.xbrl.org/2003/role/disclosureRef
-Topic 235
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.4-08(h)(2))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480678/235-10-S99-1
Reference 9: http://www.xbrl.org/2003/role/disclosureRef
-Topic 740
-Name Accounting Standards Codification
-Publisher FASB
-URI https://asc.fasb.org/740/tableOfContent
Reference 10: http://www.xbrl.org/2003/role/disclosureRef
-Topic 740
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 14
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482685/740-10-50-14
Reference 11: http://www.xbrl.org/2003/role/disclosureRef
-Topic 740
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 21
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482685/740-10-50-21
Reference 12: http://www.xbrl.org/2003/role/disclosureRef
-Topic 740
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 17
-Subparagraph (b)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482685/740-10-50-17
Reference 13: http://www.xbrl.org/2003/role/disclosureRef
-Topic 740
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 2
-Subparagraph (SAB Topic 11.C)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147479360/740-10-S99-2
Reference 14: http://www.xbrl.org/2003/role/disclosureRef
-Topic 740
-SubTopic 30
-Name Accounting Standards Codification
-Section 50
-Paragraph 2
-Subparagraph (a)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482603/740-30-50-2
| Name: |
us-gaap_IncomeTaxDisclosureTextBlock |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
dtr-types:textBlockItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
v3.24.2.u1
Equity-Based Compensation
|
6 Months Ended |
Jun. 30, 2024 |
|---|
| Share-Based Payment Arrangement [Abstract] |
|
| Equity-Based Compensation |
Equity-Based Compensation Equity Awards Stock Options Our outstanding stock options generally vest 25% annually over four years and generally expire 10 years from the date of the grant. The 2021 Equity Incentive Plan provides that stock option grants will be made with an exercise price at no less than the estimated fair value of common stock at the date of the grant. The following is a summary of the stock option transactions as of and for the three and six months ended June 30, 2024: | | | | | | | | | | | | | | | | | | | | | | | | | | Stock Options Outstanding | | (amounts in thousands, except shares and per share amount) | Shares Subject to Options Outstanding | | Weighted- Average Exercise Price per Option | | Weighted- Average Remaining Contractual Terms (in years) | | Aggregate Intrinsic Value | | Balances as of December 31, 2023 | 9,135,879 | | $ | 16.95 | | | 7.29 | | $ | 79 | | | Options granted | — | | — | | | | | | | Options exercised | — | | — | | | | | | | Options forfeited / expired | (112,536) | | 15.41 | | | | | | | Balances as of March 31, 2024 | 9,023,343 | | $ | 16.97 | | | 7.04 | | — | | | Options granted | — | | — | | | | | | | Options exercised | — | | — | | | | | | | Options forfeited / expired | (73,754) | | 16.62 | | | | | | | Balances as of June 30, 2024 | 8,949,589 | | $ | 16.97 | | | 6.79 | | $ | 27 | | | Vested and Exercisable as of June 30, 2024 | 6,297,452 | | $ | 17.28 | | | 6.75 | | $ | 14 | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | |
Aggregate intrinsic value represents the difference between the exercise price of the option and the closing price of our common stock. For the three and six months ended June 30, 2024 and 2023, no options were exercised. No options were granted during the three and six months ended June 30, 2024. Restricted Stock Awards Our outstanding Restricted Stock Awards ("RSA") generally vest 25% annually over four years. RSAs converted from pre-IPO awards generally vest on the later of the fourth anniversary of the original vesting commencement date or 50% annually on the first and second anniversary of the IPO. The following is a summary of RSA transactions for the three and six months ended June 30, 2024: | | | | | | | | | | | | | | Restricted Shares | | Weighted-Average Grant Date Fair Value | | Unvested and outstanding as of December 31, 2023 | 683,953 | | $ | 5.86 | | | Vested | (140,856) | | 13.22 | | | Forfeited | (2,799) | | 5.05 | | | Unvested and outstanding as of March 31, 2024 | 540,298 | | $ | 3.94 | | | Vested | (3,056) | | 2.49 | | | Forfeited | — | | — | | | Unvested and outstanding as of June 30, 2024 | 537,242 | | $ | 3.95 | | | | | | | | | | | | | |
Restricted Stock Units Our outstanding Restricted Stock Units ("RSU") generally vest 25% annually over four years. The following is a summary of RSU transactions as of and for the three and six months ended June 30, 2024: | | | | | | | | | | | | | | Restricted Stock Units | | Weighted-Average Grant Date Fair Value | | Unvested and outstanding as of December 31, 2023 | 10,541,625 | | $ | 11.25 | | | Granted | 6,517,337 | | 5.05 | Vested(1) | (2,385,493) | | 8.25 | | Cancelled/forfeited | (282,972) | | 9.36 | | Unvested and outstanding as of March 31, 2024 | 14,390,497 | | $ | 8.97 | | | Granted | 103,292 | | 5.62 | | Vested | (80,178) | | 6.07 | | Cancelled/forfeited | (395,338) | | 8.40 | | Unvested and outstanding as of June 30, 2024 | 14,018,273 | | $ | 8.98 | | | | | | | | | | | | | | | | | |
(1) Includes 107,948 shares that vested, but the issuance and delivery of the shares was deferred. Performance-based Restricted Stock Units ("PSUs") On September 14, 2023, the Board of Directors of the Company approved the grant of performance-based restricted stock units under the Company's 2021 Equity Incentive Plan to its executive management team and other key employees. Each grantee is eligible to vest in a number of PSUs ranging from 0% to 150% of the target number of PSUs granted, based on the aggregated achievement by the Company of certain performance metrics during the performance period beginning on January 1, 2024 and ending on December 31, 2024. The achievement of PSUs relative to the approved target is based on the following performance metrics and relative weighting: Health Plan Revenue Growth Percentage 60%, At-Risk Returning Member Medical Benefit Ratio 20% and Adjusted EBITDA, less Capital Expenditures 20%. 50% of the total number of earned PSUs will become vested upon certification of achievement of the performance metrics by the Compensation Committee on or about March 1, 2025 and the remaining 50% of earned PSUs will be become vested as of December 31, 2025, subject to continued service to the Company through such dates. On March 13, 2024, the Compensation Committee of the Board of Directors of the Company approved additional grants of PSUs under the Company's 2021 Equity Incentive Plan. Each grantee is eligible to vest in a number of PSUs ranging from 0% to 200% of the target number of PSUs granted, based on the aggregated achievement by the Company of certain performance metrics during the performance period beginning on January 1, 2024 and ending on December 31, 2026. The achievement of PSUs relative to the approved target is based on the following performance metrics and relative weighting: Revenue 50% and Adjusted EBITDA 50%. 100% of the total number of earned PSUs will become vested upon certification of achievement of the performance metrics by the Compensation Committee on or about March 1, 2027, subject to continued service to the Company through such date. The following is a summary of PSU transactions for the three and six months ended June 30, 2024: | | | | | | | | | | | | | | Performance-based restricted stock units | | Weighted-Average Grant Date Fair Value | | Unvested and outstanding as of December 31, 2023 | 7,233,205 | | $ | 5.74 | | | Granted | 1,160,000 | | 5.00 | | | Vested | — | | — | | | Cancelled/forfeited | (16,667) | | 5.74 | | | Unvested and outstanding as of March 31, 2024 | 8,376,538 | | $ | 5.64 | | | Granted | — | | — | | | Vested | — | | — | | | Cancelled/forfeited | (198,333) | | 5.67 | | | Unvested and outstanding as of June 30, 2024 | 8,178,205 | | $ | 5.64 | |
Equity-Based Compensation Expense Total equity-based compensation expense was presented on the statement of operations as follows: | | | | | | | | | | | | | | | | | | | | | | | | | | Three Months Ended June 30, | | Six Months Ended June 30, | | (amounts in thousands) | 2024 | | 2023 | | 2024 | | 2023 | | Selling, general and administrative expenses | $ | 16,022 | | | $ | 13,869 | | | $ | 35,743 | | | $ | 33,323 | | | Medical expenses | 762 | | | 1,767 | | | 1,895 | | | 4,291 | | | Total equity-based compensation expense | $ | 16,784 | | | $ | 15,636 | | | $ | 37,638 | | | $ | 37,614 | |
As of June 30, 2024, there was $93,667 in unrecognized compensation expense related to all non-vested awards (RSAs, options, RSUs and PSUs) that will be recognized over the weighted-average period of 1.70 years.
|
| X |
- DefinitionThe entire disclosure for share-based payment arrangement. Reference 1: http://www.xbrl.org/2003/role/exampleRef
-Topic 718
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 2
-Subparagraph (a)(1)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480429/718-10-50-2
Reference 2: http://www.xbrl.org/2003/role/disclosureRef
-Topic 718
-Name Accounting Standards Codification
-Publisher FASB
-URI https://asc.fasb.org/718/tableOfContent
Reference 3: http://www.xbrl.org/2003/role/disclosureRef
-Topic 718
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 2
-Subparagraph (a)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480429/718-10-50-2
Reference 4: http://www.xbrl.org/2003/role/disclosureRef
-Topic 718
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 2
-Subparagraph (h)(2)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480429/718-10-50-2
Reference 5: http://www.xbrl.org/2003/role/disclosureRef
-Topic 718
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 2
-Subparagraph (h)(2)(i)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480429/718-10-50-2
Reference 6: http://www.xbrl.org/2003/role/disclosureRef
-Topic 718
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 2
-Subparagraph (l)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480429/718-10-50-2
| Name: |
us-gaap_DisclosureOfCompensationRelatedCostsShareBasedPaymentsTextBlock |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
dtr-types:textBlockItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
v3.24.2.u1
Regulatory Requirements and Restricted Funds
|
6 Months Ended |
Jun. 30, 2024 |
|---|
| Regulated Operations [Abstract] |
|
| Regulatory Requirements and Restricted Funds |
Regulatory Requirements and Restricted Funds Our health plans or risk-bearing entities are required to maintain minimum capital requirements prescribed by various regulatory authorities in each of the states in which it operates. Risk-Based Capital Regulatory The National Association of Insurance Commissioners has adopted rules, which, if implemented by the states, set minimum capitalization requirements for insurance companies, health maintenance organizations ("HMOs"), and other entities bearing risk for health care coverage. The requirements take the form of risk-based capital (“RBC”) rules, which may vary from state to state. Certain states in which our health plans or risk bearing entities operate have adopted the RBC rules. Our health plans or risk-bearing entities were in compliance with the minimum capital requirements as of June 30, 2024. Tangible Net Equity Our health plan in California is required to comply with the tangible net equity (“TNE”) requirements. The required amount is the larger of: (1) $1,000; (2) 2% of the first $150,000 of annualized premium revenue, plus 1% of annualized premium revenue in excess of $150,000; or (3) 8% of the first $150,000 of annualized health care expenditures, except for those paid on a capitated or managed hospital payment basis, plus 4% of the annualized health care expenditures in excess of $150,000, except those paid on a capitated or managed hospital payment basis, plus 4% of annualized hospital expenditures paid on a managed hospital payment basis. We were in compliance with the TNE requirement as of June 30, 2024. We have the ability to provide additional capital to each of our health plans or risk-bearing entities when necessary to ensure that the RBC and TNE requirements are met. Certain states regulate the payment of dividends, loans, or other cash transfers from our regulated subsidiaries to our non-regulated subsidiaries and parent company. Such payments may require approval by state regulatory authorities and are limited based on certain financial criteria, such as the entity’s level of statutory income and statutory capital and surplus, or the entity’s level of tangible net equity or net worth, amongst other measures. These regulations vary by state. We were in compliance with the RBC and TNE requirements as of June 30, 2024. Restricted Assets Pursuant to the regulations governing our subsidiaries, we maintain certain deposits required by the government authorities in the form of cash, certificate of deposit and Treasury bills as protection in the event of insolvency. The use of funds from these investments is limited as required by regulation in the various states in which we operate, or as needed in the event of insolvency. Therefore, these deposits are reported within other assets on the condensed consolidated balance sheets. We hold these assets until maturity, at which time these assets will renew or are invested in a similar type of investment instrument. Given the regulatory requirements, we expect to hold these investments for long-term. As a result, we do not expect the value of these investments to decline significantly due to a sudden change in market interest rates. These investments are carried at amortized cost, which approximates fair value. See note 3, Fair Value, for further discussion.
|
| X |
- DefinitionRegulatory requirements And restricted funds text block.
| Name: |
alhc_RegulatoryRequirementsAndRestrictedFundsTextBlock |
| Namespace Prefix: |
alhc_ |
| Data Type: |
dtr-types:textBlockItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- References
+ Details
| Name: |
us-gaap_RegulatedOperationsAbstract |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:stringItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
v3.24.2.u1
Commitments and Contingencies
|
6 Months Ended |
Jun. 30, 2024 |
|---|
| Commitments and Contingencies Disclosure [Abstract] |
|
| Commitments and Contingencies |
Commitments and Contingencies Legal Proceedings We record a liability and accrue the costs for a loss when an unfavorable outcome is probable and the amount of the loss can be reasonably estimated. In some cases, no estimate of the possible loss or range of loss in excess of amounts accrued, if any, can be made because of the inherently unpredictable nature of legal and regulatory proceedings. While the liability and accrued costs reflect our best estimate, the actual amounts may materially be different. On April 27, 2022, a former employee of the Company filed a purported class action lawsuit (Dabney v. Alignment Healthcare USA, LLC, Orange County Superior Court) alleging that the Company failed to provide hourly employees with required meal and rest breaks or pay such workers a premium equal to an hour of pay for missed meal or rest breaks. Discovery in the matter commenced on June 8, 2022. On September 2, 2022, the court granted a stay of proceedings and discovery in anticipation of mediation scheduled for August 2023. On August 15, 2023, the Company entered into a tentative settlement of the action in consideration of an aggregate payment of $913. The settlement of this matter is subject to approval by the court which is expected in the third quarter of 2024. As a result of the tentative settlement, the Company has accrued for a potential liability of $913 as of June 30, 2024 and December 31, 2023 for this matter, which was recorded within accounts payable and accrued expenses on the consolidated balance sheet and selling, general and administrative expenses on the consolidated statement of operations. We may be involved in various litigation matters in the ordinary course of business. In the opinion of management, the ultimate resolution of legal proceedings is not expected to have a material adverse effect on the condensed consolidated financial statements. Amounts accrued for legal proceedings were not material as of June 30, 2024 and December 31, 2023.
|
| X |
- References
+ Details
| Name: |
us-gaap_CommitmentsAndContingenciesDisclosureAbstract |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:stringItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionThe entire disclosure for commitments and contingencies. Reference 1: http://www.xbrl.org/2009/role/commonPracticeRef
-Topic 405
-SubTopic 30
-Name Accounting Standards Codification
-Publisher FASB
-URI https://asc.fasb.org/405-30/tableOfContent
Reference 2: http://www.xbrl.org/2003/role/disclosureRef
-Topic 440
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 4
-Subparagraph (a)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482648/440-10-50-4
Reference 3: http://www.xbrl.org/2009/role/commonPracticeRef
-Topic 450
-Name Accounting Standards Codification
-Publisher FASB
-URI https://asc.fasb.org/450/tableOfContent
Reference 4: http://www.xbrl.org/2003/role/disclosureRef
-Topic 954
-SubTopic 440
-Name Accounting Standards Codification
-Section 50
-Paragraph 1
-Subparagraph (a)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147478522/954-440-50-1
Reference 5: http://www.xbrl.org/2003/role/disclosureRef
-Topic 440
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 4
-Subparagraph (c)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482648/440-10-50-4
Reference 6: http://fasb.org/us-gaap/role/ref/legacyRef
-Topic 440
-Name Accounting Standards Codification
-Publisher FASB
-URI https://asc.fasb.org/440/tableOfContent
| Name: |
us-gaap_CommitmentsAndContingenciesDisclosureTextBlock |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
dtr-types:textBlockItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
v3.24.2.u1
Pay vs Performance Disclosure - USD ($)
$ in Thousands |
3 Months Ended |
6 Months Ended |
Jun. 30, 2024 |
Jun. 30, 2023 |
Jun. 30, 2024 |
Jun. 30, 2023 |
| Pay vs Performance Disclosure |
|
|
|
|
| Net loss |
$ (24,010)
|
$ (28,477)
|
$ (70,531)
|
$ (65,761)
|
| X |
- ReferencesReference 1: http://www.xbrl.org/2003/role/presentationRef
-Publisher SEC
-Name Regulation S-K
-Number 229
-Section 402
-Subsection v
-Paragraph 1
| Name: |
ecd_PvpTable |
| Namespace Prefix: |
ecd_ |
| Data Type: |
xbrli:stringItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionThe portion of profit or loss for the period, net of income taxes, which is attributable to the parent. Reference 1: http://www.xbrl.org/2003/role/disclosureRef
-Topic 250
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 6
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147483443/250-10-50-6
Reference 2: http://www.xbrl.org/2003/role/disclosureRef
-Topic 250
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 9
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147483443/250-10-50-9
Reference 3: http://www.xbrl.org/2003/role/disclosureRef
-Topic 805
-SubTopic 60
-Name Accounting Standards Codification
-Section 65
-Paragraph 1
-Subparagraph (g)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147476176/805-60-65-1
Reference 4: http://www.xbrl.org/2003/role/disclosureRef
-Topic 740
-SubTopic 323
-Name Accounting Standards Codification
-Section 65
-Paragraph 2
-Subparagraph (g)(3)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147478666/740-323-65-2
Reference 5: http://fasb.org/us-gaap/role/ref/legacyRef
-Topic 220
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 2
-Subparagraph (SX 210.5-03(20))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147483621/220-10-S99-2
Reference 6: http://www.xbrl.org/2003/role/disclosureRef
-Topic 235
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.4-08(g)(1)(ii))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480678/235-10-S99-1
Reference 7: http://www.xbrl.org/2003/role/disclosureRef
-Topic 323
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 3
-Subparagraph (c)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147481687/323-10-50-3
Reference 8: http://www.xbrl.org/2003/role/disclosureRef
-Topic 825
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 28
-Subparagraph (f)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482907/825-10-50-28
Reference 9: http://www.xbrl.org/2003/role/disclosureRef
-Topic 220
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 6
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482765/220-10-50-6
Reference 10: http://www.xbrl.org/2003/role/disclosureRef
-Topic 250
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 3
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147483443/250-10-50-3
Reference 11: http://www.xbrl.org/2003/role/disclosureRef
-Topic 250
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 1
-Subparagraph (b)(2)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147483443/250-10-50-1
Reference 12: http://www.xbrl.org/2003/role/disclosureRef
-Topic 815
-SubTopic 40
-Name Accounting Standards Codification
-Section 65
-Paragraph 1
-Subparagraph (f)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480175/815-40-65-1
Reference 13: http://www.xbrl.org/2003/role/disclosureRef
-Topic 250
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 8
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147483443/250-10-50-8
Reference 14: http://www.xbrl.org/2003/role/disclosureRef
-Topic 250
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 11
-Subparagraph (a)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147483443/250-10-50-11
Reference 15: http://www.xbrl.org/2003/role/disclosureRef
-Topic 250
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 11
-Subparagraph (b)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147483443/250-10-50-11
Reference 16: http://www.xbrl.org/2003/role/disclosureRef
-Topic 250
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 4
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147483443/250-10-50-4
Reference 17: http://www.xbrl.org/2003/role/exampleRef
-Topic 946
-SubTopic 830
-Name Accounting Standards Codification
-Section 55
-Paragraph 10
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147479168/946-830-55-10
Reference 18: http://www.xbrl.org/2003/role/disclosureRef
-Topic 946
-SubTopic 220
-Name Accounting Standards Codification
-Section 45
-Paragraph 7
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147479105/946-220-45-7
Reference 19: http://www.xbrl.org/2003/role/disclosureRef
-Topic 944
-SubTopic 220
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.7-04(18))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147477250/944-220-S99-1
Reference 20: http://www.xbrl.org/2003/role/disclosureRef
-Topic 946
-SubTopic 220
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.6-07(9))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147479134/946-220-S99-1
Reference 21: http://www.xbrl.org/2003/role/disclosureRef
-Topic 946
-SubTopic 220
-Name Accounting Standards Codification
-Section S99
-Paragraph 3
-Subparagraph (SX 210.6-09(1)(d))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147479134/946-220-S99-3
Reference 22: http://www.xbrl.org/2003/role/disclosureRef
-Topic 470
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1A
-Subparagraph (SX 210.13-01(a)(4)(i))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480097/470-10-S99-1A
Reference 23: http://www.xbrl.org/2009/role/commonPracticeRef
-Topic 470
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1A
-Subparagraph (SX 210.13-01(a)(4)(ii))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480097/470-10-S99-1A
Reference 24: http://www.xbrl.org/2003/role/disclosureRef
-Topic 470
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1A
-Subparagraph (SX 210.13-01(a)(4)(iii)(A))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480097/470-10-S99-1A
Reference 25: http://www.xbrl.org/2003/role/disclosureRef
-Topic 470
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1A
-Subparagraph (SX 210.13-01(a)(4)(iv))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480097/470-10-S99-1A
Reference 26: http://www.xbrl.org/2003/role/disclosureRef
-Topic 470
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1A
-Subparagraph (SX 210.13-01(a)(5))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480097/470-10-S99-1A
Reference 27: http://www.xbrl.org/2003/role/disclosureRef
-Topic 470
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1B
-Subparagraph (SX 210.13-02(a)(4)(i))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480097/470-10-S99-1B
Reference 28: http://www.xbrl.org/2003/role/disclosureRef
-Topic 470
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1B
-Subparagraph (SX 210.13-02(a)(4)(iii)(A))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480097/470-10-S99-1B
Reference 29: http://www.xbrl.org/2003/role/disclosureRef
-Topic 470
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1B
-Subparagraph (SX 210.13-02(a)(4)(iii)(B))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480097/470-10-S99-1B
Reference 30: http://www.xbrl.org/2003/role/disclosureRef
-Topic 470
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1B
-Subparagraph (SX 210.13-02(a)(4)(iv))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480097/470-10-S99-1B
Reference 31: http://www.xbrl.org/2003/role/disclosureRef
-Topic 470
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1B
-Subparagraph (SX 210.13-02(a)(5))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480097/470-10-S99-1B
Reference 32: http://www.xbrl.org/2003/role/disclosureRef
-Topic 260
-SubTopic 10
-Name Accounting Standards Codification
-Section 45
-Paragraph 60B
-Subparagraph (a)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482689/260-10-45-60B
Reference 33: http://www.xbrl.org/2003/role/disclosureRef
-Topic 205
-SubTopic 20
-Name Accounting Standards Codification
-Section 50
-Paragraph 7
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147483499/205-20-50-7
Reference 34: http://fasb.org/us-gaap/role/ref/legacyRef
-Topic 230
-SubTopic 10
-Name Accounting Standards Codification
-Section 45
-Paragraph 28
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482740/230-10-45-28
Reference 35: http://www.xbrl.org/2003/role/disclosureRef
-Topic 220
-SubTopic 10
-Name Accounting Standards Codification
-Section 45
-Paragraph 1A
-Subparagraph (a)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482790/220-10-45-1A
Reference 36: http://www.xbrl.org/2003/role/disclosureRef
-Topic 220
-SubTopic 10
-Name Accounting Standards Codification
-Section 45
-Paragraph 1B
-Subparagraph (a)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482790/220-10-45-1B
Reference 37: http://fasb.org/us-gaap/role/ref/legacyRef
-Topic 942
-SubTopic 220
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.9-04(22))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147478524/942-220-S99-1
| Name: |
us-gaap_NetIncomeLoss |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:monetaryItemType |
| Balance Type: |
credit |
| Period Type: |
duration |
|
v3.24.2.u1
| X |
- ReferencesReference 1: http://www.xbrl.org/2003/role/presentationRef
-Publisher SEC
-Name Regulation S-K
-Number 229
-Section 408
-Subsection a
-Paragraph 1
| Name: |
ecd_NonRule10b51ArrAdoptedFlag |
| Namespace Prefix: |
ecd_ |
| Data Type: |
xbrli:booleanItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- ReferencesReference 1: http://www.xbrl.org/2003/role/presentationRef
-Publisher SEC
-Name Regulation S-K
-Number 229
-Section 408
-Subsection a
-Paragraph 1
| Name: |
ecd_NonRule10b51ArrTrmntdFlag |
| Namespace Prefix: |
ecd_ |
| Data Type: |
xbrli:booleanItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- ReferencesReference 1: http://www.xbrl.org/2003/role/presentationRef
-Publisher SEC
-Name Regulation S-K
-Number 229
-Section 408
-Subsection a
-Paragraph 1
| Name: |
ecd_Rule10b51ArrAdoptedFlag |
| Namespace Prefix: |
ecd_ |
| Data Type: |
xbrli:booleanItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- ReferencesReference 1: http://www.xbrl.org/2003/role/presentationRef
-Publisher SEC
-Name Regulation S-K
-Number 229
-Section 408
-Subsection a
-Paragraph 1
| Name: |
ecd_Rule10b51ArrTrmntdFlag |
| Namespace Prefix: |
ecd_ |
| Data Type: |
xbrli:booleanItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- ReferencesReference 1: http://www.xbrl.org/2003/role/presentationRef
-Publisher SEC
-Name Regulation S-K
-Number 229
-Section 408
-Subsection a
-Paragraph 2
-Subparagraph A
| Name: |
ecd_TradingArrByIndTable |
| Namespace Prefix: |
ecd_ |
| Data Type: |
xbrli:stringItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
v3.24.2.u1
Summary of Significant Accounting Policies (Policies)
|
6 Months Ended |
Jun. 30, 2024 |
|---|
| Accounting Policies [Abstract] |
|
| Basis of Presentation |
The accompanying condensed consolidated financial statements and accompanying notes have been prepared in accordance with accounting principles generally accepted in the United States of America (“U.S. GAAP”). The balance sheet as of December 31, 2023, included herein, was derived from audited financial statements, but does not include all disclosures required by GAAP. In accordance with the rules and regulations of the U.S. Securities and Exchange Commission ("SEC"), the Company has omitted certain footnote disclosures that would substantially duplicate the disclosures contained in its annual audited consolidated financial statements. Therefore, these condensed consolidated financial statements should be read in conjunction with the Company's Annual Report on Form 10-K for the year-ended December 31, 2023 as filed with the SEC. Furthermore, the condensed consolidated financial statements include the accounts of the Company, our subsidiaries, and three immaterial variable interest entities in which we are the primary beneficiary. All intercompany transactions have been eliminated in consolidation. Noncontrolling interest is presented within the equity section of the condensed consolidated balance sheets. We have no components of other comprehensive income (loss), and accordingly, comprehensive income (loss) is the same as the net income (loss) for all periods presented.
|
| Use of Estimates |
The preparation of the condensed consolidated financial statements requires management to make estimates and judgments that affect the amounts reported in the condensed consolidated financial statements. Our significant estimates include, but are not limited to, the determination of medical expenses payable; the impact of risk adjustment provisions related to our Medicare contracts; collectability of receivables; valuation of related impairment recognition of long-lived assets, including goodwill and intangible assets; equity-based compensation expense; and contingent liabilities. Estimates and judgments are based upon historical information and on various other assumptions that are believed to be reasonable under the circumstances. Actual results could differ materially from those estimates and the impact of any change in estimates is included in earnings in the period in which the estimate is adjusted.
|
| Segments |
We have determined that our chief executive officer is the chief operating decision maker (“CODM”) who regularly reviews financial operating results on a consolidated basis for purposes of allocating resources and evaluating financial performance. We operate and manage the business as one reportable segment and one operating segment, which is to provide healthcare services to our seniors. Factors used in determining the reportable segment include the nature of operating activities, our organizational and reporting structure, and the type of information reviewed by the CODM to allocate resources and evaluate financial performance. All of our assets are located in the United States.
|
| Fair Value Measurements |
Fair value is the price that would be received to sell an asset or paid to transfer a liability in an orderly transaction between market participants at the measurement date. Our current assets and current liabilities approximate fair value because of the short-term nature of these financial instruments. Financial instruments measured at fair value on a recurring basis were based upon a three-tier hierarchy as follows: Level 1 - Quoted prices in active markets for identical assets or liabilities Level 2 - Other inputs that are observable for the asset or liability, either directly or indirectly, for substantially the full term of the asset or liability Level 3 - Unobservable inputs that reflect management’s best estimate of what market participants would use in pricing the asset or liability at the measurement date The fair value of cash, cash equivalents, restricted cash and U.S. Treasury bills was determined based on Level 1 inputs. The fair value of certificate of deposits, which are recorded in other assets in the condensed consolidated balance sheets, was determined based on Level 2 inputs. There were no assets or liabilities measured at fair value using Level 3 inputs as of June 30, 2024 and December 31, 2023. Our long-term debt was reported at carrying value.
|
| Revenue and Accounts Receivable |
Premium revenue is derived monthly from the federal government based on our contracts with the Centers for Medicare and Medicaid Services (“CMS”). In accordance with these arrangements, we assume the responsibility for the outcomes and the economic risk of funding our members’ health care, supplemental benefits and related administration costs. We recognize premium revenue in the month that members are entitled to receive health care services, and premiums collected in advance are deferred. The monthly reimbursement includes a fixed payment per member per month (“PMPM”), which is adjusted based on certain risk factors derived from medical diagnoses and conditions of our members. The adjustments are estimated by projecting the ultimate annual premium and are recognized ratably during the year, with adjustments each period to reflect changes in the estimated ultimate premium. Premiums are also recorded net of estimated uncollectible amounts and retroactive membership adjustments. Capitation revenue consists primarily of capitated fees for medical care services provided by us under arrangements with third-party payors. In 2023, capitation revenue consisted primarily of revenue from CMS related to our participation in the CMS "ACO Realizing Equity, Access, and Community Health Model” or “ACO REACH” model, as discussed below. Under those arrangements with third-party payors, we receive a PMPM payment for a defined member population, and we are responsible for providing health care services to the member population over the contract period. We are solely responsible for the cost of health care services related to the member population and in some cases, we are financially responsible for the supplemental benefits provided by us to the members. We act as a principal in arranging for and controlling the services provided by our provider network and we are at risk for arranging and providing health care services. The premium and capitation payments we receive monthly from CMS for our members are determined from our annual bid or similarly from third-party payors under our capitation arrangement. These payments represent revenues for providing health care coverage, including Medicare Part D benefits. Under the Medicare Part D program, our members and the members of the third-party payors receive standard drug benefits. We may also provide enhanced benefits at our own expense. We recognize premium or capitation revenue for providing this insurance coverage in the month that members are entitled to receive health care services and any premium or capitation collected in advance is deferred. Our CMS payment related to Medicare Part D is subject to risk sharing through the Medicare Part D risk corridor provisions. We also participate in the CMS ACO REACH program, formerly the Direct Contracting Model ("DCE"). CMS serves as the claim adjudicator for institutional and specialists care, and directly pays for such fee for service claims. The ACO REACH entity ("ACO") is responsible for the cost of health care services related to the patient population attributed to the ACO by participating in 100% savings/losses via the risk share model and in some cases, are financially responsible for the supplemental benefits provided to the patients. In 2024, we entered into a management services and risk management agreement with a third-party healthcare company. The third party will be responsible for arranging and controlling the health care services provided to the ACO members, and for providing certain management and support services with respect to ACO operations. The third party will also assume specified upside and downside financial risk relative to the ACO’s performance. As a result of this arrangement, revenue is recorded on a net basis within other revenue on the condensed consolidated statement of operations for the three and six months ended June 30, 2024. Revenue recognized by the ACO for the three and six months ended June 30, 2024 was $(744) and $241, respectively. Prior to 2024, the ACO acted as a principal in arranging for and controlling services provided directly by their contracts with primary care physicians, as well as services provided by preferred institutional care providers and specialists. Capitation payments for the ACO program were determined from an annual benchmark established by CMS. These payments, which were adjusted for variable considerations, represented revenue for providing health care services, including primary care as well as institutional and specialist care. The ACO recognized capitation revenue for providing these services in the period in which the performance obligations were satisfied by transferring services to the members. Revenue recognized by the ACO for the three and six months ended June 30, 2023 was $30,113 and $62,227, respectively. Interest income earned on our cash deposits and short-term investments is included within other revenue on the condensed consolidated statements of operations. Payments by CMS to health plans are determined via a competitive bidding process with CMS and are based upon the cost of care in a local market and the average utilization of services by the member enrolled. These payments are subject to periodic adjustments under CMS’ “risk adjustment model,” which compensates health plans based on the health severity and certain demographic factors of each individual member. Members diagnosed with certain conditions are paid at a higher monthly payment than members who are healthier. Under this risk adjustment model, CMS calculates the risk adjustment payment using diagnosis data from hospital inpatient, hospital outpatient, and physician treatment settings. The Company and health care providers collect, capture, and submit the necessary and available diagnosis data to CMS within prescribed deadlines. Both premium and capitation revenues (including Medicare Part D) are subject to adjustments under the risk adjustment model. Throughout the year, we estimate risk adjustment payments based upon the diagnosis data submitted and expected to be submitted to CMS. Those estimated risk adjustment payments are recorded as an adjustment to premium and capitation revenue. Our risk adjustment data is also subject to review by the government, including audit by regulators. Our recognized premium revenue for our Medicare Advantage Plans in California, North Carolina, Nevada, Arizona, Texas and Florida are each subject to a minimum annual medical loss ratio (“MLR”) of 85%. The MLR represents medical costs as a percentage of premium revenue. The Code of Federal Regulations defines what constitutes medical costs and premium revenue, including certain additional expenses related to improving the quality of care provided, and the exclusion of certain taxes and fees, in each case as permitted or required by CMS and applicable regulatory requirements. If the minimum MLR is not met, we are required to remit a portion of the premiums back to the federal government. The amount remitted, if any, is recognized as an adjustment to premium revenues in the condensed consolidated statements of operations. The amounts payable under this provision were immaterial at June 30, 2024 and December 31, 2023. Medicare Part D payments are also subject to a federal risk corridor program, which limits a health plan’s overall losses or profit if actual spending for basic Medicare Part D benefits is much higher or lower than what was anticipated. Risk corridor is recorded within premium revenue. The risk corridor provisions compare costs targeted in our bids or third-party payors’ bids to actual prescription drug costs, limited to actual costs that would have been incurred under the standard coverage as defined by CMS. Variances exceeding certain thresholds may result in CMS or third-party payors making additional payments to us or require us to refund a portion of the premiums we received. We estimate and recognize an adjustment to premium revenue related to these provisions based upon pharmacy claims experience. We record a receivable or payable at the contract level and classify the amount as current or long-term in our condensed consolidated balance sheet based on the timing of expected settlement. Variable consideration estimates related to ACO contract revenue are based on the most likely outcome method and that a significant reversal in the amount of cumulative revenue recognized would not occur. Receivables, including risk adjusted premium due from the government or through third-party payors, pharmacy rebates, and other receivables, are shown net of allowances for credit losses and retroactive membership adjustments. We also receive advance payments each month from CMS related to Catastrophic Reinsurance, Coverage Gap Discount, and the Low-Income Member Cost Sharing Subsidy (“Subsidies”). Reinsurance subsidies represent funding from CMS for our portion of prescription drug costs, which exceed the member’s out-of-pocket threshold or the catastrophic coverage level. Low-income cost subsidies represent funding from CMS for all or a portion of the deductible, the coinsurance and co-payment amounts above the out-of-pocket threshold for low-income beneficiaries. Additionally, the Health Care Reform Law mandates consumer discounts of 75% on brand-name prescription drugs for Part D plan participants in the coverage gap. The majority of the discounts are funded by the pharmaceutical manufacturers, while we fund a smaller portion and administer the application of the total discount. These Subsidies represent cost reimbursements under the Medicare Part D program and are recorded as deposits or payables. These Subsidies received in excess of, or less than, actual subsidized benefits paid are refundable to or recoverable from CMS through an annual reconciliation process following the end of the contract year.
|
| Property and Equipment—Net |
Depreciation expense is computed using the straight-line method generally based on the following estimated useful lives: | | | | | | | Description | Estimated Service Lives (years) | | Computer and equipment | 5 | | Office equipment and furniture | 5-7 | | Software | 3-5 | | Leasehold improvements | 15 (or lease term, if shorter) |
|
| Medical Expenses and Medical Expenses Payable |
Medical Expenses Medical expenses include claim payments, capitation payments, pharmacy costs net of rebates, allocations of certain centralized expenses, internal care delivery expenses and various other costs incurred to provide health insurance coverage and care to members, as well as estimates of future payments to hospitals and others for medical care and other supplemental benefits provided. We have contracts with a network of hospitals, physicians, and other providers and compensate those providers and ancillary organizations based on contractual arrangements or CMS Medicare compensation guidelines. We pay these contracting providers either through fee-for-service arrangement in which the provider is paid negotiated rates for specific services provided or a capitation payment, which represent monthly contractual fees disbursed for each member regardless of medical services provided to the member. We are responsible for the entirety of the cost of health care services related to the member population, in addition to supplemental benefits provided by us to our seniors. In 2023, we also recorded claims expenses related to our institutional and specialist care related to our ACO program with CMS as we acted as the principal in the transaction. As discussed above, beginning in 2024, claims expense related to the ACO program is netted against ACO revenue as we act as the agent in these transactions. Capitation-related expenses are recorded on an accrual basis during the coverage period. Expenses related to fee-for-service contracts are recorded in the period in which the related services are dispensed. Pharmacy costs represent payments for members’ prescription drug benefits, net of rebates from drug manufacturers. Receivables for such pharmacy rebates are included in accounts receivable in the condensed consolidated balance sheet. In August 2022, the Inflation Reduction Act ("IRA") was signed into law. The law intends to increase tax revenue and reduce Medicare costs through lower prescription drug prices, inflation rebates, and capping annual Medicare Part D out of pocket expenses. The provisions of the law are set to take effect over the next seven years. There was no material impact on our consolidated financial statements at June 30, 2024, and we do not anticipate a material impact to operations for the remainder of fiscal year 2024. We are in the process of evaluating the impact the IRA will have on our business for fiscal years beyond 2024. Medical Expenses Payable Medical expenses payable includes estimates of our obligations for medical care services that have been rendered on behalf of our members and the members of the third-party payors, but for which claims have either not yet been received or processed, loss adjustment expense reserve for the expected costs of settling these claims, and for liabilities related to physician, hospital, and other medical cost disputes. We develop estimates for medical expenses incurred but not yet paid (“IBNP”), which includes an estimate for claims incurred but not reported (“IBNR”) and a payable for adjudicated claims. IBNR is estimated using an actuarial process that is consistently applied and centrally controlled. Medical expenses payable also includes an estimate for the costs necessary to process unpaid claims at the end of each period. We estimate the IBNR liability using actuarial methods that are commonly used by health insurance actuaries and meet Actuarial Standards of Practice. These actuarial methods consider factors, such as cost trends and completion factors that are assessed based on historical data for payment patterns, product mix, seasonality, utilization of health care services, and other relevant factors. Each period, we re-examine previously established IBNR estimates based on actual claim submissions and other changes in facts and circumstances. As the IBNR estimates recorded in prior periods develop, we adjust the amount of the estimates and include the changes in estimates in medical expenses in the period in which the change is identified. Actuarial Standards of Practice generally require that the IBNP estimates be adequate to cover obligations under moderately adverse conditions. Moderately adverse conditions are situations in which the actual claims are expected to be higher than the otherwise estimated value of such claims at the time of estimate. In many situations, the claims amount ultimately settled will be different than the estimate that satisfies the Actuarial Standards of Practice. We include in our IBNP an estimate for medical claims liability under moderately adverse conditions, which represents the risk of adverse deviation of the estimates in our actuarial method of reserving. We believe that medical expenses payable is adequate to cover future claims payments required. However, such estimates are based on knowledge of current events and anticipated future events. Therefore, the actual liability could differ materially from the amounts provided. We reassess the profitability of contracts for providing coverage to members when current operating results or forecasts indicate probable future losses. A premium deficiency reserve is established in current operations to the extent that the sum of expected future costs, claim adjustment expenses, and maintenance costs exceed related future premiums under contracts without consideration of investment income. For purposes of determining premium deficiencies, contracts are grouped in a manner consistent with the method of acquiring, servicing, and measuring the profitability of such contracts. Losses recognized as a premium deficiency result in a beneficial effect in subsequent periods as operating losses under these contracts are charged to the liability previously established.
|
| Part D Subsidies |
Premium revenue is derived monthly from the federal government based on our contracts with the Centers for Medicare and Medicaid Services (“CMS”). In accordance with these arrangements, we assume the responsibility for the outcomes and the economic risk of funding our members’ health care, supplemental benefits and related administration costs. We recognize premium revenue in the month that members are entitled to receive health care services, and premiums collected in advance are deferred. The monthly reimbursement includes a fixed payment per member per month (“PMPM”), which is adjusted based on certain risk factors derived from medical diagnoses and conditions of our members. The adjustments are estimated by projecting the ultimate annual premium and are recognized ratably during the year, with adjustments each period to reflect changes in the estimated ultimate premium. Premiums are also recorded net of estimated uncollectible amounts and retroactive membership adjustments. Capitation revenue consists primarily of capitated fees for medical care services provided by us under arrangements with third-party payors. In 2023, capitation revenue consisted primarily of revenue from CMS related to our participation in the CMS "ACO Realizing Equity, Access, and Community Health Model” or “ACO REACH” model, as discussed below. Under those arrangements with third-party payors, we receive a PMPM payment for a defined member population, and we are responsible for providing health care services to the member population over the contract period. We are solely responsible for the cost of health care services related to the member population and in some cases, we are financially responsible for the supplemental benefits provided by us to the members. We act as a principal in arranging for and controlling the services provided by our provider network and we are at risk for arranging and providing health care services. The premium and capitation payments we receive monthly from CMS for our members are determined from our annual bid or similarly from third-party payors under our capitation arrangement. These payments represent revenues for providing health care coverage, including Medicare Part D benefits. Under the Medicare Part D program, our members and the members of the third-party payors receive standard drug benefits. We may also provide enhanced benefits at our own expense. We recognize premium or capitation revenue for providing this insurance coverage in the month that members are entitled to receive health care services and any premium or capitation collected in advance is deferred. Our CMS payment related to Medicare Part D is subject to risk sharing through the Medicare Part D risk corridor provisions. We also participate in the CMS ACO REACH program, formerly the Direct Contracting Model ("DCE"). CMS serves as the claim adjudicator for institutional and specialists care, and directly pays for such fee for service claims. The ACO REACH entity ("ACO") is responsible for the cost of health care services related to the patient population attributed to the ACO by participating in 100% savings/losses via the risk share model and in some cases, are financially responsible for the supplemental benefits provided to the patients. In 2024, we entered into a management services and risk management agreement with a third-party healthcare company. The third party will be responsible for arranging and controlling the health care services provided to the ACO members, and for providing certain management and support services with respect to ACO operations. The third party will also assume specified upside and downside financial risk relative to the ACO’s performance. As a result of this arrangement, revenue is recorded on a net basis within other revenue on the condensed consolidated statement of operations for the three and six months ended June 30, 2024. Revenue recognized by the ACO for the three and six months ended June 30, 2024 was $(744) and $241, respectively. Prior to 2024, the ACO acted as a principal in arranging for and controlling services provided directly by their contracts with primary care physicians, as well as services provided by preferred institutional care providers and specialists. Capitation payments for the ACO program were determined from an annual benchmark established by CMS. These payments, which were adjusted for variable considerations, represented revenue for providing health care services, including primary care as well as institutional and specialist care. The ACO recognized capitation revenue for providing these services in the period in which the performance obligations were satisfied by transferring services to the members. Revenue recognized by the ACO for the three and six months ended June 30, 2023 was $30,113 and $62,227, respectively. Interest income earned on our cash deposits and short-term investments is included within other revenue on the condensed consolidated statements of operations. Payments by CMS to health plans are determined via a competitive bidding process with CMS and are based upon the cost of care in a local market and the average utilization of services by the member enrolled. These payments are subject to periodic adjustments under CMS’ “risk adjustment model,” which compensates health plans based on the health severity and certain demographic factors of each individual member. Members diagnosed with certain conditions are paid at a higher monthly payment than members who are healthier. Under this risk adjustment model, CMS calculates the risk adjustment payment using diagnosis data from hospital inpatient, hospital outpatient, and physician treatment settings. The Company and health care providers collect, capture, and submit the necessary and available diagnosis data to CMS within prescribed deadlines. Both premium and capitation revenues (including Medicare Part D) are subject to adjustments under the risk adjustment model. Throughout the year, we estimate risk adjustment payments based upon the diagnosis data submitted and expected to be submitted to CMS. Those estimated risk adjustment payments are recorded as an adjustment to premium and capitation revenue. Our risk adjustment data is also subject to review by the government, including audit by regulators. Our recognized premium revenue for our Medicare Advantage Plans in California, North Carolina, Nevada, Arizona, Texas and Florida are each subject to a minimum annual medical loss ratio (“MLR”) of 85%. The MLR represents medical costs as a percentage of premium revenue. The Code of Federal Regulations defines what constitutes medical costs and premium revenue, including certain additional expenses related to improving the quality of care provided, and the exclusion of certain taxes and fees, in each case as permitted or required by CMS and applicable regulatory requirements. If the minimum MLR is not met, we are required to remit a portion of the premiums back to the federal government. The amount remitted, if any, is recognized as an adjustment to premium revenues in the condensed consolidated statements of operations. The amounts payable under this provision were immaterial at June 30, 2024 and December 31, 2023. Medicare Part D payments are also subject to a federal risk corridor program, which limits a health plan’s overall losses or profit if actual spending for basic Medicare Part D benefits is much higher or lower than what was anticipated. Risk corridor is recorded within premium revenue. The risk corridor provisions compare costs targeted in our bids or third-party payors’ bids to actual prescription drug costs, limited to actual costs that would have been incurred under the standard coverage as defined by CMS. Variances exceeding certain thresholds may result in CMS or third-party payors making additional payments to us or require us to refund a portion of the premiums we received. We estimate and recognize an adjustment to premium revenue related to these provisions based upon pharmacy claims experience. We record a receivable or payable at the contract level and classify the amount as current or long-term in our condensed consolidated balance sheet based on the timing of expected settlement. Variable consideration estimates related to ACO contract revenue are based on the most likely outcome method and that a significant reversal in the amount of cumulative revenue recognized would not occur. Receivables, including risk adjusted premium due from the government or through third-party payors, pharmacy rebates, and other receivables, are shown net of allowances for credit losses and retroactive membership adjustments. We also receive advance payments each month from CMS related to Catastrophic Reinsurance, Coverage Gap Discount, and the Low-Income Member Cost Sharing Subsidy (“Subsidies”). Reinsurance subsidies represent funding from CMS for our portion of prescription drug costs, which exceed the member’s out-of-pocket threshold or the catastrophic coverage level. Low-income cost subsidies represent funding from CMS for all or a portion of the deductible, the coinsurance and co-payment amounts above the out-of-pocket threshold for low-income beneficiaries. Additionally, the Health Care Reform Law mandates consumer discounts of 75% on brand-name prescription drugs for Part D plan participants in the coverage gap. The majority of the discounts are funded by the pharmaceutical manufacturers, while we fund a smaller portion and administer the application of the total discount. These Subsidies represent cost reimbursements under the Medicare Part D program and are recorded as deposits or payables. These Subsidies received in excess of, or less than, actual subsidized benefits paid are refundable to or recoverable from CMS through an annual reconciliation process following the end of the contract year.
|
| Shared Risk Reserve Arrangements |
We established a fund (also referred to as “a pool”) for risk and profit-sharing with various independent physician associations (“IPAs”). The pool enables us and our IPAs to share in the financial responsibility and/or upside associated with providing covered medical expenses to our members. The risk pool is based on a contractually agreed upon medical budget, typically based upon a percentage of revenue. If actual medical expenses are less than the budgeted amount, this results in a surplus. Conversely, if actual medical expenses are greater than the budgeted amount, this results in a deficit. We will distribute the surplus, or a portion thereof, to each IPA based upon contractual terms. Deficits are charged to shared risk providers’ risk pool as per the contractual term and evaluated for collectability at each reporting period. We record risk-sharing receivables and payables on a gross basis on the condensed consolidated balance sheet. Throughout the year, we evaluate expected losses on risk-sharing receivables and record the resulting expected losses to the reserve. We systematically build and release reserves based on adequacy and its assessment of expected losses on a monthly basis. Credit loss associated with risk share deficit receivables are recorded within medical expense in the condensed consolidated statements of operations. As of June 30, 2024 and December 31, 2023, we recorded a valuation allowance for substantially all of the risk-sharing receivable balance due to collection risk related to the balance. The risk-sharing payable is included within medical expenses payable on the condensed consolidated balance sheet.
|
| Concentrations of Credit Risk |
Financial instruments that potentially subject us to concentrations of credit risk consist primarily of cash deposits and current and restricted investments with financial institutions. Accounts at each financial institution are insured by the Federal Deposit Insurance Corporation (“FDIC”) up to certain limits.
|
| Equity-Based Compensation |
Equity-based compensation expense is measured and recognized based on the grant date fair value of the awards. The grant date fair value of stock options is estimated using the Black-Scholes option pricing model. The grant date fair value of restricted stock units (“RSUs”) and restricted stock awards (“RSAs”) is estimated based on the fair value of our underlying common stock on the date of grant. The Black-Scholes option pricing model requires the use of highly subjective assumptions, including the award’s expected term, the fair value of the underlying common stock, the expected volatility of the price of the common stock, risk-free interest rates, and the expected dividend yield of the common stock. The assumptions used to determine the fair value of the stock-based awards are management’s best estimates and involve inherent uncertainties and the application of judgment. The expected term represents the period the stock-based awards are expected to be outstanding. As we do not have sufficient historical experience for determining the expected term of the stock option awards granted, we utilize the simplified method available under U.S. GAAP. As we do not have a substantial trading history, volatility assumptions were developed using a combination of the Company's historical volatility and the historical volatilities of a set of peer companies, adjusted for debt-equity leverage. Equity-based compensation expense for awards with service-based vesting only is recognized on a graded vesting schedule over the requisite service period of the awards, which is generally four years. Equity-based compensation expense for RSU awards with performance-based vesting is recognized over the requisite service period on a graded vesting schedule and is only recognized when the Company concludes that it is probable that the performance condition(s) will be achieved. At each reporting period, the Company reassesses the probability of achieving the performance criteria. Determining whether the performance criteria will be achieved involves judgment, and the estimate of share-based compensation expense may be revised periodically based on changes in the probability of achieving the performance criteria. Revisions are reflected in the period in which the estimate is changed. We account for forfeitures as they occur. Equity-based compensation is recorded within selling, general and administrative expenses, and medical expenses based on the function of the applicable employee and non-employee.
|
| Noncontrolling Interest |
In October 2022, the Company acquired a subsidiary and recorded a noncontrolling interest for the portion of equity ownership not attributable to Alignment Healthcare, Inc. The noncontrolling interest in the subsidiary was initially recognized at estimated fair value on October 1, 2022 and is presented within total equity in the Company's condensed consolidated balance sheet.
|
| Net Loss per Share |
Net loss per share is calculated based on net loss attributable to Alignment Healthcare, Inc.'s stockholders. The following table sets forth the computation of basic and diluted net loss per share for the three and six months ended June 30, 2024 and 2023: | | | | | | | | | | | | | | | | | | | | | | | | | | Three Months Ended
June 30, | | Six Months Ended
June 30, | | | 2024 | | 2023 | | 2024 | | 2023 | | Numerator: | | | | | | | | | Net loss | $ | (24,003) | | | $ | (28,494) | | | $ | (70,578) | | | $ | (65,865) | | | Less: Net (income) loss attributable to noncontrolling interests | (7) | | | 17 | | | 47 | | | 104 | | | Net loss attributable to Alignment Healthcare, Inc. | $ | (24,010) | | | $ | (28,477) | | | $ | (70,531) | | | $ | (65,761) | | | Denominator: | | | | | | | | | Total weighted-average common shares outstanding - basic and diluted | 191,431,917 | | 188,496,252 | | 190,514,927 | | 188,029,447 | | Less: Restricted shares of common stock | (540,130) | | (2,504,792) | | (566,202) | | (3,468,795) | | Total weighted-average common shares outstanding, net of restricted shares of common stock - basic and diluted | 190,891,787 | | 185,991,460 | | 189,948,725 | | 184,560,652 | | Net loss per share: | | | | | | | | | Net loss per share - basic and diluted | $ | (0.13) | | | $ | (0.15) | | | $ | (0.37) | | | $ | (0.36) | |
Basic net loss per share is the same as diluted net loss per share for periods presented as the inclusion of all potentially dilutive shares would have been anti-dilutive.
|
| Recent Accounting Pronouncements Issued |
In November 2023, the FASB issued a new accounting standard around segment disclosures. The new standard requires a public entity to disclose significant segment expenses and other segment items on an annual and interim basis and provide, in interim periods, all disclosures about a reportable segment’s profit or loss and assets that are currently required annually. Additionally, it requires a public entity to disclose the title and position of the Chief Operating Decision Maker. The ASU does not change how a public entity identifies its operating segments, aggregates them, or applies the quantitative thresholds to determine its reportable segments. The new standard is effective for fiscal years beginning after December 15, 2023, and interim periods within fiscal years beginning after December 15, 2024, with early adoption permitted. A public entity should apply the amendments in this ASU retrospectively to all prior periods presented in the financial statements. We expect this ASU to only impact our disclosures with no impacts to our results of operations, cash flows and financial condition.
|
| X |
- DefinitionDisclosure of medical expenses and medical expense payable.
| Name: |
alhc_MedicalExpensesAndMedicalExpensePayablePolicyTextBlock |
| Namespace Prefix: |
alhc_ |
| Data Type: |
dtr-types:textBlockItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionNoncontrolling Interest In Subsidiaries
| Name: |
alhc_NoncontrollingInterestInSubsidiariesPolicyPolicyTextBlock |
| Namespace Prefix: |
alhc_ |
| Data Type: |
dtr-types:textBlockItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionDisclosure of accounting policies of shared risk reserve arrangements.
| Name: |
alhc_SharedRiskReserveArrangementsPolicyTextBlock |
| Namespace Prefix: |
alhc_ |
| Data Type: |
dtr-types:textBlockItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- References
+ Details
| Name: |
us-gaap_AccountingPoliciesAbstract |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:stringItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionDisclosure of accounting policy for basis of accounting, or basis of presentation, used to prepare the financial statements (for example, US Generally Accepted Accounting Principles, Other Comprehensive Basis of Accounting, IFRS).
| Name: |
us-gaap_BasisOfAccountingPolicyPolicyTextBlock |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
dtr-types:textBlockItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionDisclosure of accounting policy for credit risk. Reference 1: http://fasb.org/us-gaap/role/ref/legacyRef
-Name Accounting Standards Codification
-Topic 942
-SubTopic 825
-Section 50
-Paragraph 1
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147478898/942-825-50-1
Reference 2: http://www.xbrl.org/2003/role/disclosureRef
-Name Accounting Standards Codification
-Section 50
-Paragraph 1
-Subparagraph (d)
-SubTopic 10
-Topic 275
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482861/275-10-50-1
| Name: |
us-gaap_ConcentrationRiskCreditRisk |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
dtr-types:textBlockItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionDisclosure of accounting policy for computing basic and diluted earnings or loss per share for each class of common stock and participating security. Addresses all significant policy factors, including any antidilutive items that have been excluded from the computation and takes into account stock dividends, splits and reverse splits that occur after the balance sheet date of the latest reporting period but before the issuance of the financial statements. Reference 1: http://www.xbrl.org/2003/role/disclosureRef
-Topic 260
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 1
-Subparagraph (d)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482662/260-10-50-1
Reference 2: http://fasb.org/us-gaap/role/ref/legacyRef
-Name Accounting Standards Codification
-Topic 260
-SubTopic 10
-Section 50
-Paragraph 1
-Subparagraph (c)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482662/260-10-50-1
Reference 3: http://fasb.org/us-gaap/role/ref/legacyRef
-Name Accounting Standards Codification
-Topic 260
-SubTopic 10
-Section 50
-Paragraph 2
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482662/260-10-50-2
| Name: |
us-gaap_EarningsPerSharePolicyTextBlock |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
dtr-types:textBlockItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionDisclosure of accounting policy for fair value measurements of financial and non-financial assets, liabilities and instruments classified in shareholders' equity. Disclosures include, but are not limited to, how an entity that manages a group of financial assets and liabilities on the basis of its net exposure measures the fair value of those assets and liabilities.
| Name: |
us-gaap_FairValueMeasurementPolicyPolicyTextBlock |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
dtr-types:textBlockItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionDisclosure of accounting policy pertaining to new accounting pronouncements that may impact the entity's financial reporting. Includes, but is not limited to, quantification of the expected or actual impact.
| Name: |
us-gaap_NewAccountingPronouncementsPolicyPolicyTextBlock |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
dtr-types:textBlockItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionDisclosure of accounting policy for long-lived, physical asset used in normal conduct of business and not intended for resale. Includes, but is not limited to, work of art, historical treasure, and similar asset classified as collections. Reference 1: http://fasb.org/us-gaap/role/ref/legacyRef
-Name Accounting Standards Codification
-Section 50
-Paragraph 1
-SubTopic 10
-Topic 360
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482099/360-10-50-1
Reference 2: http://www.xbrl.org/2003/role/disclosureRef
-Topic 944
-SubTopic 210
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.7-03(a)(8)(a))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147478777/944-210-S99-1
Reference 3: http://www.xbrl.org/2003/role/disclosureRef
-Name Accounting Standards Codification
-Section 50
-Paragraph 6
-SubTopic 360
-Topic 958
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147477798/958-360-50-6
Reference 4: http://www.xbrl.org/2003/role/disclosureRef
-Name Accounting Standards Codification
-Section 50
-Paragraph 1
-Subparagraph (d)
-SubTopic 360
-Topic 958
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147477798/958-360-50-1
| Name: |
us-gaap_PropertyPlantAndEquipmentPolicyTextBlock |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
dtr-types:textBlockItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionDisclosure of accounting policy for revenue. Includes revenue from contract with customer and from other sources. Reference 1: http://www.xbrl.org/2003/role/disclosureRef
-Topic 946
-SubTopic 220
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.6-07(1))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147479134/946-220-S99-1
Reference 2: http://www.xbrl.org/2003/role/exampleRef
-Topic 235
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 4
-Subparagraph (f)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147483426/235-10-50-4
Reference 3: http://www.xbrl.org/2003/role/exampleRef
-Name Accounting Standards Codification
-Section 50
-Paragraph 4
-Subparagraph (e)
-SubTopic 10
-Topic 235
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147483426/235-10-50-4
| Name: |
us-gaap_RevenueRecognitionPolicyTextBlock |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
dtr-types:textBlockItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionDisclosure of accounting policy for segment reporting. Reference 1: http://www.xbrl.org/2003/role/disclosureRef
-Topic 280
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 41
-Subparagraph (a)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482810/280-10-50-41
Reference 2: http://www.xbrl.org/2003/role/exampleRef
-Topic 280
-SubTopic 10
-Name Accounting Standards Codification
-Section 55
-Paragraph 47
-Subparagraph (bb)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482785/280-10-55-47
Reference 3: http://www.xbrl.org/2003/role/disclosureRef
-Topic 280
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 29
-Subparagraph (f)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482810/280-10-50-29
Reference 4: http://www.xbrl.org/2003/role/exampleRef
-Topic 280
-SubTopic 10
-Name Accounting Standards Codification
-Section 55
-Paragraph 54
-Subparagraph (b)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482785/280-10-55-54
Reference 5: http://www.xbrl.org/2003/role/disclosureRef
-Topic 280
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 36
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482810/280-10-50-36
Reference 6: http://www.xbrl.org/2003/role/exampleRef
-Topic 280
-SubTopic 10
-Name Accounting Standards Codification
-Section 55
-Paragraph 47
-Subparagraph (b)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482785/280-10-55-47
Reference 7: http://www.xbrl.org/2003/role/disclosureRef
-Topic 280
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 29
-Subparagraph (d)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482810/280-10-50-29
Reference 8: http://www.xbrl.org/2003/role/disclosureRef
-Topic 280
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 29
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482810/280-10-50-29
Reference 9: http://www.xbrl.org/2003/role/disclosureRef
-Topic 280
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 29
-Subparagraph (a)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482810/280-10-50-29
Reference 10: http://www.xbrl.org/2003/role/disclosureRef
-Topic 280
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 29
-Subparagraph (b)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482810/280-10-50-29
Reference 11: http://www.xbrl.org/2003/role/disclosureRef
-Topic 280
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 29
-Subparagraph (c)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482810/280-10-50-29
Reference 12: http://www.xbrl.org/2003/role/disclosureRef
-Topic 280
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 29
-Subparagraph (e)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482810/280-10-50-29
| Name: |
us-gaap_SegmentReportingPolicyPolicyTextBlock |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
dtr-types:textBlockItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionDisclosure of accounting policy for award under share-based payment arrangement. Includes, but is not limited to, methodology and assumption used in measuring cost. Reference 1: http://www.xbrl.org/2003/role/disclosureRef
-Topic 718
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 2
-Subparagraph (f)(1)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480429/718-10-50-2
Reference 2: http://www.xbrl.org/2003/role/disclosureRef
-Topic 718
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 2
-Subparagraph (f)(2)(i)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480429/718-10-50-2
Reference 3: http://www.xbrl.org/2003/role/disclosureRef
-Topic 718
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 2
-Subparagraph (f)(2)(ii)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480429/718-10-50-2
Reference 4: http://www.xbrl.org/2003/role/disclosureRef
-Topic 718
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 2
-Subparagraph (f)(2)(v)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480429/718-10-50-2
Reference 5: http://www.xbrl.org/2003/role/disclosureRef
-Topic 718
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SAB Topic 14.C.Q3)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147479830/718-10-S99-1
Reference 6: http://www.xbrl.org/2003/role/disclosureRef
-Topic 718
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SAB Topic 14.D.1.Q5)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147479830/718-10-S99-1
Reference 7: http://www.xbrl.org/2003/role/disclosureRef
-Topic 718
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SAB Topic 14.D.3.Q2)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147479830/718-10-S99-1
Reference 8: http://www.xbrl.org/2003/role/disclosureRef
-Topic 718
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SAB Topic 14.D.2.Q6)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147479830/718-10-S99-1
Reference 9: http://www.xbrl.org/2003/role/disclosureRef
-Topic 718
-Name Accounting Standards Codification
-Publisher FASB
-URI https://asc.fasb.org/718/tableOfContent
Reference 10: http://www.xbrl.org/2003/role/disclosureRef
-Topic 718
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 2
-Subparagraph (b)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480429/718-10-50-2
Reference 11: http://www.xbrl.org/2003/role/disclosureRef
-Topic 718
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 2
-Subparagraph (f)(2)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480429/718-10-50-2
| Name: |
us-gaap_ShareBasedCompensationOptionAndIncentivePlansPolicy |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
dtr-types:textBlockItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionDisclosure of accounting policy for the use of estimates in the preparation of financial statements in conformity with generally accepted accounting principles. Reference 1: http://fasb.org/us-gaap/role/ref/legacyRef
-Name Accounting Standards Codification
-Topic 275
-SubTopic 10
-Section 50
-Paragraph 9
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482861/275-10-50-9
Reference 2: http://fasb.org/us-gaap/role/ref/legacyRef
-Name Accounting Standards Codification
-Topic 275
-SubTopic 10
-Section 50
-Paragraph 4
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482861/275-10-50-4
Reference 3: http://www.xbrl.org/2003/role/disclosureRef
-Name Accounting Standards Codification
-Section 50
-Paragraph 1
-Subparagraph (b)
-SubTopic 10
-Topic 275
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482861/275-10-50-1
Reference 4: http://www.xbrl.org/2003/role/disclosureRef
-Name Accounting Standards Codification
-Section 50
-Paragraph 1
-Subparagraph (c)
-SubTopic 10
-Topic 275
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482861/275-10-50-1
Reference 5: http://www.xbrl.org/2003/role/disclosureRef
-Name Accounting Standards Codification
-Section 50
-Paragraph 11
-SubTopic 10
-Topic 275
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482861/275-10-50-11
Reference 6: http://www.xbrl.org/2003/role/disclosureRef
-Name Accounting Standards Codification
-Section 50
-Paragraph 12
-SubTopic 10
-Topic 275
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482861/275-10-50-12
Reference 7: http://fasb.org/us-gaap/role/ref/legacyRef
-Name Accounting Standards Codification
-Topic 275
-SubTopic 10
-Section 50
-Paragraph 8
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482861/275-10-50-8
| Name: |
us-gaap_UseOfEstimates |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
dtr-types:textBlockItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
v3.24.2.u1
Summary of Significant Accounting Policies (Tables)
|
6 Months Ended |
Jun. 30, 2024 |
|---|
| Accounting Policies [Abstract] |
|
| Schedule of Earned Revenue |
Earned premium revenue consisted of premium revenue and capitation revenue for the three and six months ended June 30, 2024 and 2023 were as follows: | | | | | | | | | | | | | | | | | | | | | | | | | Three Months Ended
June 30, | | Six Months Ended
June 30, | | 2024 | | 2023 | | 2024 | | 2023 | | Premium | $ | 673,532 | | | $ | 424,704 | | | $ | 1,293,254 | | | $ | 824,444 | | | Capitation | 562 | | | 32,173 | | | 2,396 | | | 67,245 | | | Total | $ | 674,094 | | | $ | 456,877 | | | $ | 1,295,650 | | | $ | 891,689 | |
|
| Schedule of Property and Equipment |
Depreciation expense is computed using the straight-line method generally based on the following estimated useful lives: | | | | | | | Description | Estimated Service Lives (years) | | Computer and equipment | 5 | | Office equipment and furniture | 5-7 | | Software | 3-5 | | Leasehold improvements | 15 (or lease term, if shorter) |
Property and equipment consisted of the following as of June 30, 2024 and December 31, 2023: | | | | | | | | | | | | | June 30,
2024 | | December 31,
2023 | | Computers and equipment | $ | 12,235 | | | $ | 11,447 | | | Office equipment and furniture | 4,397 | | | 4,396 | | | Software | 165,697 | | | 148,864 | | | Leasehold improvements | 6,347 | | | 6,347 | | | Construction in progress | 9,887 | | | 4,532 | | | Subtotal | 198,563 | | | 175,586 | | | Less accumulated depreciation | (136,133) | | | (123,685) | | | Property and equipment-net | $ | 62,430 | | | $ | 51,901 | |
|
| Schedule of Computation of Basic and Diluted Net Loss Per Share |
The following table sets forth the computation of basic and diluted net loss per share for the three and six months ended June 30, 2024 and 2023: | | | | | | | | | | | | | | | | | | | | | | | | | | Three Months Ended
June 30, | | Six Months Ended
June 30, | | | 2024 | | 2023 | | 2024 | | 2023 | | Numerator: | | | | | | | | | Net loss | $ | (24,003) | | | $ | (28,494) | | | $ | (70,578) | | | $ | (65,865) | | | Less: Net (income) loss attributable to noncontrolling interests | (7) | | | 17 | | | 47 | | | 104 | | | Net loss attributable to Alignment Healthcare, Inc. | $ | (24,010) | | | $ | (28,477) | | | $ | (70,531) | | | $ | (65,761) | | | Denominator: | | | | | | | | | Total weighted-average common shares outstanding - basic and diluted | 191,431,917 | | 188,496,252 | | 190,514,927 | | 188,029,447 | | Less: Restricted shares of common stock | (540,130) | | (2,504,792) | | (566,202) | | (3,468,795) | | Total weighted-average common shares outstanding, net of restricted shares of common stock - basic and diluted | 190,891,787 | | 185,991,460 | | 189,948,725 | | 184,560,652 | | Net loss per share: | | | | | | | | | Net loss per share - basic and diluted | $ | (0.13) | | | $ | (0.15) | | | $ | (0.37) | | | $ | (0.36) | |
|
| Schedule of Computation of Diluted Net Loss Per Share |
In addition to the restricted shares of common stock, we also excluded the following potential common shares, presented based on amounts outstanding at each period end, from the computation of diluted net loss per share as of June 30, 2024 and 2023: | | | | | | | | | | | | | | June 30, | | | 2024 | | 2023 | | Stock options | 8,949,589 | | 10,566,529 | | Restricted stock units | 22,196,478 | | 10,145,593 | | Total | 31,146,067 | | 20,712,122 |
|
| X |
- References
+ Details
| Name: |
us-gaap_AccountingPoliciesAbstract |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:stringItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionTabular disclosure of disaggregation of revenue into categories depicting how nature, amount, timing, and uncertainty of revenue and cash flows are affected by economic factor. Reference 1: http://www.xbrl.org/2009/role/commonPracticeRef
-Topic 606
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 5
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147479806/606-10-50-5
| Name: |
us-gaap_DisaggregationOfRevenueTableTextBlock |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
dtr-types:textBlockItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionTabular disclosure of physical assets used in the normal conduct of business and not intended for resale. Includes, but is not limited to, balances by class of assets, depreciation and depletion expense and method used, including composite depreciation, and accumulated deprecation. Reference 1: http://fasb.org/us-gaap/role/ref/legacyRef
-Name Accounting Standards Codification
-Section 50
-Paragraph 1
-SubTopic 10
-Topic 360
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482099/360-10-50-1
| Name: |
us-gaap_PropertyPlantAndEquipmentTextBlock |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
dtr-types:textBlockItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionTabular disclosure of an entity's basic and diluted earnings per share calculations, including a reconciliation of numerators and denominators of the basic and diluted per-share computations for income from continuing operations. Reference 1: http://www.xbrl.org/2009/role/commonPracticeRef
-Topic 260
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 1
-Subparagraph (a)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482662/260-10-50-1
| Name: |
us-gaap_ScheduleOfEarningsPerShareBasicAndDilutedTableTextBlock |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
dtr-types:textBlockItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionTabular disclosure of the effect of income (loss) on an entity's diluted earnings per share. Reference 1: http://www.xbrl.org/2009/role/commonPracticeRef
-Topic 260
-SubTopic 10
-Name Accounting Standards Codification
-Section 45
-Paragraph 3
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482689/260-10-45-3
Reference 2: http://fasb.org/us-gaap/role/ref/legacyRef
-Name Accounting Standards Codification
-Topic 260
-SubTopic 10
-Section 50
-Paragraph 1
-Subparagraph (a)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482662/260-10-50-1
Reference 3: http://fasb.org/us-gaap/role/ref/legacyRef
-Name Accounting Standards Codification
-Topic 260
-SubTopic 10
-Section 55
-Paragraph 52
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482635/260-10-55-52
| Name: |
us-gaap_ScheduleOfEarningsPerShareDilutedByCommonClassTextBlock |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
dtr-types:textBlockItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
v3.24.2.u1
Fair Value (Tables)
|
6 Months Ended |
Jun. 30, 2024 |
|---|
| Fair Value Disclosures [Abstract] |
|
| Schedule of Carrying Value and Fair Value of Financial Instruments |
The following tables present the carrying value and fair value of these financial instruments as of June 30, 2024 and December 31, 2023: | | | | | | | | | | | | | | | | | | | | | | | | | June 30, 2024 | | | | Fair Value | | Carrying
Value | | Level 1 | | Level 2 | | Level 3 | | U.S. Treasury bills | $ | 44,628 | | | $ | 44,577 | | | $ | — | | | $ | — | | | Certificate of deposits | 2,336 | | | — | | | 2,336 | | | — | | | Total | $ | 46,964 | | | $ | 44,577 | | | $ | 2,336 | | | $ | — | |
| | | | | | | | | | | | | | | | | | | | | | | | | December 31, 2023 | | | | Fair Value | | Carrying
Value | | Level 1 | | Level 2 | | Level 3 | | U.S. Treasury bills | $ | 117,337 | | | $ | 117,310 | | | $ | — | | | $ | — | | | Certificate of deposits | 1,755 | | | — | | | 1,755 | | | — | | | Total | $ | 119,092 | | | $ | 117,310 | | | $ | 1,755 | | | $ | — | |
|
| X |
- References
+ Details
| Name: |
us-gaap_FairValueDisclosuresAbstract |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:stringItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionTabular disclosure of assets and liabilities, including [financial] instruments measured at fair value that are classified in stockholders' equity, if any, that are measured at fair value on a recurring basis. The disclosures contemplated herein include the fair value measurements at the reporting date by the level within the fair value hierarchy in which the fair value measurements in their entirety fall, segregating fair value measurements using quoted prices in active markets for identical assets (Level 1), significant other observable inputs (Level 2), and significant unobservable inputs (Level 3). Reference 1: http://www.xbrl.org/2009/role/commonPracticeRef
-Topic 820
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 2
-Subparagraph (b)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482106/820-10-50-2
Reference 2: http://www.xbrl.org/2009/role/commonPracticeRef
-Topic 820
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 2
-Subparagraph (a)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482106/820-10-50-2
| Name: |
us-gaap_ScheduleOfFairValueAssetsAndLiabilitiesMeasuredOnRecurringBasisTableTextBlock |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
dtr-types:textBlockItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
v3.24.2.u1
Accounts Receivable (Tables)
|
6 Months Ended |
Jun. 30, 2024 |
|---|
| Accounts Receivable, after Allowance for Credit Loss [Abstract] |
|
| Schedule of Accounts Receivable |
Accounts receivable consisted of the following as of June 30, 2024 and December 31, 2023: | | | | | | | | | | | | | | June 30,
2024 | | December 31,
2023 | | Government receivables | $ | 78,529 | | | $ | 35,529 | | | Pharmacy rebate receivables | 94,695 | | | 75,894 | | | Other receivables | 10,085 | | | 8,326 | | | Total accounts receivable | 183,309 | | | 119,749 | | | Allowance for credit losses | (95) | | | — | | | Accounts receivable, net | $ | 183,214 | | | $ | 119,749 | |
|
| X |
- References
+ Details
| Name: |
us-gaap_AccountsReceivableNetAbstract |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:stringItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionTabular disclosure of the various types of trade accounts and notes receivable and for each the gross carrying value, allowance, and net carrying value as of the balance sheet date. Presentation is categorized by current, noncurrent and unclassified receivables. Reference 1: http://fasb.org/us-gaap/role/ref/legacyRef
-Topic 210
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.5-02(4))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480566/210-10-S99-1
Reference 2: http://fasb.org/us-gaap/role/ref/legacyRef
-Topic 210
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.5-02(3))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480566/210-10-S99-1
| Name: |
us-gaap_ScheduleOfAccountsNotesLoansAndFinancingReceivableTextBlock |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
dtr-types:textBlockItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
v3.24.2.u1
Property and Equipment (Tables)
|
6 Months Ended |
Jun. 30, 2024 |
|---|
| Property, Plant and Equipment [Abstract] |
|
| Schedule of Property and Equipment |
Depreciation expense is computed using the straight-line method generally based on the following estimated useful lives: | | | | | | | Description | Estimated Service Lives (years) | | Computer and equipment | 5 | | Office equipment and furniture | 5-7 | | Software | 3-5 | | Leasehold improvements | 15 (or lease term, if shorter) |
Property and equipment consisted of the following as of June 30, 2024 and December 31, 2023: | | | | | | | | | | | | | June 30,
2024 | | December 31,
2023 | | Computers and equipment | $ | 12,235 | | | $ | 11,447 | | | Office equipment and furniture | 4,397 | | | 4,396 | | | Software | 165,697 | | | 148,864 | | | Leasehold improvements | 6,347 | | | 6,347 | | | Construction in progress | 9,887 | | | 4,532 | | | Subtotal | 198,563 | | | 175,586 | | | Less accumulated depreciation | (136,133) | | | (123,685) | | | Property and equipment-net | $ | 62,430 | | | $ | 51,901 | |
|
| X |
- References
+ Details
| Name: |
us-gaap_PropertyPlantAndEquipmentAbstract |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:stringItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionTabular disclosure of physical assets used in the normal conduct of business and not intended for resale. Includes, but is not limited to, balances by class of assets, depreciation and depletion expense and method used, including composite depreciation, and accumulated deprecation. Reference 1: http://fasb.org/us-gaap/role/ref/legacyRef
-Name Accounting Standards Codification
-Section 50
-Paragraph 1
-SubTopic 10
-Topic 360
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482099/360-10-50-1
| Name: |
us-gaap_PropertyPlantAndEquipmentTextBlock |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
dtr-types:textBlockItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
v3.24.2.u1
Goodwill and Intangible Assets (Tables)
|
6 Months Ended |
Jun. 30, 2024 |
|---|
| Goodwill and Intangible Assets Disclosure [Abstract] |
|
| Schedule of Intangible Assets |
Intangible assets consisted of the following as of June 30, 2024 and December 31, 2023: | | | | | | | | | | | | | | | | | | | | | | | | | June 30, 2024 | | Gross Carrying Value | | Accumulated Amortization | | Net Carrying Value | | Weighted Average Life | | Goodwill | $ | 34,826 | | | $ | — | | | $ | 34,826 | | | — | | License (indefinite lived) | 4,967 | | | — | | | 4,967 | | | — | | Plan member relationships | 2,700 | | | (2,700) | | | — | | | 9 years | | Other | 1,050 | | | (816) | | | 234 | | | 2 - 10 years | | Total | $ | 43,543 | | | $ | (3,516) | | | $ | 40,027 | | | |
| | | | | | | | | | | | | | | | | | | | | | | | | December 31, 2023 | | Gross Carrying Value | | Accumulated Amortization | | Net Carrying Value | | Weighted Average Life | | Goodwill | $ | 34,826 | | | $ | — | | | $ | 34,826 | | | — | | License (indefinite lived) | 4,967 | | | — | | | 4,967 | | | — | | Plan member relationships | 2,700 | | | (2,700) | | | — | | | 9 years | | Other | 1,050 | | | (765) | | | 285 | | | 2 - 10 years | | Total | $ | 43,543 | | | $ | (3,465) | | | $ | 40,078 | | | |
|
| Schedule of Estimated Amortization Expense Related to Intangible Assets |
Estimated amortization expense relating to intangible assets for each of the next five years ending December 31, is as follows: | | | | | | | Remainder of 2024 | $ | 31 | | | 2025 | 60 | | | 2026 | 60 | | | 2027 | 60 | | | 2028 | 23 | | | | | $ | 234 | |
|
| X |
- References
+ Details
| Name: |
us-gaap_GoodwillAndIntangibleAssetsDisclosureAbstract |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:stringItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionTabular disclosure of goodwill and intangible assets, which may be broken down by segment or major class. Reference 1: http://www.xbrl.org/2009/role/commonPracticeRef
-Topic 350
-SubTopic 30
-Name Accounting Standards Codification
-Publisher FASB
-URI https://asc.fasb.org/350-30/tableOfContent
Reference 2: http://www.xbrl.org/2009/role/commonPracticeRef
-Topic 350
-SubTopic 20
-Name Accounting Standards Codification
-Publisher FASB
-URI https://asc.fasb.org/350-20/tableOfContent
| Name: |
us-gaap_ScheduleOfIntangibleAssetsAndGoodwillTableTextBlock |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
dtr-types:textBlockItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionTabular disclosure of the amount of amortization expense expected to be recorded in succeeding fiscal years for finite-lived intangible assets. Reference 1: http://www.xbrl.org/2003/role/exampleRef
-Topic 350
-SubTopic 30
-Name Accounting Standards Codification
-Section 55
-Paragraph 40
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482640/350-30-55-40
Reference 2: http://www.xbrl.org/2009/role/commonPracticeRef
-Topic 350
-SubTopic 30
-Name Accounting Standards Codification
-Section 50
-Paragraph 2
-Subparagraph (a)(3)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482665/350-30-50-2
| Name: |
us-gaap_ScheduleofFiniteLivedIntangibleAssetsFutureAmortizationExpenseTableTextBlock |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
dtr-types:textBlockItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
v3.24.2.u1
Medical Expenses Payable (Tables)
|
6 Months Ended |
Jun. 30, 2024 |
|---|
| Insurance [Abstract] |
|
| Schedule of Medical Expenses Payable |
The following table is a detail of medical expenses payable as of June 30, 2024 and December 31, 2023: | | | | | | | | | | | | | | June 30,
2024 | | December 31,
2023 | | Claims incurred but not paid | $ | 156,379 | | | $ | 95,664 | | | Capitation and risk-sharing payable | 69,316 | | | 50,894 | | | Other | 89,674 | | | 58,841 | | | Medical expenses payable | $ | 315,369 | | | $ | 205,399 | |
|
| Schedule of Components of Change in Medical Expenses Payable |
The following table presents components of the change in medical expenses payable as of June 30, 2024 and 2023: | | | | | | | | | | | | | June 30,
2024 | | June 30,
2023 | | Claims incurred but not paid - beginning balance | $ | 95,664 | | | $ | 88,813 | | | Incurred related to: | | | | | Current year | 407,156 | | | 235,027 | | | Prior years | (7,257) | | | (7,168) | | | Total incurred, net of reinsurance | 399,899 | | | 227,859 | | | Payments related to: | | | | | Current year | 263,824 | | | 156,152 | | | Prior years | 75,360 | | | 68,632 | | | Total payments, net of reinsurance | 339,184 | | | 224,784 | | | Claims incurred but not paid - ending balance | 156,379 | | | 91,888 | | | Capitation payable, risk-sharing payable, and other | 158,990 | | | 115,310 | | | Total medical expenses payable | $ | 315,369 | | | $ | 207,198 | |
|
| X |
- References
+ Details
| Name: |
us-gaap_InsuranceAbstract |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:stringItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionTabular disclosure of the activity in the reserve for settling insured claims and expenses incurred in the claims settlement process for the period. The estimated liability includes the amount of money that will be required for future payments of (a) claims that have been reported to the insurer, (b) claims related to insured events that have occurred but that have not been reported to the insurer as of the date the liability is estimated, and (c) claim adjustment expenses. Claim adjustment expenses include costs incurred in the claim settlement process such as legal fees; outside adjuster fees; and costs to record, process, and adjust claims. Reference 1: http://www.xbrl.org/2003/role/disclosureRef
-Topic 944
-SubTopic 40
-Name Accounting Standards Codification
-Section 50
-Paragraph 3
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480081/944-40-50-3
| Name: |
us-gaap_ScheduleOfLiabilityForUnpaidClaimsAndClaimsAdjustmentExpense |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
dtr-types:textBlockItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionTabular disclosure for the reconciliation of claims development to the liability for unpaid claims and claim adjustment expense for short-duration insurance contracts. Reference 1: http://www.xbrl.org/2003/role/exampleRef
-Topic 944
-SubTopic 40
-Name Accounting Standards Codification
-Section 55
-Paragraph 9E
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480046/944-40-55-9E
Reference 2: http://www.xbrl.org/2009/role/commonPracticeRef
-Topic 944
-SubTopic 40
-Name Accounting Standards Codification
-Section 50
-Paragraph 4C
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480081/944-40-50-4C
| Name: |
us-gaap_ShortdurationInsuranceContractsReconciliationOfClaimsDevelopmentToLiabilityTableTextBlock |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
dtr-types:textBlockItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
v3.24.2.u1
Long-Term Debt (Tables)
|
6 Months Ended |
Jun. 30, 2024 |
|---|
| Debt Disclosure [Abstract] |
|
| Schedule of Long-Term Debt Outstanding, Net of Unamortized Debt Issuance Costs |
Long-term debt is recorded at carrying value in the condensed consolidated balance sheets. The carrying value of long-term debt outstanding, net of unamortized debt issuance costs, consisted of the following as of June 30, 2024 and December 31, 2023: | | | | | | | | | | | | | June 30,
2024 | | December 31,
2023 | | Long-term debt | $ | 215,000 | | | $ | 165,000 | | | Less unamortized debt issuance costs | (3,258) | | | (3,187) | | | Long-term debt-net of amortization | 211,742 | | | 161,813 | | | Less current portion of long-term debt | — | | | — | | | Long-term debt - net of current portion | $ | 211,742 | | | $ | 161,813 | |
|
| Schedule of Future Maturities Under the Term Loan |
Future maturities under the term loan for each of the next five years ending December 31, are as follows: | | | | | | | Amount | | Remainder of 2024 | $ | — | | | 2025 | 2,150 | | | 2026 | 2,150 | | | 2027 | 210,700 | | | 2028 | — | | | $ | 215,000 | |
|
| X |
- References
+ Details
| Name: |
us-gaap_DebtDisclosureAbstract |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:stringItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionTabular disclosure of information pertaining to short-term and long-debt instruments or arrangements, including but not limited to identification of terms, features, collateral requirements and other information necessary to a fair presentation.
| Name: |
us-gaap_ScheduleOfDebtTableTextBlock |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
dtr-types:textBlockItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionTabular disclosure of maturity and sinking fund requirement for long-term debt. Reference 1: http://fasb.org/us-gaap/role/ref/legacyRef
-Name Accounting Standards Codification
-Section 50
-Paragraph 1
-SubTopic 10
-Topic 470
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147481544/470-10-50-1
| Name: |
us-gaap_ScheduleOfMaturitiesOfLongTermDebtTableTextBlock |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
dtr-types:textBlockItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
v3.24.2.u1
Equity-Based Compensation (Tables)
|
6 Months Ended |
Jun. 30, 2024 |
|---|
| Share-Based Payment Arrangement [Abstract] |
|
| Schedule of Stock Option Activity Transactions |
The following is a summary of the stock option transactions as of and for the three and six months ended June 30, 2024: | | | | | | | | | | | | | | | | | | | | | | | | | | Stock Options Outstanding | | (amounts in thousands, except shares and per share amount) | Shares Subject to Options Outstanding | | Weighted- Average Exercise Price per Option | | Weighted- Average Remaining Contractual Terms (in years) | | Aggregate Intrinsic Value | | Balances as of December 31, 2023 | 9,135,879 | | $ | 16.95 | | | 7.29 | | $ | 79 | | | Options granted | — | | — | | | | | | | Options exercised | — | | — | | | | | | | Options forfeited / expired | (112,536) | | 15.41 | | | | | | | Balances as of March 31, 2024 | 9,023,343 | | $ | 16.97 | | | 7.04 | | — | | | Options granted | — | | — | | | | | | | Options exercised | — | | — | | | | | | | Options forfeited / expired | (73,754) | | 16.62 | | | | | | | Balances as of June 30, 2024 | 8,949,589 | | $ | 16.97 | | | 6.79 | | $ | 27 | | | Vested and Exercisable as of June 30, 2024 | 6,297,452 | | $ | 17.28 | | | 6.75 | | $ | 14 | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | |
|
| Schedule of Restricted Stock Transactions |
The following is a summary of RSA transactions for the three and six months ended June 30, 2024: | | | | | | | | | | | | | | Restricted Shares | | Weighted-Average Grant Date Fair Value | | Unvested and outstanding as of December 31, 2023 | 683,953 | | $ | 5.86 | | | Vested | (140,856) | | 13.22 | | | Forfeited | (2,799) | | 5.05 | | | Unvested and outstanding as of March 31, 2024 | 540,298 | | $ | 3.94 | | | Vested | (3,056) | | 2.49 | | | Forfeited | — | | — | | | Unvested and outstanding as of June 30, 2024 | 537,242 | | $ | 3.95 | | | | | | | | | | | | | |
The following is a summary of RSU transactions as of and for the three and six months ended June 30, 2024: | | | | | | | | | | | | | | Restricted Stock Units | | Weighted-Average Grant Date Fair Value | | Unvested and outstanding as of December 31, 2023 | 10,541,625 | | $ | 11.25 | | | Granted | 6,517,337 | | 5.05 | Vested(1) | (2,385,493) | | 8.25 | | Cancelled/forfeited | (282,972) | | 9.36 | | Unvested and outstanding as of March 31, 2024 | 14,390,497 | | $ | 8.97 | | | Granted | 103,292 | | 5.62 | | Vested | (80,178) | | 6.07 | | Cancelled/forfeited | (395,338) | | 8.40 | | Unvested and outstanding as of June 30, 2024 | 14,018,273 | | $ | 8.98 | | | | | | | | | | | | | | | | | |
(1) Includes 107,948 shares that vested, but the issuance and delivery of the shares was deferred.
|
| Schedule of PSUs Transactions |
The following is a summary of PSU transactions for the three and six months ended June 30, 2024: | | | | | | | | | | | | | | Performance-based restricted stock units | | Weighted-Average Grant Date Fair Value | | Unvested and outstanding as of December 31, 2023 | 7,233,205 | | $ | 5.74 | | | Granted | 1,160,000 | | 5.00 | | | Vested | — | | — | | | Cancelled/forfeited | (16,667) | | 5.74 | | | Unvested and outstanding as of March 31, 2024 | 8,376,538 | | $ | 5.64 | | | Granted | — | | — | | | Vested | — | | — | | | Cancelled/forfeited | (198,333) | | 5.67 | | | Unvested and outstanding as of June 30, 2024 | 8,178,205 | | $ | 5.64 | |
|
| Schedule of Equity-Based Compensation Expense of Operation |
Total equity-based compensation expense was presented on the statement of operations as follows: | | | | | | | | | | | | | | | | | | | | | | | | | | Three Months Ended June 30, | | Six Months Ended June 30, | | (amounts in thousands) | 2024 | | 2023 | | 2024 | | 2023 | | Selling, general and administrative expenses | $ | 16,022 | | | $ | 13,869 | | | $ | 35,743 | | | $ | 33,323 | | | Medical expenses | 762 | | | 1,767 | | | 1,895 | | | 4,291 | | | Total equity-based compensation expense | $ | 16,784 | | | $ | 15,636 | | | $ | 37,638 | | | $ | 37,614 | |
|
| X |
- DefinitionSchedule of equity-based compensation expense on statement of operations
| Name: |
alhc_ScheduleOfEquityBasedCompensationExpenseOnStatementOfOperationsTableTextBlock |
| Namespace Prefix: |
alhc_ |
| Data Type: |
dtr-types:textBlockItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionTabular disclosure for stock option plans. Includes, but is not limited to, outstanding awards at beginning and end of year, grants, exercises, forfeitures, and weighted-average grant date fair value. Reference 1: http://fasb.org/us-gaap/role/ref/legacyRef
-Topic 718
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 2
-Subparagraph (c)(1)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480429/718-10-50-2
Reference 2: http://fasb.org/us-gaap/role/ref/legacyRef
-Name Accounting Standards Codification
-Section 50
-Paragraph 2
-Subparagraph (d)
-SubTopic 10
-Topic 718
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480429/718-10-50-2
Reference 3: http://fasb.org/us-gaap/role/ref/legacyRef
-Name Accounting Standards Codification
-Section 50
-Paragraph 2
-Subparagraph (e)
-SubTopic 10
-Topic 718
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480429/718-10-50-2
| Name: |
us-gaap_ScheduleOfShareBasedCompensationStockOptionsActivityTableTextBlock |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
dtr-types:textBlockItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionDisclosure of the number and weighted-average grant date fair value for restricted stock and restricted stock units that were outstanding at the beginning and end of the year, and the number of restricted stock and restricted stock units that were granted, vested, or forfeited during the year.
| Name: |
us-gaap_ScheduleOfSharebasedCompensationRestrictedStockAndRestrictedStockUnitsActivityTableTextBlock |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
dtr-types:textBlockItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionTabular disclosure of number and weighted-average grant date fair value for nonvested performance shares. Reference 1: http://fasb.org/us-gaap/role/ref/legacyRef
-Name Accounting Standards Codification
-Section 50
-Subparagraph (c)
-Paragraph 2
-SubTopic 10
-Topic 718
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480429/718-10-50-2
| Name: |
us-gaap_ShareBasedCompensationPerformanceSharesAwardUnvestedActivityTableTextBlock |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
dtr-types:textBlockItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
v3.24.2.u1
Summary of Significant Accounting Policies - Additional Information (Details)
|
3 Months Ended |
6 Months Ended |
12 Months Ended |
|
Jun. 30, 2024
USD ($)
|
Jun. 30, 2023
USD ($)
|
Jun. 30, 2024
USD ($)
segment
Entity
|
Jun. 30, 2023
USD ($)
|
Dec. 31, 2023
USD ($)
|
| Accounting Policies [Line Items] |
|
|
|
|
|
| Number of consolidated variable interest entities | Entity |
|
|
3
|
|
|
| Number of reporting segments | segment |
|
|
1
|
|
|
| Number of operating segments | segment |
|
|
1
|
|
|
| Assets, fair value disclosure |
$ 46,964,000
|
|
$ 46,964,000
|
|
$ 119,092,000
|
| Revenues |
681,286,000
|
$ 462,379,000
|
1,309,887,000
|
$ 901,534,000
|
|
| Interest income earned |
5,602,000
|
4,727,000
|
$ 11,045,000
|
8,444,000
|
|
| Percentage of consumer discounts on brand name |
|
|
75.00%
|
|
|
| Federal deposit insurance corporation premium expense |
|
|
$ 362,396,000
|
|
316,977,000
|
| Award requisite service period |
|
|
4 years
|
|
|
| Net loss attributable to noncontrolling interest |
(7,000)
|
17,000
|
$ 47,000
|
104,000
|
|
| Minimum |
|
|
|
|
|
| Accounting Policies [Line Items] |
|
|
|
|
|
| Loss ratio |
|
|
85.00%
|
|
|
| Realizing Equity, Access, and Community Health (REACH) Model |
|
|
|
|
|
| Accounting Policies [Line Items] |
|
|
|
|
|
| Revenues |
(744,000)
|
$ 30,113,000
|
$ 241,000
|
$ 62,227,000
|
|
| Level 3 |
|
|
|
|
|
| Accounting Policies [Line Items] |
|
|
|
|
|
| Assets, fair value disclosure |
0
|
|
0
|
|
0
|
| Liabilities, fair value disclosure |
$ 0
|
|
$ 0
|
|
$ 0
|
| X |
- DefinitionLine items represent financial concepts included in a table. These concepts are used to disclose accounting policies associated with domain members defined in one or many axes to the table.
| Name: |
alhc_AccountingPoliciesLineItems |
| Namespace Prefix: |
alhc_ |
| Data Type: |
xbrli:stringItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionNumber of consolidated variable interest entities.
| Name: |
alhc_NumberOfConsolidatedVariableInterestEntities |
| Namespace Prefix: |
alhc_ |
| Data Type: |
xbrli:integerItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionPercentage of consumer discounts on brand name.
| Name: |
alhc_PercentageOfConsumerDiscountsOnBrandName |
| Namespace Prefix: |
alhc_ |
| Data Type: |
dtr-types:percentItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionFair value portion of asset recognized for present right to economic benefit. Reference 1: http://www.xbrl.org/2003/role/exampleRef
-Topic 820
-SubTopic 10
-Name Accounting Standards Codification
-Section 55
-Paragraph 100
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482078/820-10-55-100
Reference 2: http://www.xbrl.org/2003/role/disclosureRef
-Topic 820
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 2
-Subparagraph (b)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482106/820-10-50-2
Reference 3: http://www.xbrl.org/2003/role/disclosureRef
-Topic 820
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 2
-Subparagraph (a)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482106/820-10-50-2
| Name: |
us-gaap_AssetsFairValueDisclosure |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:monetaryItemType |
| Balance Type: |
debit |
| Period Type: |
instant |
|
| X |
- DefinitionAmount of expense for Federal Deposit Insurance Corporation (FDIC) insurance. Reference 1: http://fasb.org/us-gaap/role/ref/legacyRef
-Topic 942
-SubTopic 220
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.9-04(14))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147478524/942-220-S99-1
| Name: |
us-gaap_FederalDepositInsuranceCorporationPremiumExpense |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:monetaryItemType |
| Balance Type: |
debit |
| Period Type: |
duration |
|
| X |
- DefinitionFair value of financial and nonfinancial obligations. Reference 1: http://www.xbrl.org/2009/role/commonPracticeRef
-Topic 820
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 2
-Subparagraph (a)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482106/820-10-50-2
Reference 2: http://www.xbrl.org/2003/role/disclosureRef
-Topic 820
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 2
-Subparagraph (b)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482106/820-10-50-2
| Name: |
us-gaap_LiabilitiesFairValueDisclosure |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:monetaryItemType |
| Balance Type: |
credit |
| Period Type: |
instant |
|
| X |
- DefinitionRatio of non-life losses and loss expenses to non-life net premiums earned.
| Name: |
us-gaap_LossRatio |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
dtr-types:percentItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionAmount of Net Income (Loss) attributable to noncontrolling interest. Reference 1: http://www.xbrl.org/2003/role/disclosureRef
-Topic 250
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 6
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147483443/250-10-50-6
Reference 2: http://www.xbrl.org/2003/role/disclosureRef
-Topic 250
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 9
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147483443/250-10-50-9
Reference 3: http://www.xbrl.org/2003/role/disclosureRef
-Topic 250
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 8
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147483443/250-10-50-8
Reference 4: http://www.xbrl.org/2003/role/disclosureRef
-Topic 944
-SubTopic 220
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.7-04(17))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147477250/944-220-S99-1
Reference 5: http://www.xbrl.org/2009/role/commonPracticeRef
-Topic 220
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 6
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482765/220-10-50-6
Reference 6: http://fasb.org/us-gaap/role/ref/legacyRef
-Topic 810
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 1A
-Subparagraph (a)(2)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147481203/810-10-50-1A
Reference 7: http://fasb.org/us-gaap/role/ref/legacyRef
-Name Accounting Standards Codification
-Topic 810
-SubTopic 10
-Section 55
-Paragraph 4J
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147481175/810-10-55-4J
Reference 8: http://www.xbrl.org/2003/role/disclosureRef
-Topic 220
-SubTopic 10
-Name Accounting Standards Codification
-Section 45
-Paragraph 1A
-Subparagraph (a)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482790/220-10-45-1A
Reference 9: http://www.xbrl.org/2003/role/disclosureRef
-Topic 220
-SubTopic 10
-Name Accounting Standards Codification
-Section 45
-Paragraph 1B
-Subparagraph (a)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482790/220-10-45-1B
| Name: |
us-gaap_NetIncomeLossAttributableToNoncontrollingInterest |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:monetaryItemType |
| Balance Type: |
debit |
| Period Type: |
duration |
|
| X |
- DefinitionNumber of operating segments. An operating segment is a component of an enterprise: (a) that engages in business activities from which it may earn revenues and incur expenses (including revenues and expenses relating to transactions with other components of the same enterprise), (b) whose operating results are regularly reviewed by the enterprise's chief operating decision maker to make decisions about resources to be allocated to the segment and assess its performance, and (c) for which discrete financial information is available. An operating segment may engage in business activities for which it has yet to earn revenues, for example, start-up operations may be operating segments before earning revenues. Reference 1: http://www.xbrl.org/2003/role/exampleRef
-Topic 280
-SubTopic 10
-Name Accounting Standards Codification
-Section 55
-Paragraph 49
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482785/280-10-55-49
Reference 2: http://www.xbrl.org/2009/role/commonPracticeRef
-Topic 280
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 18
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482810/280-10-50-18
| Name: |
us-gaap_NumberOfOperatingSegments |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:integerItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionNumber of segments reported by the entity. A reportable segment is a component of an entity for which there is an accounting requirement to report separate financial information on that component in the entity's financial statements. Reference 1: http://www.xbrl.org/2003/role/exampleRef
-Topic 280
-SubTopic 10
-Name Accounting Standards Codification
-Section 55
-Paragraph 47
-Subparagraph (a)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482785/280-10-55-47
Reference 2: http://www.xbrl.org/2003/role/exampleRef
-Topic 280
-SubTopic 10
-Name Accounting Standards Codification
-Section 55
-Paragraph 54
-Subparagraph (e)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482785/280-10-55-54
Reference 3: http://www.xbrl.org/2009/role/commonPracticeRef
-Topic 280
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 18
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482810/280-10-50-18
| Name: |
us-gaap_NumberOfReportableSegments |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:integerItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionAmount of revenue recognized from goods sold, services rendered, insurance premiums, or other activities that constitute an earning process. Includes, but is not limited to, investment and interest income before deduction of interest expense when recognized as a component of revenue, and sales and trading gain (loss). Reference 1: http://www.xbrl.org/2003/role/exampleRef
-Topic 280
-SubTopic 10
-Name Accounting Standards Codification
-Section 55
-Paragraph 48
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482785/280-10-55-48
Reference 2: http://www.xbrl.org/2003/role/disclosureRef
-Topic 280
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 41
-Subparagraph (a)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482810/280-10-50-41
Reference 3: http://www.xbrl.org/2003/role/disclosureRef
-Topic 270
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 1
-Subparagraph (i)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482964/270-10-50-1
Reference 4: http://www.xbrl.org/2003/role/disclosureRef
-Topic 280
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 32
-Subparagraph (ee)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482810/280-10-50-32
Reference 5: http://fasb.org/us-gaap/role/ref/otherTransitionRef
-Topic 280
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 32
-Subparagraph (b)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482810/280-10-50-32
Reference 6: http://fasb.org/us-gaap/role/ref/otherTransitionRef
-Topic 280
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 32
-Subparagraph (a)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482810/280-10-50-32
Reference 7: http://www.xbrl.org/2003/role/disclosureRef
-Topic 235
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.4-08(g)(1)(ii))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480678/235-10-S99-1
Reference 8: http://www.xbrl.org/2003/role/disclosureRef
-Topic 323
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 3
-Subparagraph (c)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147481687/323-10-50-3
Reference 9: http://www.xbrl.org/2003/role/disclosureRef
-Topic 825
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 28
-Subparagraph (f)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482907/825-10-50-28
Reference 10: http://www.xbrl.org/2003/role/disclosureRef
-Topic 470
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1A
-Subparagraph (SX 210.13-01(a)(4)(i))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480097/470-10-S99-1A
Reference 11: http://www.xbrl.org/2009/role/commonPracticeRef
-Topic 470
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1A
-Subparagraph (SX 210.13-01(a)(4)(ii))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480097/470-10-S99-1A
Reference 12: http://www.xbrl.org/2003/role/disclosureRef
-Topic 470
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1A
-Subparagraph (SX 210.13-01(a)(4)(iii)(A))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480097/470-10-S99-1A
Reference 13: http://www.xbrl.org/2003/role/disclosureRef
-Topic 470
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1A
-Subparagraph (SX 210.13-01(a)(4)(iv))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480097/470-10-S99-1A
Reference 14: http://www.xbrl.org/2003/role/disclosureRef
-Topic 470
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1A
-Subparagraph (SX 210.13-01(a)(5))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480097/470-10-S99-1A
Reference 15: http://www.xbrl.org/2003/role/disclosureRef
-Topic 470
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1B
-Subparagraph (SX 210.13-02(a)(4)(i))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480097/470-10-S99-1B
Reference 16: http://www.xbrl.org/2003/role/disclosureRef
-Topic 470
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1B
-Subparagraph (SX 210.13-02(a)(4)(iii)(A))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480097/470-10-S99-1B
Reference 17: http://www.xbrl.org/2003/role/disclosureRef
-Topic 470
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1B
-Subparagraph (SX 210.13-02(a)(4)(iii)(B))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480097/470-10-S99-1B
Reference 18: http://www.xbrl.org/2003/role/disclosureRef
-Topic 470
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1B
-Subparagraph (SX 210.13-02(a)(4)(iv))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480097/470-10-S99-1B
Reference 19: http://www.xbrl.org/2003/role/disclosureRef
-Topic 470
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1B
-Subparagraph (SX 210.13-02(a)(5))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480097/470-10-S99-1B
Reference 20: http://www.xbrl.org/2003/role/disclosureRef
-Topic 280
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 30
-Subparagraph (a)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482810/280-10-50-30
Reference 21: http://www.xbrl.org/2003/role/disclosureRef
-Topic 280
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 42
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482810/280-10-50-42
Reference 22: http://www.xbrl.org/2003/role/disclosureRef
-Topic 280
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 22
-Subparagraph (b)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482810/280-10-50-22
Reference 23: http://www.xbrl.org/2003/role/disclosureRef
-Topic 280
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 40
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482810/280-10-50-40
Reference 24: http://www.xbrl.org/2003/role/disclosureRef
-Topic 280
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 22
-Subparagraph (a)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482810/280-10-50-22
Reference 25: http://www.xbrl.org/2003/role/disclosureRef
-Topic 942
-SubTopic 235
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.9-05(b)(2))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147477314/942-235-S99-1
Reference 26: http://www.xbrl.org/2003/role/disclosureRef
-Topic 220
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 2
-Subparagraph (SX 210.5-03(1))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147483621/220-10-S99-2
| Name: |
us-gaap_Revenues |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:monetaryItemType |
| Balance Type: |
credit |
| Period Type: |
duration |
|
| X |
- DefinitionEstimated period over which an employee is required to provide service in exchange for the equity-based payment award, in 'PnYnMnDTnHnMnS' format, for example, 'P1Y5M13D' represents the reported fact of one year, five months, and thirteen days. Reference 1: http://www.xbrl.org/2003/role/exampleRef
-Topic 718
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 2
-Subparagraph (a)(1)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480429/718-10-50-2
| Name: |
us-gaap_ShareBasedCompensationArrangementByShareBasedPaymentAwardAwardRequisiteServicePeriod1 |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:durationItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- Details
| Name: |
srt_RangeAxis=srt_MinimumMember |
| Namespace Prefix: |
|
| Data Type: |
na |
| Balance Type: |
|
| Period Type: |
|
|
| X |
- Details
| Name: |
srt_ProductOrServiceAxis=alhc_RealizingEquityAccessAndCommunityHealthREACHModelMember |
| Namespace Prefix: |
|
| Data Type: |
na |
| Balance Type: |
|
| Period Type: |
|
|
v3.24.2.u1
Summary of Significant Accounting Policies - Schedule of Earned Revenue (Details) - USD ($)
$ in Thousands |
3 Months Ended |
6 Months Ended |
Jun. 30, 2024 |
Jun. 30, 2023 |
Jun. 30, 2024 |
Jun. 30, 2023 |
| Disaggregation of Revenue [Line Items] |
|
|
|
|
| Earned premiums |
$ 674,094
|
$ 456,877
|
$ 1,295,650
|
$ 891,689
|
| Premium |
|
|
|
|
| Disaggregation of Revenue [Line Items] |
|
|
|
|
| Earned premiums |
673,532
|
424,704
|
1,293,254
|
824,444
|
| Capitation |
|
|
|
|
| Disaggregation of Revenue [Line Items] |
|
|
|
|
| Earned premiums |
$ 562
|
$ 32,173
|
$ 2,396
|
$ 67,245
|
| X |
- DefinitionLine items represent financial concepts included in a table. These concepts are used to disclose reportable information associated with domain members defined in one or many axes to the table. Reference 1: http://www.xbrl.org/2003/role/disclosureRef
-Topic 606
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 5
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147479806/606-10-50-5
Reference 2: http://www.xbrl.org/2003/role/exampleRef
-Topic 606
-SubTopic 10
-Name Accounting Standards Codification
-Section 55
-Paragraph 91
-Subparagraph (a)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147479777/606-10-55-91
Reference 3: http://www.xbrl.org/2003/role/exampleRef
-Topic 606
-SubTopic 10
-Name Accounting Standards Codification
-Section 55
-Paragraph 91
-Subparagraph (b)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147479777/606-10-55-91
Reference 4: http://www.xbrl.org/2003/role/exampleRef
-Topic 606
-SubTopic 10
-Name Accounting Standards Codification
-Section 55
-Paragraph 91
-Subparagraph (c)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147479777/606-10-55-91
Reference 5: http://www.xbrl.org/2003/role/exampleRef
-Topic 606
-SubTopic 10
-Name Accounting Standards Codification
-Section 55
-Paragraph 91
-Subparagraph (d)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147479777/606-10-55-91
Reference 6: http://www.xbrl.org/2003/role/exampleRef
-Topic 606
-SubTopic 10
-Name Accounting Standards Codification
-Section 55
-Paragraph 91
-Subparagraph (e)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147479777/606-10-55-91
Reference 7: http://www.xbrl.org/2003/role/exampleRef
-Topic 606
-SubTopic 10
-Name Accounting Standards Codification
-Section 55
-Paragraph 91
-Subparagraph (f)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147479777/606-10-55-91
Reference 8: http://www.xbrl.org/2003/role/exampleRef
-Topic 606
-SubTopic 10
-Name Accounting Standards Codification
-Section 55
-Paragraph 91
-Subparagraph (g)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147479777/606-10-55-91
| Name: |
us-gaap_DisaggregationOfRevenueLineItems |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:stringItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionAmount, after premiums ceded to other entities and premiums assumed by the entity, of premiums earned. Reference 1: http://www.xbrl.org/2003/role/disclosureRef
-Topic 944
-SubTopic 235
-Name Accounting Standards Codification
-Section S99
-Paragraph 2
-Subparagraph (SX 210.12-17(Column E))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147477965/944-235-S99-2
Reference 2: http://www.xbrl.org/2003/role/disclosureRef
-Topic 944
-SubTopic 605
-Name Accounting Standards Codification
-Section 50
-Paragraph 1
-Subparagraph (c)(3)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147479032/944-605-50-1
Reference 3: http://www.xbrl.org/2003/role/disclosureRef
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.9-04(13)(c))
-SubTopic 220
-Topic 942
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147478524/942-220-S99-1
Reference 4: http://www.xbrl.org/2003/role/disclosureRef
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.7-04(1))
-SubTopic 220
-Topic 944
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147477250/944-220-S99-1
| Name: |
us-gaap_PremiumsEarnedNet |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:monetaryItemType |
| Balance Type: |
credit |
| Period Type: |
duration |
|
| X |
- Details
| Name: |
srt_ProductOrServiceAxis=us-gaap_HealthCarePremiumMember |
| Namespace Prefix: |
|
| Data Type: |
na |
| Balance Type: |
|
| Period Type: |
|
|
| X |
- Details
| Name: |
srt_ProductOrServiceAxis=alhc_HealthCareCapitationMember |
| Namespace Prefix: |
|
| Data Type: |
na |
| Balance Type: |
|
| Period Type: |
|
|
v3.24.2.u1
| X |
- DefinitionLine items represent financial concepts included in a table. These concepts are used to disclose reportable information associated with domain members defined in one or many axes to the table. Reference 1: http://www.xbrl.org/2003/role/disclosureRef
-Topic 842
-SubTopic 20
-Name Accounting Standards Codification
-Section 50
-Paragraph 7A
-Subparagraph (a)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147478964/842-20-50-7A
| Name: |
us-gaap_PropertyPlantAndEquipmentLineItems |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:stringItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionUseful life of long lived, physical assets used in the normal conduct of business and not intended for resale, in 'PnYnMnDTnHnMnS' format, for example, 'P1Y5M13D' represents the reported fact of one year, five months, and thirteen days. Examples include, but not limited to, land, buildings, machinery and equipment, office equipment, furniture and fixtures, and computer equipment.
| Name: |
us-gaap_PropertyPlantAndEquipmentUsefulLife |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:durationItemType |
| Balance Type: |
na |
| Period Type: |
instant |
|
| X |
- Details
| Name: |
us-gaap_PropertyPlantAndEquipmentByTypeAxis=us-gaap_ComputerEquipmentMember |
| Namespace Prefix: |
|
| Data Type: |
na |
| Balance Type: |
|
| Period Type: |
|
|
| X |
- Details
| Name: |
us-gaap_PropertyPlantAndEquipmentByTypeAxis=alhc_OfficeEquipmentAndFurnitureMember |
| Namespace Prefix: |
|
| Data Type: |
na |
| Balance Type: |
|
| Period Type: |
|
|
| X |
- Details
| Name: |
srt_RangeAxis=srt_MinimumMember |
| Namespace Prefix: |
|
| Data Type: |
na |
| Balance Type: |
|
| Period Type: |
|
|
| X |
- Details
| Name: |
srt_RangeAxis=srt_MaximumMember |
| Namespace Prefix: |
|
| Data Type: |
na |
| Balance Type: |
|
| Period Type: |
|
|
| X |
- Details
| Name: |
us-gaap_PropertyPlantAndEquipmentByTypeAxis=us-gaap_SoftwareDevelopmentMember |
| Namespace Prefix: |
|
| Data Type: |
na |
| Balance Type: |
|
| Period Type: |
|
|
| X |
- Details
| Name: |
us-gaap_PropertyPlantAndEquipmentByTypeAxis=us-gaap_LeaseholdImprovementsMember |
| Namespace Prefix: |
|
| Data Type: |
na |
| Balance Type: |
|
| Period Type: |
|
|
v3.24.2.u1
Summary of Significant Accounting Policies - Schedule of Computation of Basic and Diluted Net Loss Per Share (Details) - USD ($)
$ / shares in Units, $ in Thousands |
3 Months Ended |
6 Months Ended |
Jun. 30, 2024 |
Jun. 30, 2023 |
Jun. 30, 2024 |
Jun. 30, 2023 |
| Numerator: |
|
|
|
|
| Net loss |
$ (24,003)
|
$ (28,494)
|
$ (70,578)
|
$ (65,865)
|
| Less: Net (income) loss attributable to noncontrolling interest |
(7)
|
17
|
47
|
104
|
| Net loss attributable to Alignment Healthcare, Inc. |
$ (24,010)
|
$ (28,477)
|
$ (70,531)
|
$ (65,761)
|
| Denominator: |
|
|
|
|
| Total weighted-average common shares outstanding - basic (in shares) |
191,431,917
|
188,496,252
|
190,514,927
|
188,029,447
|
| Total weighted-average common shares outstanding - diluted (in shares) |
191,431,917
|
188,496,252
|
190,514,927
|
188,029,447
|
| Less: Restricted shares of common stock (in shares) |
(540,130)
|
(2,504,792)
|
(566,202)
|
(3,468,795)
|
| Total weighted-average common shares outstanding, net of restricted shares of common stock - basic (in shares) |
190,891,787
|
185,991,460
|
189,948,725
|
184,560,652
|
| Total weighted-average common shares outstanding, net of restricted shares of common stock - diluted (in shares) |
190,891,787
|
185,991,460
|
189,948,725
|
184,560,652
|
| Net loss per share: |
|
|
|
|
| Net loss per share - basic (in dollars per share) |
$ (0.13)
|
$ (0.15)
|
$ (0.37)
|
$ (0.36)
|
| Net loss per share - diluted (in dollars per share) |
$ (0.13)
|
$ (0.15)
|
$ (0.37)
|
$ (0.36)
|
| X |
- DefinitionWeighted Average Number Of Shares Issued, Diluted
| Name: |
alhc_WeightedAverageNumberOfSharesIssuedDiluted |
| Namespace Prefix: |
alhc_ |
| Data Type: |
xbrli:sharesItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- References
+ Details
| Name: |
us-gaap_EarningsPerShareAbstract |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:stringItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionThe amount of net income (loss) for the period per each share of common stock or unit outstanding during the reporting period. Reference 1: http://www.xbrl.org/2003/role/disclosureRef
-Topic 250
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 6
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147483443/250-10-50-6
Reference 2: http://www.xbrl.org/2003/role/exampleRef
-Topic 260
-SubTopic 10
-Name Accounting Standards Codification
-Section 55
-Paragraph 52
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482635/260-10-55-52
Reference 3: http://www.xbrl.org/2003/role/disclosureRef
-Topic 805
-SubTopic 60
-Name Accounting Standards Codification
-Section 65
-Paragraph 1
-Subparagraph (g)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147476176/805-60-65-1
Reference 4: http://www.xbrl.org/2003/role/disclosureRef
-Topic 740
-SubTopic 323
-Name Accounting Standards Codification
-Section 65
-Paragraph 2
-Subparagraph (g)(3)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147478666/740-323-65-2
Reference 5: http://www.xbrl.org/2003/role/disclosureRef
-Topic 250
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 3
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147483443/250-10-50-3
Reference 6: http://www.xbrl.org/2003/role/disclosureRef
-Topic 260
-SubTopic 10
-Name Accounting Standards Codification
-Section 55
-Paragraph 15
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482635/260-10-55-15
Reference 7: http://www.xbrl.org/2003/role/disclosureRef
-Topic 815
-SubTopic 40
-Name Accounting Standards Codification
-Section 65
-Paragraph 1
-Subparagraph (e)(4)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480175/815-40-65-1
Reference 8: http://www.xbrl.org/2003/role/disclosureRef
-Topic 815
-SubTopic 40
-Name Accounting Standards Codification
-Section 65
-Paragraph 1
-Subparagraph (f)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480175/815-40-65-1
Reference 9: http://www.xbrl.org/2003/role/disclosureRef
-Topic 250
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 11
-Subparagraph (a)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147483443/250-10-50-11
Reference 10: http://www.xbrl.org/2003/role/disclosureRef
-Topic 250
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 11
-Subparagraph (b)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147483443/250-10-50-11
Reference 11: http://www.xbrl.org/2003/role/disclosureRef
-Topic 250
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 7
-Subparagraph (a)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147483443/250-10-50-7
Reference 12: http://www.xbrl.org/2003/role/disclosureRef
-Topic 260
-SubTopic 10
-Name Accounting Standards Codification
-Section 45
-Paragraph 2
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482689/260-10-45-2
Reference 13: http://www.xbrl.org/2003/role/disclosureRef
-Topic 260
-SubTopic 10
-Name Accounting Standards Codification
-Section 45
-Paragraph 60B
-Subparagraph (d)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482689/260-10-45-60B
Reference 14: http://www.xbrl.org/2003/role/disclosureRef
-Topic 250
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 4
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147483443/250-10-50-4
Reference 15: http://www.xbrl.org/2003/role/disclosureRef
-Topic 260
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 1
-Subparagraph (a)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482662/260-10-50-1
Reference 16: http://www.xbrl.org/2003/role/disclosureRef
-Topic 260
-SubTopic 10
-Name Accounting Standards Codification
-Section 45
-Paragraph 10
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482689/260-10-45-10
Reference 17: http://www.xbrl.org/2003/role/disclosureRef
-Topic 220
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 2
-Subparagraph (SX 210.5-03(25))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147483621/220-10-S99-2
Reference 18: http://www.xbrl.org/2003/role/disclosureRef
-Topic 942
-SubTopic 220
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.9-04(27))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147478524/942-220-S99-1
Reference 19: http://www.xbrl.org/2003/role/disclosureRef
-Topic 944
-SubTopic 220
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.7-04(23))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147477250/944-220-S99-1
Reference 20: http://www.xbrl.org/2003/role/disclosureRef
-Topic 260
-SubTopic 10
-Name Accounting Standards Codification
-Section 45
-Paragraph 7
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482689/260-10-45-7
| Name: |
us-gaap_EarningsPerShareBasic |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
dtr-types:perShareItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionThe amount of net income (loss) for the period available to each share of common stock or common unit outstanding during the reporting period and to each share or unit that would have been outstanding assuming the issuance of common shares or units for all dilutive potential common shares or units outstanding during the reporting period. Reference 1: http://www.xbrl.org/2003/role/disclosureRef
-Topic 250
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 6
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147483443/250-10-50-6
Reference 2: http://www.xbrl.org/2003/role/exampleRef
-Topic 260
-SubTopic 10
-Name Accounting Standards Codification
-Section 55
-Paragraph 52
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482635/260-10-55-52
Reference 3: http://www.xbrl.org/2003/role/disclosureRef
-Topic 805
-SubTopic 60
-Name Accounting Standards Codification
-Section 65
-Paragraph 1
-Subparagraph (g)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147476176/805-60-65-1
Reference 4: http://www.xbrl.org/2003/role/disclosureRef
-Topic 740
-SubTopic 323
-Name Accounting Standards Codification
-Section 65
-Paragraph 2
-Subparagraph (g)(3)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147478666/740-323-65-2
Reference 5: http://www.xbrl.org/2003/role/disclosureRef
-Topic 250
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 3
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147483443/250-10-50-3
Reference 6: http://www.xbrl.org/2003/role/disclosureRef
-Topic 260
-SubTopic 10
-Name Accounting Standards Codification
-Section 55
-Paragraph 15
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482635/260-10-55-15
Reference 7: http://www.xbrl.org/2003/role/disclosureRef
-Topic 815
-SubTopic 40
-Name Accounting Standards Codification
-Section 65
-Paragraph 1
-Subparagraph (e)(4)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480175/815-40-65-1
Reference 8: http://www.xbrl.org/2003/role/disclosureRef
-Topic 815
-SubTopic 40
-Name Accounting Standards Codification
-Section 65
-Paragraph 1
-Subparagraph (f)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480175/815-40-65-1
Reference 9: http://www.xbrl.org/2003/role/disclosureRef
-Topic 250
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 11
-Subparagraph (a)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147483443/250-10-50-11
Reference 10: http://www.xbrl.org/2003/role/disclosureRef
-Topic 250
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 11
-Subparagraph (b)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147483443/250-10-50-11
Reference 11: http://www.xbrl.org/2003/role/disclosureRef
-Topic 250
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 7
-Subparagraph (a)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147483443/250-10-50-7
Reference 12: http://www.xbrl.org/2003/role/disclosureRef
-Topic 260
-SubTopic 10
-Name Accounting Standards Codification
-Section 45
-Paragraph 2
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482689/260-10-45-2
Reference 13: http://www.xbrl.org/2003/role/disclosureRef
-Topic 260
-SubTopic 10
-Name Accounting Standards Codification
-Section 45
-Paragraph 60B
-Subparagraph (d)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482689/260-10-45-60B
Reference 14: http://www.xbrl.org/2003/role/disclosureRef
-Topic 250
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 4
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147483443/250-10-50-4
Reference 15: http://www.xbrl.org/2003/role/disclosureRef
-Topic 260
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 1
-Subparagraph (a)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482662/260-10-50-1
Reference 16: http://www.xbrl.org/2003/role/disclosureRef
-Topic 220
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 2
-Subparagraph (SX 210.5-03(25))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147483621/220-10-S99-2
Reference 17: http://www.xbrl.org/2003/role/disclosureRef
-Topic 942
-SubTopic 220
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.9-04(27))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147478524/942-220-S99-1
Reference 18: http://www.xbrl.org/2003/role/disclosureRef
-Topic 944
-SubTopic 220
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.7-04(23))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147477250/944-220-S99-1
Reference 19: http://www.xbrl.org/2003/role/disclosureRef
-Topic 260
-SubTopic 10
-Name Accounting Standards Codification
-Section 45
-Paragraph 7
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482689/260-10-45-7
| Name: |
us-gaap_EarningsPerShareDiluted |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
dtr-types:perShareItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionThe portion of profit or loss for the period, net of income taxes, which is attributable to the parent. Reference 1: http://www.xbrl.org/2003/role/disclosureRef
-Topic 250
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 6
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147483443/250-10-50-6
Reference 2: http://www.xbrl.org/2003/role/disclosureRef
-Topic 250
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 9
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147483443/250-10-50-9
Reference 3: http://www.xbrl.org/2003/role/disclosureRef
-Topic 805
-SubTopic 60
-Name Accounting Standards Codification
-Section 65
-Paragraph 1
-Subparagraph (g)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147476176/805-60-65-1
Reference 4: http://www.xbrl.org/2003/role/disclosureRef
-Topic 740
-SubTopic 323
-Name Accounting Standards Codification
-Section 65
-Paragraph 2
-Subparagraph (g)(3)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147478666/740-323-65-2
Reference 5: http://fasb.org/us-gaap/role/ref/legacyRef
-Topic 220
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 2
-Subparagraph (SX 210.5-03(20))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147483621/220-10-S99-2
Reference 6: http://www.xbrl.org/2003/role/disclosureRef
-Topic 235
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.4-08(g)(1)(ii))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480678/235-10-S99-1
Reference 7: http://www.xbrl.org/2003/role/disclosureRef
-Topic 323
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 3
-Subparagraph (c)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147481687/323-10-50-3
Reference 8: http://www.xbrl.org/2003/role/disclosureRef
-Topic 825
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 28
-Subparagraph (f)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482907/825-10-50-28
Reference 9: http://www.xbrl.org/2003/role/disclosureRef
-Topic 220
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 6
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482765/220-10-50-6
Reference 10: http://www.xbrl.org/2003/role/disclosureRef
-Topic 250
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 3
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147483443/250-10-50-3
Reference 11: http://www.xbrl.org/2003/role/disclosureRef
-Topic 250
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 1
-Subparagraph (b)(2)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147483443/250-10-50-1
Reference 12: http://www.xbrl.org/2003/role/disclosureRef
-Topic 815
-SubTopic 40
-Name Accounting Standards Codification
-Section 65
-Paragraph 1
-Subparagraph (f)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480175/815-40-65-1
Reference 13: http://www.xbrl.org/2003/role/disclosureRef
-Topic 250
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 8
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147483443/250-10-50-8
Reference 14: http://www.xbrl.org/2003/role/disclosureRef
-Topic 250
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 11
-Subparagraph (a)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147483443/250-10-50-11
Reference 15: http://www.xbrl.org/2003/role/disclosureRef
-Topic 250
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 11
-Subparagraph (b)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147483443/250-10-50-11
Reference 16: http://www.xbrl.org/2003/role/disclosureRef
-Topic 250
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 4
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147483443/250-10-50-4
Reference 17: http://www.xbrl.org/2003/role/exampleRef
-Topic 946
-SubTopic 830
-Name Accounting Standards Codification
-Section 55
-Paragraph 10
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147479168/946-830-55-10
Reference 18: http://www.xbrl.org/2003/role/disclosureRef
-Topic 946
-SubTopic 220
-Name Accounting Standards Codification
-Section 45
-Paragraph 7
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147479105/946-220-45-7
Reference 19: http://www.xbrl.org/2003/role/disclosureRef
-Topic 944
-SubTopic 220
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.7-04(18))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147477250/944-220-S99-1
Reference 20: http://www.xbrl.org/2003/role/disclosureRef
-Topic 946
-SubTopic 220
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.6-07(9))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147479134/946-220-S99-1
Reference 21: http://www.xbrl.org/2003/role/disclosureRef
-Topic 946
-SubTopic 220
-Name Accounting Standards Codification
-Section S99
-Paragraph 3
-Subparagraph (SX 210.6-09(1)(d))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147479134/946-220-S99-3
Reference 22: http://www.xbrl.org/2003/role/disclosureRef
-Topic 470
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1A
-Subparagraph (SX 210.13-01(a)(4)(i))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480097/470-10-S99-1A
Reference 23: http://www.xbrl.org/2009/role/commonPracticeRef
-Topic 470
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1A
-Subparagraph (SX 210.13-01(a)(4)(ii))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480097/470-10-S99-1A
Reference 24: http://www.xbrl.org/2003/role/disclosureRef
-Topic 470
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1A
-Subparagraph (SX 210.13-01(a)(4)(iii)(A))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480097/470-10-S99-1A
Reference 25: http://www.xbrl.org/2003/role/disclosureRef
-Topic 470
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1A
-Subparagraph (SX 210.13-01(a)(4)(iv))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480097/470-10-S99-1A
Reference 26: http://www.xbrl.org/2003/role/disclosureRef
-Topic 470
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1A
-Subparagraph (SX 210.13-01(a)(5))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480097/470-10-S99-1A
Reference 27: http://www.xbrl.org/2003/role/disclosureRef
-Topic 470
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1B
-Subparagraph (SX 210.13-02(a)(4)(i))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480097/470-10-S99-1B
Reference 28: http://www.xbrl.org/2003/role/disclosureRef
-Topic 470
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1B
-Subparagraph (SX 210.13-02(a)(4)(iii)(A))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480097/470-10-S99-1B
Reference 29: http://www.xbrl.org/2003/role/disclosureRef
-Topic 470
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1B
-Subparagraph (SX 210.13-02(a)(4)(iii)(B))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480097/470-10-S99-1B
Reference 30: http://www.xbrl.org/2003/role/disclosureRef
-Topic 470
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1B
-Subparagraph (SX 210.13-02(a)(4)(iv))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480097/470-10-S99-1B
Reference 31: http://www.xbrl.org/2003/role/disclosureRef
-Topic 470
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1B
-Subparagraph (SX 210.13-02(a)(5))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480097/470-10-S99-1B
Reference 32: http://www.xbrl.org/2003/role/disclosureRef
-Topic 260
-SubTopic 10
-Name Accounting Standards Codification
-Section 45
-Paragraph 60B
-Subparagraph (a)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482689/260-10-45-60B
Reference 33: http://www.xbrl.org/2003/role/disclosureRef
-Topic 205
-SubTopic 20
-Name Accounting Standards Codification
-Section 50
-Paragraph 7
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147483499/205-20-50-7
Reference 34: http://fasb.org/us-gaap/role/ref/legacyRef
-Topic 230
-SubTopic 10
-Name Accounting Standards Codification
-Section 45
-Paragraph 28
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482740/230-10-45-28
Reference 35: http://www.xbrl.org/2003/role/disclosureRef
-Topic 220
-SubTopic 10
-Name Accounting Standards Codification
-Section 45
-Paragraph 1A
-Subparagraph (a)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482790/220-10-45-1A
Reference 36: http://www.xbrl.org/2003/role/disclosureRef
-Topic 220
-SubTopic 10
-Name Accounting Standards Codification
-Section 45
-Paragraph 1B
-Subparagraph (a)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482790/220-10-45-1B
Reference 37: http://fasb.org/us-gaap/role/ref/legacyRef
-Topic 942
-SubTopic 220
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.9-04(22))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147478524/942-220-S99-1
| Name: |
us-gaap_NetIncomeLoss |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:monetaryItemType |
| Balance Type: |
credit |
| Period Type: |
duration |
|
| X |
- DefinitionAmount of Net Income (Loss) attributable to noncontrolling interest. Reference 1: http://www.xbrl.org/2003/role/disclosureRef
-Topic 250
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 6
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147483443/250-10-50-6
Reference 2: http://www.xbrl.org/2003/role/disclosureRef
-Topic 250
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 9
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147483443/250-10-50-9
Reference 3: http://www.xbrl.org/2003/role/disclosureRef
-Topic 250
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 8
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147483443/250-10-50-8
Reference 4: http://www.xbrl.org/2003/role/disclosureRef
-Topic 944
-SubTopic 220
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.7-04(17))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147477250/944-220-S99-1
Reference 5: http://www.xbrl.org/2009/role/commonPracticeRef
-Topic 220
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 6
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482765/220-10-50-6
Reference 6: http://fasb.org/us-gaap/role/ref/legacyRef
-Topic 810
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 1A
-Subparagraph (a)(2)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147481203/810-10-50-1A
Reference 7: http://fasb.org/us-gaap/role/ref/legacyRef
-Name Accounting Standards Codification
-Topic 810
-SubTopic 10
-Section 55
-Paragraph 4J
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147481175/810-10-55-4J
Reference 8: http://www.xbrl.org/2003/role/disclosureRef
-Topic 220
-SubTopic 10
-Name Accounting Standards Codification
-Section 45
-Paragraph 1A
-Subparagraph (a)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482790/220-10-45-1A
Reference 9: http://www.xbrl.org/2003/role/disclosureRef
-Topic 220
-SubTopic 10
-Name Accounting Standards Codification
-Section 45
-Paragraph 1B
-Subparagraph (a)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482790/220-10-45-1B
| Name: |
us-gaap_NetIncomeLossAttributableToNoncontrollingInterest |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:monetaryItemType |
| Balance Type: |
debit |
| Period Type: |
duration |
|
| X |
- References
+ Details
| Name: |
us-gaap_NetIncomeLossAvailableToCommonStockholdersBasicAbstract |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:stringItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionThe consolidated profit or loss for the period, net of income taxes, including the portion attributable to the noncontrolling interest. Reference 1: http://www.xbrl.org/2003/role/disclosureRef
-Topic 250
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 6
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147483443/250-10-50-6
Reference 2: http://www.xbrl.org/2003/role/disclosureRef
-Topic 250
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 9
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147483443/250-10-50-9
Reference 3: http://www.xbrl.org/2003/role/disclosureRef
-Topic 805
-SubTopic 60
-Name Accounting Standards Codification
-Section 65
-Paragraph 1
-Subparagraph (g)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147476176/805-60-65-1
Reference 4: http://www.xbrl.org/2003/role/disclosureRef
-Topic 740
-SubTopic 323
-Name Accounting Standards Codification
-Section 65
-Paragraph 2
-Subparagraph (g)(3)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147478666/740-323-65-2
Reference 5: http://www.xbrl.org/2003/role/disclosureRef
-Topic 235
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.4-08(g)(1)(ii))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480678/235-10-S99-1
Reference 6: http://www.xbrl.org/2003/role/disclosureRef
-Topic 323
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 3
-Subparagraph (c)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147481687/323-10-50-3
Reference 7: http://www.xbrl.org/2003/role/disclosureRef
-Topic 825
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 28
-Subparagraph (f)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482907/825-10-50-28
Reference 8: http://www.xbrl.org/2003/role/disclosureRef
-Topic 250
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 1
-Subparagraph (b)(2)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147483443/250-10-50-1
Reference 9: http://www.xbrl.org/2003/role/disclosureRef
-Topic 815
-SubTopic 40
-Name Accounting Standards Codification
-Section 65
-Paragraph 1
-Subparagraph (f)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480175/815-40-65-1
Reference 10: http://www.xbrl.org/2003/role/disclosureRef
-Topic 250
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 8
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147483443/250-10-50-8
Reference 11: http://www.xbrl.org/2003/role/exampleRef
-Topic 946
-SubTopic 830
-Name Accounting Standards Codification
-Section 55
-Paragraph 11
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147479168/946-830-55-11
Reference 12: http://www.xbrl.org/2003/role/disclosureRef
-Topic 946
-SubTopic 205
-Name Accounting Standards Codification
-Section 45
-Paragraph 3
-Subparagraph (a)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147478009/946-205-45-3
Reference 13: http://www.xbrl.org/2003/role/disclosureRef
-Topic 946
-SubTopic 220
-Name Accounting Standards Codification
-Section 45
-Paragraph 7
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147479105/946-220-45-7
Reference 14: http://www.xbrl.org/2003/role/disclosureRef
-Topic 944
-SubTopic 220
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.7-04(16))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147477250/944-220-S99-1
Reference 15: http://www.xbrl.org/2003/role/disclosureRef
-Topic 946
-SubTopic 220
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.6-07(9))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147479134/946-220-S99-1
Reference 16: http://www.xbrl.org/2003/role/disclosureRef
-Topic 946
-SubTopic 220
-Name Accounting Standards Codification
-Section S99
-Paragraph 3
-Subparagraph (SX 210.6-09(1)(d))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147479134/946-220-S99-3
Reference 17: http://www.xbrl.org/2003/role/disclosureRef
-Topic 810
-SubTopic 10
-Name Accounting Standards Codification
-Section 45
-Paragraph 19
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147481231/810-10-45-19
Reference 18: http://www.xbrl.org/2009/role/commonPracticeRef
-Topic 220
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 6
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482765/220-10-50-6
Reference 19: http://www.xbrl.org/2003/role/disclosureRef
-Topic 470
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1A
-Subparagraph (SX 210.13-01(a)(4)(i))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480097/470-10-S99-1A
Reference 20: http://www.xbrl.org/2009/role/commonPracticeRef
-Topic 470
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1A
-Subparagraph (SX 210.13-01(a)(4)(ii))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480097/470-10-S99-1A
Reference 21: http://www.xbrl.org/2003/role/disclosureRef
-Topic 470
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1A
-Subparagraph (SX 210.13-01(a)(4)(iii)(A))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480097/470-10-S99-1A
Reference 22: http://www.xbrl.org/2003/role/disclosureRef
-Topic 470
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1A
-Subparagraph (SX 210.13-01(a)(4)(iv))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480097/470-10-S99-1A
Reference 23: http://www.xbrl.org/2003/role/disclosureRef
-Topic 470
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1A
-Subparagraph (SX 210.13-01(a)(5))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480097/470-10-S99-1A
Reference 24: http://www.xbrl.org/2003/role/disclosureRef
-Topic 470
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1B
-Subparagraph (SX 210.13-02(a)(4)(i))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480097/470-10-S99-1B
Reference 25: http://www.xbrl.org/2003/role/disclosureRef
-Topic 470
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1B
-Subparagraph (SX 210.13-02(a)(4)(iii)(A))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480097/470-10-S99-1B
Reference 26: http://www.xbrl.org/2003/role/disclosureRef
-Topic 470
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1B
-Subparagraph (SX 210.13-02(a)(4)(iii)(B))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480097/470-10-S99-1B
Reference 27: http://www.xbrl.org/2003/role/disclosureRef
-Topic 470
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1B
-Subparagraph (SX 210.13-02(a)(4)(iv))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480097/470-10-S99-1B
Reference 28: http://www.xbrl.org/2003/role/disclosureRef
-Topic 470
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1B
-Subparagraph (SX 210.13-02(a)(5))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480097/470-10-S99-1B
Reference 29: http://www.xbrl.org/2003/role/disclosureRef
-Topic 942
-SubTopic 235
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.9-05(b)(2))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147477314/942-235-S99-1
Reference 30: http://www.xbrl.org/2003/role/disclosureRef
-Topic 205
-SubTopic 20
-Name Accounting Standards Codification
-Section 50
-Paragraph 7
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147483499/205-20-50-7
Reference 31: http://www.xbrl.org/2003/role/exampleRef
-Topic 810
-SubTopic 10
-Name Accounting Standards Codification
-Section 55
-Paragraph 4J
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147481175/810-10-55-4J
Reference 32: http://www.xbrl.org/2003/role/exampleRef
-Topic 810
-SubTopic 10
-Name Accounting Standards Codification
-Section 55
-Paragraph 4K
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147481175/810-10-55-4K
Reference 33: http://www.xbrl.org/2003/role/disclosureRef
-Topic 220
-SubTopic 10
-Name Accounting Standards Codification
-Section 45
-Paragraph 1A
-Subparagraph (a)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482790/220-10-45-1A
Reference 34: http://www.xbrl.org/2003/role/disclosureRef
-Topic 220
-SubTopic 10
-Name Accounting Standards Codification
-Section 45
-Paragraph 1B
-Subparagraph (a)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482790/220-10-45-1B
Reference 35: http://www.xbrl.org/2003/role/disclosureRef
-Topic 230
-SubTopic 10
-Name Accounting Standards Codification
-Section 45
-Paragraph 2
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482740/230-10-45-2
Reference 36: http://www.xbrl.org/2003/role/disclosureRef
-Topic 810
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 1A
-Subparagraph (a)(1)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147481203/810-10-50-1A
Reference 37: http://www.xbrl.org/2003/role/disclosureRef
-Topic 810
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 1A
-Subparagraph (c)(1)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147481203/810-10-50-1A
| Name: |
us-gaap_ProfitLoss |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:monetaryItemType |
| Balance Type: |
credit |
| Period Type: |
duration |
|
| X |
- DefinitionThe average number of shares or units issued and outstanding that are used in calculating diluted EPS or earnings per unit (EPU), determined based on the timing of issuance of shares or units in the period. Reference 1: http://www.xbrl.org/2003/role/disclosureRef
-Topic 260
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 1
-Subparagraph (a)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482662/260-10-50-1
Reference 2: http://www.xbrl.org/2003/role/disclosureRef
-Topic 260
-SubTopic 10
-Name Accounting Standards Codification
-Section 45
-Paragraph 16
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482689/260-10-45-16
| Name: |
us-gaap_WeightedAverageNumberOfDilutedSharesOutstanding |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:sharesItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionThis element represents the weighted average total number of shares issued throughout the period including the first (beginning balance outstanding) and last (ending balance outstanding) day of the period before considering any reductions (for instance, shares held in treasury) to arrive at the weighted average number of shares outstanding. Weighted average relates to the portion of time within a reporting period that common shares have been issued and outstanding to the total time in that period. Such concept is used in determining the weighted average number of shares outstanding for purposes of calculating earnings per share (basic). Reference 1: http://fasb.org/us-gaap/role/ref/legacyRef
-Name Accounting Standards Codification
-Topic 260
-SubTopic 10
-Section 45
-Paragraph 13
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482689/260-10-45-13
Reference 2: http://fasb.org/us-gaap/role/ref/legacyRef
-Name Accounting Standards Codification
-Topic 260
-SubTopic 10
-Section 45
-Paragraph 10
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482689/260-10-45-10
| Name: |
us-gaap_WeightedAverageNumberOfSharesIssuedBasic |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:sharesItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionNumber of [basic] shares or units, after adjustment for contingently issuable shares or units and other shares or units not deemed outstanding, determined by relating the portion of time within a reporting period that common shares or units have been outstanding to the total time in that period. Reference 1: http://www.xbrl.org/2003/role/disclosureRef
-Topic 260
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 1
-Subparagraph (a)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482662/260-10-50-1
Reference 2: http://www.xbrl.org/2003/role/disclosureRef
-Topic 260
-SubTopic 10
-Name Accounting Standards Codification
-Section 45
-Paragraph 10
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482689/260-10-45-10
| Name: |
us-gaap_WeightedAverageNumberOfSharesOutstandingBasic |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:sharesItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- References
+ Details
| Name: |
us-gaap_WeightedAverageNumberOfSharesOutstandingDilutedDisclosureItemsAbstract |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:stringItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionNumber of shares of restricted stock determined by relating the portion of time within a reporting period that restricted shares have been outstanding to the total time in that period. Restricted shares are subject to sales, contractual, regulatory or other restrictions that prevent or inhibit the holder from freely disposing of them before the restriction ends. Reference 1: http://fasb.org/us-gaap/role/ref/legacyRef
-Name Accounting Standards Codification
-Topic 260
-SubTopic 10
-Section 45
-Paragraph 13
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482689/260-10-45-13
| Name: |
us-gaap_WeightedAverageNumberOfSharesRestrictedStock |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:sharesItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
v3.24.2.u1
Summary of Significant Accounting Policies - Schedule of Computation of Diluted Net Loss Per Share (Details) - shares
|
6 Months Ended |
Jun. 30, 2024 |
Jun. 30, 2023 |
| Antidilutive securities excluded from computation of earnings per share (in shares) |
31,146,067
|
20,712,122
|
| Stock options |
|
|
| Antidilutive securities excluded from computation of earnings per share (in shares) |
8,949,589
|
10,566,529
|
| Restricted stock units |
|
|
| Antidilutive securities excluded from computation of earnings per share (in shares) |
22,196,478
|
10,145,593
|
| X |
- DefinitionSecurities (including those issuable pursuant to contingent stock agreements) that could potentially dilute basic earnings per share (EPS) or earnings per unit (EPU) in the future that were not included in the computation of diluted EPS or EPU because to do so would increase EPS or EPU amounts or decrease loss per share or unit amounts for the period presented. Reference 1: http://www.xbrl.org/2003/role/disclosureRef
-Topic 260
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 1
-Subparagraph (c)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482662/260-10-50-1
| Name: |
us-gaap_AntidilutiveSecuritiesExcludedFromComputationOfEarningsPerShareAmount |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:sharesItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- Details
| Name: |
us-gaap_AwardTypeAxis=us-gaap_StockOptionMember |
| Namespace Prefix: |
|
| Data Type: |
na |
| Balance Type: |
|
| Period Type: |
|
|
| X |
- Details
| Name: |
us-gaap_AwardTypeAxis=us-gaap_RestrictedStockUnitsRSUMember |
| Namespace Prefix: |
|
| Data Type: |
na |
| Balance Type: |
|
| Period Type: |
|
|
v3.24.2.u1
Fair Value - Schedule of Carrying Value and Fair Value of Financial Instruments (Details) - USD ($)
|
Jun. 30, 2024 |
Dec. 31, 2023 |
| Fair Value, Assets and Liabilities Measured on Recurring and Nonrecurring Basis [Line Items] |
|
|
| Assets, fair value disclosure |
$ 46,964,000
|
$ 119,092,000
|
| Level 1 |
|
|
| Fair Value, Assets and Liabilities Measured on Recurring and Nonrecurring Basis [Line Items] |
|
|
| Assets, fair value disclosure |
44,577,000
|
117,310,000
|
| Level 2 |
|
|
| Fair Value, Assets and Liabilities Measured on Recurring and Nonrecurring Basis [Line Items] |
|
|
| Assets, fair value disclosure |
2,336,000
|
1,755,000
|
| Level 3 |
|
|
| Fair Value, Assets and Liabilities Measured on Recurring and Nonrecurring Basis [Line Items] |
|
|
| Assets, fair value disclosure |
0
|
0
|
| U.S. Treasury bills |
|
|
| Fair Value, Assets and Liabilities Measured on Recurring and Nonrecurring Basis [Line Items] |
|
|
| U.S. Treasury bills |
44,628,000
|
117,337,000
|
| U.S. Treasury bills | Level 1 |
|
|
| Fair Value, Assets and Liabilities Measured on Recurring and Nonrecurring Basis [Line Items] |
|
|
| U.S. Treasury bills |
44,577,000
|
117,310,000
|
| U.S. Treasury bills | Level 2 |
|
|
| Fair Value, Assets and Liabilities Measured on Recurring and Nonrecurring Basis [Line Items] |
|
|
| U.S. Treasury bills |
0
|
0
|
| U.S. Treasury bills | Level 3 |
|
|
| Fair Value, Assets and Liabilities Measured on Recurring and Nonrecurring Basis [Line Items] |
|
|
| U.S. Treasury bills |
0
|
0
|
| Certificate of deposits |
|
|
| Fair Value, Assets and Liabilities Measured on Recurring and Nonrecurring Basis [Line Items] |
|
|
| Certificate of deposits |
2,336,000
|
1,755,000
|
| Certificate of deposits | Level 1 |
|
|
| Fair Value, Assets and Liabilities Measured on Recurring and Nonrecurring Basis [Line Items] |
|
|
| Certificate of deposits |
0
|
0
|
| Certificate of deposits | Level 2 |
|
|
| Fair Value, Assets and Liabilities Measured on Recurring and Nonrecurring Basis [Line Items] |
|
|
| Certificate of deposits |
2,336,000
|
1,755,000
|
| Certificate of deposits | Level 3 |
|
|
| Fair Value, Assets and Liabilities Measured on Recurring and Nonrecurring Basis [Line Items] |
|
|
| Certificate of deposits |
$ 0
|
$ 0
|
| X |
- DefinitionFair value portion of asset recognized for present right to economic benefit. Reference 1: http://www.xbrl.org/2003/role/exampleRef
-Topic 820
-SubTopic 10
-Name Accounting Standards Codification
-Section 55
-Paragraph 100
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482078/820-10-55-100
Reference 2: http://www.xbrl.org/2003/role/disclosureRef
-Topic 820
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 2
-Subparagraph (b)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482106/820-10-50-2
Reference 3: http://www.xbrl.org/2003/role/disclosureRef
-Topic 820
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 2
-Subparagraph (a)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482106/820-10-50-2
| Name: |
us-gaap_AssetsFairValueDisclosure |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:monetaryItemType |
| Balance Type: |
debit |
| Period Type: |
instant |
|
| X |
- DefinitionAmount, after allowance for credit loss, of investment in debt security measured at amortized cost (held-to-maturity). Reference 1: http://www.xbrl.org/2003/role/disclosureRef
-Topic 320
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 5
-Subparagraph (d)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147481800/320-10-50-5
Reference 2: http://www.xbrl.org/2003/role/disclosureRef
-Topic 320
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 5
-Subparagraph (f)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147481800/320-10-50-5
Reference 3: http://www.xbrl.org/2003/role/disclosureRef
-Topic 942
-SubTopic 210
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.9-03(6))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147478546/942-210-S99-1
Reference 4: http://www.xbrl.org/2003/role/disclosureRef
-Topic 320
-SubTopic 10
-Name Accounting Standards Codification
-Section 45
-Paragraph 1
-Subparagraph (b)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147481830/320-10-45-1
| Name: |
us-gaap_DebtSecuritiesHeldToMaturityAmortizedCostAfterAllowanceForCreditLoss |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:monetaryItemType |
| Balance Type: |
debit |
| Period Type: |
instant |
|
| X |
- DefinitionLine items represent financial concepts included in a table. These concepts are used to disclose reportable information associated with domain members defined in one or many axes to the table. Reference 1: http://www.xbrl.org/2003/role/exampleRef
-Topic 820
-SubTopic 10
-Name Accounting Standards Codification
-Section 55
-Paragraph 100
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482078/820-10-55-100
Reference 2: http://www.xbrl.org/2003/role/disclosureRef
-Topic 820
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 2
-Subparagraph (b)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482106/820-10-50-2
Reference 3: http://www.xbrl.org/2003/role/disclosureRef
-Topic 820
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 2
-Subparagraph (a)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482106/820-10-50-2
Reference 4: http://www.xbrl.org/2003/role/disclosureRef
-Topic 820
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 3
-Subparagraph (a)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482106/820-10-50-3
| Name: |
us-gaap_FairValueAssetsAndLiabilitiesMeasuredOnRecurringAndNonrecurringBasisLineItems |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:stringItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionThe aggregate value of all restricted investments. Reference 1: http://www.xbrl.org/2003/role/disclosureRef
-Topic 946
-SubTopic 320
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.12-12(Column C)(Footnote 8)(c))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147477271/946-320-S99-1
Reference 2: http://www.xbrl.org/2003/role/disclosureRef
-Topic 946
-SubTopic 320
-Name Accounting Standards Codification
-Section S99
-Paragraph 3
-Subparagraph (SX 210.12-12B(Column C)(Footnote 11)(c))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147477271/946-320-S99-3
Reference 3: http://www.xbrl.org/2003/role/disclosureRef
-Topic 946
-SubTopic 320
-Name Accounting Standards Codification
-Section S99
-Paragraph 6
-Subparagraph (SX 210.12-14(Column F)(Footnote 5)(a))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147477271/946-320-S99-6
Reference 4: http://www.xbrl.org/2003/role/disclosureRef
-Topic 954
-SubTopic 210
-Name Accounting Standards Codification
-Section 45
-Paragraph 4
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147477220/954-210-45-4
Reference 5: http://www.xbrl.org/2003/role/disclosureRef
-Topic 954
-SubTopic 210
-Name Accounting Standards Codification
-Section 50
-Paragraph 2
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147478600/954-210-50-2
| Name: |
us-gaap_RestrictedInvestmentsAtFairValue |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:monetaryItemType |
| Balance Type: |
debit |
| Period Type: |
instant |
|
| X |
- Details
| Name: |
us-gaap_FinancialInstrumentAxis=us-gaap_USTreasurySecuritiesMember |
| Namespace Prefix: |
|
| Data Type: |
na |
| Balance Type: |
|
| Period Type: |
|
|
| X |
- Details
| Name: |
us-gaap_FinancialInstrumentAxis=us-gaap_CertificatesOfDepositMember |
| Namespace Prefix: |
|
| Data Type: |
na |
| Balance Type: |
|
| Period Type: |
|
|
v3.24.2.u1
Fair Value - Additional Information (Details) - USD ($)
|
6 Months Ended |
12 Months Ended |
Jun. 30, 2024 |
Dec. 31, 2023 |
| Fair Value, Balance Sheet Grouping, Financial Statement Captions [Line Items] |
|
|
| Asset impairment charges |
$ 0
|
$ 0
|
| US Treasury Bill Securities |
|
|
| Fair Value, Balance Sheet Grouping, Financial Statement Captions [Line Items] |
|
|
| Gross unrecognized loss |
0
|
|
| Restricted investments |
1,375,000
|
1,423,000
|
| Certificate of deposits |
|
|
| Fair Value, Balance Sheet Grouping, Financial Statement Captions [Line Items] |
|
|
| Restricted investments |
2,336,000
|
1,755,000
|
| Short-Term Investments | US Treasury Bill Securities |
|
|
| Fair Value, Balance Sheet Grouping, Financial Statement Captions [Line Items] |
|
|
| Treasury securities investments |
24,651,000
|
115,914,000
|
| Cash and Cash Equivalents | US Treasury Bill Securities |
|
|
| Fair Value, Balance Sheet Grouping, Financial Statement Captions [Line Items] |
|
|
| Treasury securities investments |
$ 18,602,000
|
$ 22,232,000
|
| X |
- DefinitionAmount of write-down of assets recognized in the income statement. Includes, but is not limited to, losses from tangible assets, intangible assets and goodwill. Reference 1: http://fasb.org/us-gaap/role/ref/legacyRef
-Name Accounting Standards Codification
-Section 45
-Paragraph 28
-Subparagraph (b)
-SubTopic 10
-Topic 230
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482740/230-10-45-28
Reference 2: http://fasb.org/us-gaap/role/ref/legacyRef
-Name Accounting Standards Codification
-Topic 360
-SubTopic 10
-Section 45
-Paragraph 4
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482130/360-10-45-4
| Name: |
us-gaap_AssetImpairmentCharges |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:monetaryItemType |
| Balance Type: |
debit |
| Period Type: |
duration |
|
| X |
- DefinitionAmount, after allowance for credit loss, of investment in debt security measured at amortized cost (held-to-maturity), classified as current. Reference 1: http://www.xbrl.org/2009/role/commonPracticeRef
-Topic 320
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 5
-Subparagraph (d)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147481800/320-10-50-5
Reference 2: http://www.xbrl.org/2009/role/commonPracticeRef
-Topic 320
-SubTopic 10
-Name Accounting Standards Codification
-Section 45
-Paragraph 2
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147481830/320-10-45-2
Reference 3: http://www.xbrl.org/2003/role/disclosureRef
-Topic 942
-SubTopic 210
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.9-03(6))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147478546/942-210-S99-1
Reference 4: http://www.xbrl.org/2003/role/disclosureRef
-Topic 320
-SubTopic 10
-Name Accounting Standards Codification
-Section 45
-Paragraph 1
-Subparagraph (b)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147481830/320-10-45-1
| Name: |
us-gaap_DebtSecuritiesHeldToMaturityAmortizedCostAfterAllowanceForCreditLossCurrent |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:monetaryItemType |
| Balance Type: |
debit |
| Period Type: |
instant |
|
| X |
- DefinitionLine items represent financial concepts included in a table. These concepts are used to disclose reportable information associated with domain members defined in one or many axes to the table.
| Name: |
us-gaap_FairValueBalanceSheetGroupingFinancialStatementCaptionsLineItems |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:stringItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionAmount of accumulated unrealized loss on investment in debt security measured at amortized cost (held-to-maturity). Reference 1: http://fasb.org/us-gaap/role/ref/otherTransitionRef
-Topic 320
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 5
-Subparagraph (c)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147481800/320-10-50-5
Reference 2: http://www.xbrl.org/2003/role/disclosureRef
-Topic 320
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 5A
-Subparagraph (c)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147481800/320-10-50-5A
| Name: |
us-gaap_HeldToMaturitySecuritiesAccumulatedUnrecognizedHoldingLoss |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:monetaryItemType |
| Balance Type: |
debit |
| Period Type: |
instant |
|
| X |
- DefinitionThis element represents the noncurrent portion of investments which are not defined as or included in marketable (debt, equity, or other) securities that are pledged or subject to withdrawal restrictions. Reference 1: http://www.xbrl.org/2003/role/disclosureRef
-Topic 954
-SubTopic 210
-Name Accounting Standards Codification
-Section 45
-Paragraph 4
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147477220/954-210-45-4
Reference 2: http://www.xbrl.org/2003/role/disclosureRef
-Topic 954
-SubTopic 210
-Name Accounting Standards Codification
-Section 50
-Paragraph 2
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147478600/954-210-50-2
| Name: |
us-gaap_RestrictedInvestmentsNoncurrent |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:monetaryItemType |
| Balance Type: |
debit |
| Period Type: |
instant |
|
| X |
- Details
| Name: |
us-gaap_FinancialInstrumentAxis=us-gaap_USTreasuryBillSecuritiesMember |
| Namespace Prefix: |
|
| Data Type: |
na |
| Balance Type: |
|
| Period Type: |
|
|
| X |
- Details
| Name: |
us-gaap_FinancialInstrumentAxis=us-gaap_CertificatesOfDepositMember |
| Namespace Prefix: |
|
| Data Type: |
na |
| Balance Type: |
|
| Period Type: |
|
|
| X |
- Details
| Name: |
us-gaap_BalanceSheetLocationAxis=us-gaap_ShortTermInvestmentsMember |
| Namespace Prefix: |
|
| Data Type: |
na |
| Balance Type: |
|
| Period Type: |
|
|
| X |
- Details
| Name: |
us-gaap_BalanceSheetLocationAxis=us-gaap_CashAndCashEquivalentsMember |
| Namespace Prefix: |
|
| Data Type: |
na |
| Balance Type: |
|
| Period Type: |
|
|
v3.24.2.u1
Accounts Receivable - Schedule of Accounts Receivable (Details) - USD ($)
$ in Thousands |
Jun. 30, 2024 |
Dec. 31, 2023 |
| Accounts Receivable, after Allowance for Credit Loss [Abstract] |
|
|
| Government receivables |
$ 78,529
|
$ 35,529
|
| Pharmacy rebate receivables |
94,695
|
75,894
|
| Other receivables |
10,085
|
8,326
|
| Total accounts receivable |
183,309
|
119,749
|
| Allowance for credit losses |
(95)
|
0
|
| Accounts receivable, net |
$ 183,214
|
$ 119,749
|
| X |
- Definition
+ References
+ Details
| Name: |
alhc_PharmacyRebateReceivables |
| Namespace Prefix: |
alhc_ |
| Data Type: |
xbrli:monetaryItemType |
| Balance Type: |
debit |
| Period Type: |
instant |
|
| X |
- DefinitionAmount, before allowance for credit loss, of right to consideration from customer for product sold and service rendered in normal course of business. Reference 1: http://www.xbrl.org/2003/role/disclosureRef
-Topic 310
-SubTopic 10
-Name Accounting Standards Codification
-Section 45
-Paragraph 2
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147481990/310-10-45-2
Reference 2: http://www.xbrl.org/2003/role/disclosureRef
-Topic 310
-SubTopic 10
-Name Accounting Standards Codification
-Section 45
-Paragraph 13
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147481990/310-10-45-13
Reference 3: http://www.xbrl.org/2009/role/commonPracticeRef
-Topic 944
-SubTopic 210
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.7-03(a)(5))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147478777/944-210-S99-1
Reference 4: http://www.xbrl.org/2003/role/disclosureRef
-Topic 210
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.5-02(3)(a)(1))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480566/210-10-S99-1
| Name: |
us-gaap_AccountsReceivableGross |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:monetaryItemType |
| Balance Type: |
debit |
| Period Type: |
instant |
|
| X |
- DefinitionAmount, after allowance for credit loss, of right to consideration from customer for product sold and service rendered in normal course of business. Reference 1: http://www.xbrl.org/2003/role/exampleRef
-Topic 946
-SubTopic 310
-Name Accounting Standards Codification
-Section 45
-Paragraph 1
-Subparagraph (d)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147477802/946-310-45-1
Reference 2: http://www.xbrl.org/2009/role/commonPracticeRef
-Topic 944
-SubTopic 210
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.7-03(a)(5))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147478777/944-210-S99-1
Reference 3: http://www.xbrl.org/2003/role/disclosureRef
-Topic 946
-SubTopic 210
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.6-04(5)(b))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147479170/946-210-S99-1
Reference 4: http://www.xbrl.org/2003/role/disclosureRef
-Topic 954
-SubTopic 310
-Name Accounting Standards Codification
-Section 45
-Paragraph 1
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147479196/954-310-45-1
Reference 5: http://www.xbrl.org/2009/role/commonPracticeRef
-Topic 944
-SubTopic 210
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.7-03(a)(3))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147478777/944-210-S99-1
| Name: |
us-gaap_AccountsReceivableNet |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:monetaryItemType |
| Balance Type: |
debit |
| Period Type: |
instant |
|
| X |
- References
+ Details
| Name: |
us-gaap_AccountsReceivableNetAbstract |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:stringItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionAmount of allowance for credit loss on accounts receivable. Reference 1: http://www.xbrl.org/2009/role/commonPracticeRef
-Topic 944
-SubTopic 210
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.7-03(a)(5))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147478777/944-210-S99-1
Reference 2: http://www.xbrl.org/2003/role/disclosureRef
-Topic 210
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.5-02(4))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480566/210-10-S99-1
Reference 3: http://www.xbrl.org/2003/role/disclosureRef
-Topic 326
-SubTopic 20
-Name Accounting Standards Codification
-Section 45
-Paragraph 1
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147479344/326-20-45-1
Reference 4: http://www.xbrl.org/2003/role/disclosureRef
-Topic 310
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 4
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147481962/310-10-50-4
Reference 5: http://www.xbrl.org/2003/role/disclosureRef
-Topic 326
-SubTopic 20
-Name Accounting Standards Codification
-Section 50
-Paragraph 13
-Subparagraph (a)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147479319/326-20-50-13
Reference 6: http://www.xbrl.org/2003/role/disclosureRef
-Topic 326
-SubTopic 20
-Name Accounting Standards Codification
-Section 50
-Paragraph 13
-Subparagraph (f)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147479319/326-20-50-13
| Name: |
us-gaap_AllowanceForDoubtfulAccountsReceivable |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:monetaryItemType |
| Balance Type: |
credit |
| Period Type: |
instant |
|
| X |
- DefinitionThe amount of receivables that are derived from government contracts. Reference 1: http://www.xbrl.org/2003/role/disclosureRef
-Topic 912
-SubTopic 310
-Name Accounting Standards Codification
-Section 45
-Paragraph 1
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147478345/912-310-45-1
| Name: |
us-gaap_GovernmentContractReceivable |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:monetaryItemType |
| Balance Type: |
debit |
| Period Type: |
instant |
|
| X |
- DefinitionAmount due from parties in nontrade transactions, classified as other. Reference 1: http://www.xbrl.org/2003/role/exampleRef
-Topic 280
-SubTopic 10
-Name Accounting Standards Codification
-Section 55
-Paragraph 49
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482785/280-10-55-49
Reference 2: http://www.xbrl.org/2003/role/disclosureRef
-Topic 946
-SubTopic 210
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.6-04(5)(a)(5))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147479170/946-210-S99-1
Reference 3: http://www.xbrl.org/2003/role/disclosureRef
-Topic 210
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.5-02(3)(a)(4))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480566/210-10-S99-1
Reference 4: http://www.xbrl.org/2009/role/commonPracticeRef
-Topic 944
-SubTopic 210
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.7-03(a)(3))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147478777/944-210-S99-1
| Name: |
us-gaap_OtherReceivables |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:monetaryItemType |
| Balance Type: |
debit |
| Period Type: |
instant |
|
v3.24.2.u1
| X |
- References
+ Details
| Name: |
us-gaap_AccountsReceivableNetAbstract |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:stringItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionAmount of expense (reversal of expense) for expected credit loss on accounts receivable. Reference 1: http://www.xbrl.org/2003/role/disclosureRef
-Topic 326
-SubTopic 20
-Name Accounting Standards Codification
-Section 50
-Paragraph 13
-Subparagraph (b)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147479319/326-20-50-13
Reference 2: http://www.xbrl.org/2003/role/disclosureRef
-Topic 220
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 2
-Subparagraph (SX 210.5-03(5))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147483621/220-10-S99-2
| Name: |
us-gaap_ProvisionForDoubtfulAccounts |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:monetaryItemType |
| Balance Type: |
debit |
| Period Type: |
duration |
|
v3.24.2.u1
Property and Equipment - Schedule of Property and Equipment (Details) - USD ($)
$ in Thousands |
Jun. 30, 2024 |
Dec. 31, 2023 |
| Property Plant and Equipment [Line Items] |
|
|
| Subtotal |
$ 198,563
|
$ 175,586
|
| Less accumulated depreciation |
(136,133)
|
(123,685)
|
| Property and equipment-net |
62,430
|
51,901
|
| Computers and equipment |
|
|
| Property Plant and Equipment [Line Items] |
|
|
| Subtotal |
12,235
|
11,447
|
| Office equipment and furniture |
|
|
| Property Plant and Equipment [Line Items] |
|
|
| Subtotal |
4,397
|
4,396
|
| Software |
|
|
| Property Plant and Equipment [Line Items] |
|
|
| Subtotal |
165,697
|
148,864
|
| Leasehold improvements |
|
|
| Property Plant and Equipment [Line Items] |
|
|
| Subtotal |
6,347
|
6,347
|
| Construction in progress |
|
|
| Property Plant and Equipment [Line Items] |
|
|
| Subtotal |
$ 9,887
|
$ 4,532
|
| X |
- DefinitionAmount of accumulated depreciation, depletion and amortization for physical assets used in the normal conduct of business to produce goods and services. Reference 1: http://www.xbrl.org/2003/role/disclosureRef
-Topic 944
-SubTopic 210
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.7-03(a)(8)(b))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147478777/944-210-S99-1
Reference 2: http://www.xbrl.org/2003/role/disclosureRef
-Topic 210
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.5-02(14))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480566/210-10-S99-1
Reference 3: http://fasb.org/us-gaap/role/ref/legacyRef
-Name Accounting Standards Codification
-Topic 360
-SubTopic 10
-Section 50
-Paragraph 1
-Subparagraph (c)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482099/360-10-50-1
| Name: |
us-gaap_AccumulatedDepreciationDepletionAndAmortizationPropertyPlantAndEquipment |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:monetaryItemType |
| Balance Type: |
credit |
| Period Type: |
instant |
|
| X |
- DefinitionAmount before accumulated depreciation, depletion and amortization of physical assets used in the normal conduct of business and not intended for resale. Examples include, but are not limited to, land, buildings, machinery and equipment, office equipment, and furniture and fixtures. Reference 1: http://www.xbrl.org/2003/role/disclosureRef
-Topic 944
-SubTopic 210
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.7-03(a)(8))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147478777/944-210-S99-1
Reference 2: http://www.xbrl.org/2003/role/disclosureRef
-Topic 210
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.5-02(13))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480566/210-10-S99-1
Reference 3: http://fasb.org/us-gaap/role/ref/legacyRef
-Topic 360
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 1
-Subparagraph (b)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482099/360-10-50-1
| Name: |
us-gaap_PropertyPlantAndEquipmentGross |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:monetaryItemType |
| Balance Type: |
debit |
| Period Type: |
instant |
|
| X |
- DefinitionLine items represent financial concepts included in a table. These concepts are used to disclose reportable information associated with domain members defined in one or many axes to the table. Reference 1: http://www.xbrl.org/2003/role/disclosureRef
-Topic 842
-SubTopic 20
-Name Accounting Standards Codification
-Section 50
-Paragraph 7A
-Subparagraph (a)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147478964/842-20-50-7A
| Name: |
us-gaap_PropertyPlantAndEquipmentLineItems |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:stringItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionAmount after accumulated depreciation, depletion and amortization of physical assets used in the normal conduct of business to produce goods and services and not intended for resale. Examples include, but are not limited to, land, buildings, machinery and equipment, office equipment, and furniture and fixtures. Reference 1: http://fasb.org/us-gaap/role/ref/legacyRef
-Name Accounting Standards Codification
-Section 50
-Paragraph 1
-SubTopic 10
-Topic 360
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482099/360-10-50-1
Reference 2: http://www.xbrl.org/2003/role/disclosureRef
-Topic 842
-SubTopic 20
-Name Accounting Standards Codification
-Section 50
-Paragraph 7A
-Subparagraph (a)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147478964/842-20-50-7A
Reference 3: http://www.xbrl.org/2003/role/exampleRef
-Topic 852
-SubTopic 10
-Name Accounting Standards Codification
-Section 55
-Paragraph 10
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147481372/852-10-55-10
Reference 4: http://www.xbrl.org/2003/role/disclosureRef
-Topic 944
-SubTopic 210
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.7-03(a)(8))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147478777/944-210-S99-1
Reference 5: http://www.xbrl.org/2003/role/disclosureRef
-Topic 942
-SubTopic 360
-Name Accounting Standards Codification
-Section 50
-Paragraph 1
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147478451/942-360-50-1
| Name: |
us-gaap_PropertyPlantAndEquipmentNet |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:monetaryItemType |
| Balance Type: |
debit |
| Period Type: |
instant |
|
| X |
- Details
| Name: |
us-gaap_PropertyPlantAndEquipmentByTypeAxis=us-gaap_ComputerEquipmentMember |
| Namespace Prefix: |
|
| Data Type: |
na |
| Balance Type: |
|
| Period Type: |
|
|
| X |
- Details
| Name: |
us-gaap_PropertyPlantAndEquipmentByTypeAxis=us-gaap_FurnitureAndFixturesMember |
| Namespace Prefix: |
|
| Data Type: |
na |
| Balance Type: |
|
| Period Type: |
|
|
| X |
- Details
| Name: |
us-gaap_PropertyPlantAndEquipmentByTypeAxis=alhc_SoftwareMember |
| Namespace Prefix: |
|
| Data Type: |
na |
| Balance Type: |
|
| Period Type: |
|
|
| X |
- Details
| Name: |
us-gaap_PropertyPlantAndEquipmentByTypeAxis=us-gaap_LeaseholdImprovementsMember |
| Namespace Prefix: |
|
| Data Type: |
na |
| Balance Type: |
|
| Period Type: |
|
|
| X |
- Details
| Name: |
us-gaap_PropertyPlantAndEquipmentByTypeAxis=us-gaap_ConstructionInProgressMember |
| Namespace Prefix: |
|
| Data Type: |
na |
| Balance Type: |
|
| Period Type: |
|
|
v3.24.2.u1
| X |
- DefinitionThe amount of expense recognized in the current period that reflects the allocation of the cost of tangible assets over the assets' useful lives. Includes production and non-production related depreciation. Reference 1: http://fasb.org/us-gaap/role/ref/legacyRef
-Name Accounting Standards Codification
-Section 45
-Paragraph 28
-Subparagraph (b)
-SubTopic 10
-Topic 230
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482740/230-10-45-28
Reference 2: http://fasb.org/us-gaap/role/ref/legacyRef
-Name Accounting Standards Codification
-Topic 360
-SubTopic 10
-Section 50
-Paragraph 1
-Subparagraph (a)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482099/360-10-50-1
| Name: |
us-gaap_Depreciation |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:monetaryItemType |
| Balance Type: |
debit |
| Period Type: |
duration |
|
| X |
- DefinitionLine items represent financial concepts included in a table. These concepts are used to disclose reportable information associated with domain members defined in one or many axes to the table. Reference 1: http://www.xbrl.org/2003/role/disclosureRef
-Topic 842
-SubTopic 20
-Name Accounting Standards Codification
-Section 50
-Paragraph 7A
-Subparagraph (a)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147478964/842-20-50-7A
| Name: |
us-gaap_PropertyPlantAndEquipmentLineItems |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:stringItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- Details
| Name: |
us-gaap_IncomeStatementLocationAxis=alhc_MedicalExpensesMember |
| Namespace Prefix: |
|
| Data Type: |
na |
| Balance Type: |
|
| Period Type: |
|
|
v3.24.2.u1
Goodwill and Intangible Assets - Schedule of Intangible Assets (Details) - USD ($)
$ in Thousands |
6 Months Ended |
12 Months Ended |
Jun. 30, 2024 |
Dec. 31, 2023 |
| Indefinite Lived Intangible Assets By Major Class [Line Items] |
|
|
| Goodwill, Gross Carrying Value |
$ 34,826
|
$ 34,826
|
| Goodwill |
34,826
|
34,826
|
| Gross Carrying Value |
43,543
|
43,543
|
| Accumulated Amortization |
(3,516)
|
(3,465)
|
| Net Carrying Value |
40,027
|
40,078
|
| Plan member relationships |
|
|
| Indefinite Lived Intangible Assets By Major Class [Line Items] |
|
|
| Gross Carrying Value |
2,700
|
2,700
|
| Accumulated Amortization |
(2,700)
|
(2,700)
|
| Net Carrying Value |
$ 0
|
$ 0
|
| Weighted Average Life |
9 years
|
9 years
|
| Other |
|
|
| Indefinite Lived Intangible Assets By Major Class [Line Items] |
|
|
| Gross Carrying Value |
$ 1,050
|
$ 1,050
|
| Accumulated Amortization |
(816)
|
(765)
|
| Net Carrying Value |
$ 234
|
$ 285
|
| Other | Minimum |
|
|
| Indefinite Lived Intangible Assets By Major Class [Line Items] |
|
|
| Weighted Average Life |
2 years
|
2 years
|
| Other | Maximum |
|
|
| Indefinite Lived Intangible Assets By Major Class [Line Items] |
|
|
| Weighted Average Life |
10 years
|
10 years
|
| License (indefinite lived) |
|
|
| Indefinite Lived Intangible Assets By Major Class [Line Items] |
|
|
| Gross Carrying Value |
$ 4,967
|
$ 4,967
|
| Net Carrying Value |
$ 4,967
|
$ 4,967
|
| X |
- DefinitionWeighted average amortization period of finite-lived intangible assets acquired either individually or as part of a group of assets, in 'PnYnMnDTnHnMnS' format, for example, 'P1Y5M13D' represents the reported fact of one year, five months, and thirteen days. Reference 1: http://www.xbrl.org/2003/role/disclosureRef
-Topic 350
-SubTopic 30
-Name Accounting Standards Codification
-Section 50
-Paragraph 1
-Subparagraph (a)(3)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482665/350-30-50-1
Reference 2: http://www.xbrl.org/2003/role/disclosureRef
-Topic 985
-SubTopic 20
-Name Accounting Standards Codification
-Section 50
-Paragraph 2
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147481283/985-20-50-2
| Name: |
us-gaap_AcquiredFiniteLivedIntangibleAssetsWeightedAverageUsefulLife |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:durationItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionAccumulated amount of amortization of assets, excluding financial assets and goodwill, lacking physical substance with a finite life. Reference 1: http://www.xbrl.org/2003/role/exampleRef
-Topic 350
-SubTopic 30
-Name Accounting Standards Codification
-Section 55
-Paragraph 40
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482640/350-30-55-40
Reference 2: http://www.xbrl.org/2003/role/disclosureRef
-Topic 350
-SubTopic 10
-Name Accounting Standards Codification
-Section S45
-Paragraph 1
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480265/350-10-S45-1
Reference 3: http://www.xbrl.org/2003/role/disclosureRef
-Topic 350
-SubTopic 30
-Name Accounting Standards Codification
-Section 50
-Paragraph 2
-Subparagraph (a)(1)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482665/350-30-50-2
Reference 4: http://www.xbrl.org/2003/role/disclosureRef
-Topic 210
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.5-02(16))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480566/210-10-S99-1
| Name: |
us-gaap_FiniteLivedIntangibleAssetsAccumulatedAmortization |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:monetaryItemType |
| Balance Type: |
credit |
| Period Type: |
instant |
|
| X |
- DefinitionAmount before amortization of assets, excluding financial assets and goodwill, lacking physical substance with a finite life. Reference 1: http://www.xbrl.org/2003/role/exampleRef
-Topic 350
-SubTopic 30
-Name Accounting Standards Codification
-Section 55
-Paragraph 40
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482640/350-30-55-40
Reference 2: http://www.xbrl.org/2003/role/disclosureRef
-Topic 350
-SubTopic 10
-Name Accounting Standards Codification
-Section S45
-Paragraph 1
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480265/350-10-S45-1
Reference 3: http://www.xbrl.org/2003/role/disclosureRef
-Topic 350
-SubTopic 30
-Name Accounting Standards Codification
-Section 50
-Paragraph 2
-Subparagraph (a)(1)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482665/350-30-50-2
Reference 4: http://www.xbrl.org/2003/role/disclosureRef
-Topic 928
-SubTopic 340
-Name Accounting Standards Codification
-Section 50
-Paragraph 1
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147478859/928-340-50-1
| Name: |
us-gaap_FiniteLivedIntangibleAssetsGross |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:monetaryItemType |
| Balance Type: |
debit |
| Period Type: |
instant |
|
| X |
- DefinitionAmount after amortization of assets, excluding financial assets and goodwill, lacking physical substance with a finite life. Reference 1: http://www.xbrl.org/2009/role/commonPracticeRef
-Topic 350
-SubTopic 30
-Name Accounting Standards Codification
-Section 50
-Paragraph 2
-Subparagraph (a)(1)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482665/350-30-50-2
Reference 2: http://www.xbrl.org/2003/role/disclosureRef
-Topic 926
-SubTopic 20
-Name Accounting Standards Codification
-Section 50
-Paragraph 5
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147483154/926-20-50-5
| Name: |
us-gaap_FiniteLivedIntangibleAssetsNet |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:monetaryItemType |
| Balance Type: |
debit |
| Period Type: |
instant |
|
| X |
- DefinitionAmount, after accumulated impairment loss, of asset representing future economic benefit arising from other asset acquired in business combination or from joint venture formation or both, that is not individually identified and separately recognized. Reference 1: http://www.xbrl.org/2003/role/exampleRef
-Topic 280
-SubTopic 10
-Name Accounting Standards Codification
-Section 55
-Paragraph 49
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482785/280-10-55-49
Reference 2: http://www.xbrl.org/2003/role/exampleRef
-Topic 350
-SubTopic 20
-Name Accounting Standards Codification
-Section 55
-Paragraph 24
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482548/350-20-55-24
Reference 3: http://www.xbrl.org/2003/role/exampleRef
-Topic 820
-SubTopic 10
-Name Accounting Standards Codification
-Section 55
-Paragraph 100
-Subparagraph (d)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482078/820-10-55-100
Reference 4: http://www.xbrl.org/2003/role/exampleRef
-Topic 852
-SubTopic 10
-Name Accounting Standards Codification
-Section 55
-Paragraph 10
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147481372/852-10-55-10
Reference 5: http://www.xbrl.org/2003/role/disclosureRef
-Topic 210
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.5-02(15))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480566/210-10-S99-1
Reference 6: http://www.xbrl.org/2003/role/disclosureRef
-Topic 350
-SubTopic 20
-Name Accounting Standards Codification
-Section 45
-Paragraph 1
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482598/350-20-45-1
Reference 7: http://www.xbrl.org/2009/role/commonPracticeRef
-Topic 350
-SubTopic 20
-Name Accounting Standards Codification
-Section 50
-Paragraph 1
-Subparagraph (a)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482573/350-20-50-1
Reference 8: http://www.xbrl.org/2009/role/commonPracticeRef
-Topic 350
-SubTopic 20
-Name Accounting Standards Codification
-Section 50
-Paragraph 1
-Subparagraph (h)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482573/350-20-50-1
Reference 9: http://www.xbrl.org/2003/role/disclosureRef
-Topic 942
-SubTopic 210
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.9-03(10)(1))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147478546/942-210-S99-1
| Name: |
us-gaap_Goodwill |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:monetaryItemType |
| Balance Type: |
debit |
| Period Type: |
instant |
|
| X |
- DefinitionAmount, before accumulated impairment loss, of asset representing future economic benefit arising from other asset acquired in business combination or from joint venture formation or both, that is not individually identified and separately recognized. Reference 1: http://www.xbrl.org/2003/role/exampleRef
-Topic 350
-SubTopic 20
-Name Accounting Standards Codification
-Section 55
-Paragraph 24
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482548/350-20-55-24
Reference 2: http://www.xbrl.org/2003/role/disclosureRef
-Topic 350
-SubTopic 20
-Name Accounting Standards Codification
-Section 50
-Paragraph 1
-Subparagraph (a)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482573/350-20-50-1
Reference 3: http://www.xbrl.org/2003/role/disclosureRef
-Topic 350
-SubTopic 20
-Name Accounting Standards Codification
-Section 50
-Paragraph 1
-Subparagraph (h)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482573/350-20-50-1
| Name: |
us-gaap_GoodwillGross |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:monetaryItemType |
| Balance Type: |
debit |
| Period Type: |
instant |
|
| X |
- DefinitionLine items represent financial concepts included in a table. These concepts are used to disclose reportable information associated with domain members defined in one or many axes to the table. Reference 1: http://www.xbrl.org/2003/role/exampleRef
-Topic 350
-SubTopic 30
-Name Accounting Standards Codification
-Section 55
-Paragraph 40
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482640/350-30-55-40
Reference 2: http://www.xbrl.org/2003/role/disclosureRef
-Topic 350
-SubTopic 30
-Name Accounting Standards Codification
-Section 45
-Paragraph 1
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482686/350-30-45-1
Reference 3: http://www.xbrl.org/2003/role/disclosureRef
-Topic 350
-SubTopic 30
-Name Accounting Standards Codification
-Section 50
-Paragraph 3
-Subparagraph (d)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482665/350-30-50-3
Reference 4: http://www.xbrl.org/2003/role/disclosureRef
-Topic 350
-SubTopic 30
-Name Accounting Standards Codification
-Section 50
-Paragraph 2
-Subparagraph (b)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482665/350-30-50-2
| Name: |
us-gaap_IndefiniteLivedIntangibleAssetsByMajorClassLineItems |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:stringItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- Details
| Name: |
us-gaap_FiniteLivedIntangibleAssetsByMajorClassAxis=alhc_PlanRelationshipMember |
| Namespace Prefix: |
|
| Data Type: |
na |
| Balance Type: |
|
| Period Type: |
|
|
| X |
- Details
| Name: |
us-gaap_FiniteLivedIntangibleAssetsByMajorClassAxis=us-gaap_OtherIntangibleAssetsMember |
| Namespace Prefix: |
|
| Data Type: |
na |
| Balance Type: |
|
| Period Type: |
|
|
| X |
- Details
| Name: |
srt_RangeAxis=srt_MinimumMember |
| Namespace Prefix: |
|
| Data Type: |
na |
| Balance Type: |
|
| Period Type: |
|
|
| X |
- Details
| Name: |
srt_RangeAxis=srt_MaximumMember |
| Namespace Prefix: |
|
| Data Type: |
na |
| Balance Type: |
|
| Period Type: |
|
|
| X |
- Details
| Name: |
us-gaap_IndefiniteLivedIntangibleAssetsByMajorClassAxis=us-gaap_LicenseMember |
| Namespace Prefix: |
|
| Data Type: |
na |
| Balance Type: |
|
| Period Type: |
|
|
v3.24.2.u1
| X |
- DefinitionThe aggregate expense charged against earnings to allocate the cost of intangible assets (nonphysical assets not used in production) in a systematic and rational manner to the periods expected to benefit from such assets. As a noncash expense, this element is added back to net income when calculating cash provided by or used in operations using the indirect method. Reference 1: http://fasb.org/us-gaap/role/ref/legacyRef
-Name Accounting Standards Codification
-Section 45
-Paragraph 28
-Subparagraph (b)
-SubTopic 10
-Topic 230
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482740/230-10-45-28
Reference 2: http://www.xbrl.org/2003/role/exampleRef
-Topic 350
-SubTopic 30
-Name Accounting Standards Codification
-Section 55
-Paragraph 40
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482640/350-30-55-40
Reference 3: http://www.xbrl.org/2003/role/disclosureRef
-Topic 350
-SubTopic 30
-Name Accounting Standards Codification
-Section 50
-Paragraph 2
-Subparagraph (a)(2)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482665/350-30-50-2
Reference 4: http://www.xbrl.org/2003/role/disclosureRef
-Topic 350
-SubTopic 30
-Name Accounting Standards Codification
-Section 45
-Paragraph 2
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482686/350-30-45-2
| Name: |
us-gaap_AmortizationOfIntangibleAssets |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:monetaryItemType |
| Balance Type: |
debit |
| Period Type: |
duration |
|
| X |
- DefinitionTotal loss recognized during the period from the impairment of goodwill plus the loss recognized in the period resulting from the impairment of the carrying amount of intangible assets, other than goodwill.
| Name: |
us-gaap_GoodwillAndIntangibleAssetImpairment |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:monetaryItemType |
| Balance Type: |
debit |
| Period Type: |
duration |
|
| X |
- References
+ Details
| Name: |
us-gaap_GoodwillAndIntangibleAssetsDisclosureAbstract |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:stringItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
v3.24.2.u1
| X |
- DefinitionAmount of amortization for assets, excluding financial assets and goodwill, lacking physical substance with finite life expected to be recognized in next fiscal year following current fiscal year. Excludes interim and annual periods when interim periods are reported from current statement of financial position date (rolling approach). Reference 1: http://www.xbrl.org/2003/role/exampleRef
-Topic 350
-SubTopic 30
-Name Accounting Standards Codification
-Section 55
-Paragraph 40
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482640/350-30-55-40
Reference 2: http://www.xbrl.org/2003/role/disclosureRef
-Topic 350
-SubTopic 30
-Name Accounting Standards Codification
-Section 50
-Paragraph 2
-Subparagraph (a)(3)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482665/350-30-50-2
Reference 3: http://www.xbrl.org/2003/role/disclosureRef
-Topic 985
-SubTopic 20
-Name Accounting Standards Codification
-Section 50
-Paragraph 2
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147481283/985-20-50-2
| Name: |
us-gaap_FiniteLivedIntangibleAssetsAmortizationExpenseNextTwelveMonths |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:monetaryItemType |
| Balance Type: |
debit |
| Period Type: |
instant |
|
| X |
- DefinitionAmount of amortization for assets, excluding financial assets and goodwill, lacking physical substance with finite life expected to be recognized in remainder of current fiscal year. Reference 1: http://www.xbrl.org/2009/role/commonPracticeRef
-Topic 985
-SubTopic 20
-Name Accounting Standards Codification
-Section 50
-Paragraph 2
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147481283/985-20-50-2
| Name: |
us-gaap_FiniteLivedIntangibleAssetsAmortizationExpenseRemainderOfFiscalYear |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:monetaryItemType |
| Balance Type: |
debit |
| Period Type: |
instant |
|
| X |
- DefinitionAmount of amortization for assets, excluding financial assets and goodwill, lacking physical substance with finite life expected to be recognized in fourth fiscal year following current fiscal year. Excludes interim and annual periods when interim periods are reported from current statement of financial position date (rolling approach). Reference 1: http://www.xbrl.org/2003/role/exampleRef
-Topic 350
-SubTopic 30
-Name Accounting Standards Codification
-Section 55
-Paragraph 40
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482640/350-30-55-40
Reference 2: http://www.xbrl.org/2003/role/disclosureRef
-Topic 350
-SubTopic 30
-Name Accounting Standards Codification
-Section 50
-Paragraph 2
-Subparagraph (a)(3)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482665/350-30-50-2
Reference 3: http://www.xbrl.org/2003/role/disclosureRef
-Topic 985
-SubTopic 20
-Name Accounting Standards Codification
-Section 50
-Paragraph 2
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147481283/985-20-50-2
| Name: |
us-gaap_FiniteLivedIntangibleAssetsAmortizationExpenseYearFour |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:monetaryItemType |
| Balance Type: |
debit |
| Period Type: |
instant |
|
| X |
- DefinitionAmount of amortization for assets, excluding financial assets and goodwill, lacking physical substance with finite life expected to be recognized in third fiscal year following current fiscal year. Excludes interim and annual periods when interim periods are reported from current statement of financial position date (rolling approach). Reference 1: http://www.xbrl.org/2003/role/exampleRef
-Topic 350
-SubTopic 30
-Name Accounting Standards Codification
-Section 55
-Paragraph 40
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482640/350-30-55-40
Reference 2: http://www.xbrl.org/2003/role/disclosureRef
-Topic 350
-SubTopic 30
-Name Accounting Standards Codification
-Section 50
-Paragraph 2
-Subparagraph (a)(3)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482665/350-30-50-2
Reference 3: http://www.xbrl.org/2003/role/disclosureRef
-Topic 985
-SubTopic 20
-Name Accounting Standards Codification
-Section 50
-Paragraph 2
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147481283/985-20-50-2
| Name: |
us-gaap_FiniteLivedIntangibleAssetsAmortizationExpenseYearThree |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:monetaryItemType |
| Balance Type: |
debit |
| Period Type: |
instant |
|
| X |
- DefinitionAmount of amortization for assets, excluding financial assets and goodwill, lacking physical substance with finite life expected to be recognized in second fiscal year following current fiscal year. Excludes interim and annual periods when interim periods are reported from current statement of financial position date (rolling approach). Reference 1: http://www.xbrl.org/2003/role/exampleRef
-Topic 350
-SubTopic 30
-Name Accounting Standards Codification
-Section 55
-Paragraph 40
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482640/350-30-55-40
Reference 2: http://www.xbrl.org/2003/role/disclosureRef
-Topic 350
-SubTopic 30
-Name Accounting Standards Codification
-Section 50
-Paragraph 2
-Subparagraph (a)(3)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482665/350-30-50-2
Reference 3: http://www.xbrl.org/2003/role/disclosureRef
-Topic 985
-SubTopic 20
-Name Accounting Standards Codification
-Section 50
-Paragraph 2
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147481283/985-20-50-2
| Name: |
us-gaap_FiniteLivedIntangibleAssetsAmortizationExpenseYearTwo |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:monetaryItemType |
| Balance Type: |
debit |
| Period Type: |
instant |
|
| X |
- References
+ Details
| Name: |
us-gaap_GoodwillAndIntangibleAssetsDisclosureAbstract |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:stringItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
v3.24.2.u1
Medical Expenses Payable - Schedule of Medical Expenses Payable (Details) - USD ($)
$ in Thousands |
Jun. 30, 2024 |
Dec. 31, 2023 |
Jun. 30, 2023 |
Dec. 31, 2022 |
| Insurance [Abstract] |
|
|
|
|
| Claims incurred but not paid |
$ 156,379
|
$ 95,664
|
$ 91,888
|
$ 88,813
|
| Capitation and risk-sharing payable |
69,316
|
50,894
|
|
|
| Other |
89,674
|
58,841
|
|
|
| Medical expenses payable |
$ 315,369
|
$ 205,399
|
$ 207,198
|
|
| X |
- DefinitionLiability for claims and claims capitation payable and risk sharing payable.
| Name: |
alhc_LiabilityForClaimsAndClaimsCapitationPayableAndRiskSharingPayable |
| Namespace Prefix: |
alhc_ |
| Data Type: |
xbrli:monetaryItemType |
| Balance Type: |
credit |
| Period Type: |
instant |
|
| X |
- DefinitionLiability for claims and claims, other medical expenses payable.
| Name: |
alhc_LiabilityForClaimsAndClaimsOtherMedicalExpensesPayable |
| Namespace Prefix: |
alhc_ |
| Data Type: |
xbrli:monetaryItemType |
| Balance Type: |
credit |
| Period Type: |
instant |
|
| X |
- References
+ Details
| Name: |
us-gaap_InsuranceAbstract |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:stringItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionThe amount needed to reflect the estimated ultimate cost of settling claims relating to insured events that have occurred on or before the balance sheet date, whether or not reported to the insurer at that date. Reference 1: http://www.xbrl.org/2003/role/exampleRef
-Topic 944
-SubTopic 40
-Name Accounting Standards Codification
-Section 55
-Paragraph 7
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480046/944-40-55-7
Reference 2: http://www.xbrl.org/2003/role/exampleRef
-Topic 944
-SubTopic 40
-Name Accounting Standards Codification
-Section 55
-Paragraph 9E
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480046/944-40-55-9E
Reference 3: http://www.xbrl.org/2009/role/commonPracticeRef
-Topic 944
-SubTopic 40
-Name Accounting Standards Codification
-Section 50
-Paragraph 3
-Subparagraph (cc)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480081/944-40-50-3
Reference 4: http://www.xbrl.org/2009/role/commonPracticeRef
-Topic 944
-SubTopic 210
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.7-03(a)(13)(a)(1))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147478777/944-210-S99-1
| Name: |
us-gaap_LiabilityForClaimsAndClaimsAdjustmentExpense |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:monetaryItemType |
| Balance Type: |
credit |
| Period Type: |
instant |
|
| X |
- DefinitionEstimated costs as of the balance sheet date of settling insured claims and costs incurred in the claims settlement process for claims that have not yet been submitted to the insurance company for reimbursement.
| Name: |
us-gaap_LiabilityForUnpaidClaimsAndClaimsAdjustmentExpenseIncurredButNotReportedIBNRClaimsAmount |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:monetaryItemType |
| Balance Type: |
credit |
| Period Type: |
instant |
|
v3.24.2.u1
| X |
- DefinitionClaims reserve estimates, excluding provision from prior year claims and claims adjustment expense.
| Name: |
alhc_ClaimsReserveEstimatesExcludingProvisionFromPriorYearClaimsAndClaimsAdjustmentExpense |
| Namespace Prefix: |
alhc_ |
| Data Type: |
xbrli:monetaryItemType |
| Balance Type: |
credit |
| Period Type: |
duration |
|
| X |
- DefinitionRemaining claim amounts payment period.
| Name: |
alhc_RemainingClaimAmountsPaymentPeriod |
| Namespace Prefix: |
alhc_ |
| Data Type: |
xbrli:durationItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- References
+ Details
| Name: |
us-gaap_InsuranceAbstract |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:stringItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
v3.24.2.u1
Medical Expenses Payable - Schedule of Components of Change in Medical Expenses Payable (Details) - USD ($)
$ in Thousands |
6 Months Ended |
|
Jun. 30, 2024 |
Jun. 30, 2023 |
Dec. 31, 2023 |
| Liability for Unpaid Claims and Claims Adjustment Expense [Roll Forward] |
|
|
|
| Claims incurred but not paid - beginning balance |
$ 95,664
|
$ 88,813
|
|
| Incurred related to: |
|
|
|
| Current year |
407,156
|
235,027
|
|
| Prior years |
(7,257)
|
(7,168)
|
|
| Total incurred, net of reinsurance |
399,899
|
227,859
|
|
| Payments related to: |
|
|
|
| Current year |
263,824
|
156,152
|
|
| Prior years |
75,360
|
68,632
|
|
| Total payments, net of reinsurance |
339,184
|
224,784
|
|
| Claims incurred but not paid - ending balance |
156,379
|
91,888
|
|
| Capitation payable, risk-sharing payable, and other |
158,990
|
115,310
|
|
| Medical expenses payable |
$ 315,369
|
$ 207,198
|
$ 205,399
|
| X |
- DefinitionLiability for claims and claims, capitation payable, risk-sharing payable, and other.
| Name: |
alhc_LiabilityForClaimsAndClaimsCapitationPayableRiskSharingPayableAndOther |
| Namespace Prefix: |
alhc_ |
| Data Type: |
xbrli:monetaryItemType |
| Balance Type: |
credit |
| Period Type: |
instant |
|
| X |
- DefinitionThe amount needed to reflect the estimated ultimate cost of settling claims relating to insured events that have occurred on or before the balance sheet date, whether or not reported to the insurer at that date. Reference 1: http://www.xbrl.org/2003/role/exampleRef
-Topic 944
-SubTopic 40
-Name Accounting Standards Codification
-Section 55
-Paragraph 7
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480046/944-40-55-7
Reference 2: http://www.xbrl.org/2003/role/exampleRef
-Topic 944
-SubTopic 40
-Name Accounting Standards Codification
-Section 55
-Paragraph 9E
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480046/944-40-55-9E
Reference 3: http://www.xbrl.org/2009/role/commonPracticeRef
-Topic 944
-SubTopic 40
-Name Accounting Standards Codification
-Section 50
-Paragraph 3
-Subparagraph (cc)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480081/944-40-50-3
Reference 4: http://www.xbrl.org/2009/role/commonPracticeRef
-Topic 944
-SubTopic 210
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.7-03(a)(13)(a)(1))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147478777/944-210-S99-1
| Name: |
us-gaap_LiabilityForClaimsAndClaimsAdjustmentExpense |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:monetaryItemType |
| Balance Type: |
credit |
| Period Type: |
instant |
|
| X |
- References
+ Details
| Name: |
us-gaap_LiabilityForUnpaidClaimsAndClaimsAdjustmentExpenseClaimsPaidAbstract |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:stringItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionAmount, after effects of reinsurance, of payments to settle claims incurred in the current period and related claims settlement costs. Reference 1: http://www.xbrl.org/2003/role/exampleRef
-Topic 944
-SubTopic 40
-Name Accounting Standards Codification
-Section 55
-Paragraph 7
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480046/944-40-55-7
Reference 2: http://www.xbrl.org/2003/role/disclosureRef
-Topic 944
-SubTopic 40
-Name Accounting Standards Codification
-Section 50
-Paragraph 3
-Subparagraph (c)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480081/944-40-50-3
| Name: |
us-gaap_LiabilityForUnpaidClaimsAndClaimsAdjustmentExpenseClaimsPaidCurrentYear1 |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:monetaryItemType |
| Balance Type: |
credit |
| Period Type: |
duration |
|
| X |
- DefinitionAmount, after effects of reinsurance, of payments to settle claims incurred in prior periods and related claims settlement costs. Reference 1: http://www.xbrl.org/2003/role/exampleRef
-Topic 944
-SubTopic 40
-Name Accounting Standards Codification
-Section 55
-Paragraph 7
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480046/944-40-55-7
Reference 2: http://www.xbrl.org/2003/role/disclosureRef
-Topic 944
-SubTopic 40
-Name Accounting Standards Codification
-Section 50
-Paragraph 3
-Subparagraph (c)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480081/944-40-50-3
| Name: |
us-gaap_LiabilityForUnpaidClaimsAndClaimsAdjustmentExpenseClaimsPaidPriorYears1 |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:monetaryItemType |
| Balance Type: |
credit |
| Period Type: |
duration |
|
| X |
- DefinitionEstimated costs as of the balance sheet date of settling insured claims and costs incurred in the claims settlement process for claims that have not yet been submitted to the insurance company for reimbursement.
| Name: |
us-gaap_LiabilityForUnpaidClaimsAndClaimsAdjustmentExpenseIncurredButNotReportedIBNRClaimsAmount |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:monetaryItemType |
| Balance Type: |
credit |
| Period Type: |
instant |
|
| X |
- DefinitionAmount, after effects of reinsurance, of expense (reversal of expense) for claims incurred and costs incurred in the claim settlement process. Reference 1: http://www.xbrl.org/2003/role/exampleRef
-Topic 944
-SubTopic 40
-Name Accounting Standards Codification
-Section 55
-Paragraph 7
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480046/944-40-55-7
Reference 2: http://www.xbrl.org/2009/role/commonPracticeRef
-Topic 944
-SubTopic 40
-Name Accounting Standards Codification
-Section 50
-Paragraph 3
-Subparagraph (b)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480081/944-40-50-3
| Name: |
us-gaap_LiabilityForUnpaidClaimsAndClaimsAdjustmentExpenseIncurredClaims1 |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:monetaryItemType |
| Balance Type: |
debit |
| Period Type: |
duration |
|
| X |
- References
+ Details
| Name: |
us-gaap_LiabilityForUnpaidClaimsAndClaimsAdjustmentExpenseIncurredClaimsAbstract |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:stringItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionA roll forward is a reconciliation of a concept from the beginning of a period to the end of a period.
| Name: |
us-gaap_LiabilityForUnpaidClaimsAndClaimsAdjustmentExpenseNetAbstract |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:stringItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionAmount, after effects of reinsurance, of payments to settle insured claims and pay costs incurred in the claims settlement process. Reference 1: http://fasb.org/us-gaap/role/ref/legacyRef
-Name Accounting Standards Codification
-Section 45
-Paragraph 25
-Subparagraph (g)
-SubTopic 10
-Topic 230
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482740/230-10-45-25
Reference 2: http://www.xbrl.org/2003/role/exampleRef
-Topic 944
-SubTopic 40
-Name Accounting Standards Codification
-Section 55
-Paragraph 7
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480046/944-40-55-7
Reference 3: http://www.xbrl.org/2009/role/commonPracticeRef
-Topic 944
-SubTopic 40
-Name Accounting Standards Codification
-Section 50
-Paragraph 3
-Subparagraph (c)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480081/944-40-50-3
| Name: |
us-gaap_PaymentsForLossesAndLossAdjustmentExpense |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:monetaryItemType |
| Balance Type: |
credit |
| Period Type: |
duration |
|
v3.24.2.u1
Long-Term Debt - Schedule of Long-Term Debt Outstanding, Net of Unamortized Debt Issuance Costs (Details) - USD ($)
$ in Thousands |
Jun. 30, 2024 |
Dec. 31, 2023 |
| Debt Disclosure [Abstract] |
|
|
| Long-term debt |
$ 215,000
|
$ 165,000
|
| Less unamortized debt issuance costs |
(3,258)
|
(3,187)
|
| Long-term debt-net of amortization |
211,742
|
161,813
|
| Less current portion of long-term debt |
0
|
0
|
| Long-term debt - net of current portion |
$ 211,742
|
$ 161,813
|
| X |
- References
+ Details
| Name: |
us-gaap_DebtDisclosureAbstract |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:stringItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionAmount, before unamortized (discount) premium and debt issuance costs, of long-term debt. Includes, but is not limited to, notes payable, bonds payable, commercial loans, mortgage loans, convertible debt, subordinated debt and other types of debt. Reference 1: http://fasb.org/us-gaap/role/ref/legacyRef
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.5-02(22))
-SubTopic 10
-Topic 210
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480566/210-10-S99-1
Reference 2: http://fasb.org/us-gaap/role/ref/legacyRef
-Topic 942
-SubTopic 210
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.9-03(16))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147478546/942-210-S99-1
Reference 3: http://www.xbrl.org/2003/role/disclosureRef
-Topic 470
-SubTopic 20
-Name Accounting Standards Codification
-Section 50
-Paragraph 4
-Subparagraph (b)(1)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147481139/470-20-50-4
| Name: |
us-gaap_DebtInstrumentCarryingAmount |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:monetaryItemType |
| Balance Type: |
credit |
| Period Type: |
instant |
|
| X |
- DefinitionAmount of unamortized debt discount (premium) and debt issuance costs. Reference 1: http://www.xbrl.org/2003/role/exampleRef
-Topic 835
-SubTopic 30
-Name Accounting Standards Codification
-Section 55
-Paragraph 8
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482949/835-30-55-8
Reference 2: http://www.xbrl.org/2003/role/exampleRef
-Topic 470
-SubTopic 20
-Name Accounting Standards Codification
-Section 55
-Paragraph 69B
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147481568/470-20-55-69B
Reference 3: http://www.xbrl.org/2003/role/exampleRef
-Topic 470
-SubTopic 20
-Name Accounting Standards Codification
-Section 55
-Paragraph 69C
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147481568/470-20-55-69C
Reference 4: http://www.xbrl.org/2003/role/disclosureRef
-Topic 470
-SubTopic 20
-Name Accounting Standards Codification
-Section 50
-Paragraph 1D
-Subparagraph (a)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147481139/470-20-50-1D
Reference 5: http://www.xbrl.org/2003/role/disclosureRef
-Topic 835
-SubTopic 30
-Name Accounting Standards Codification
-Section 50
-Paragraph 1
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482900/835-30-50-1
Reference 6: http://www.xbrl.org/2003/role/disclosureRef
-Topic 835
-SubTopic 30
-Name Accounting Standards Codification
-Section 45
-Paragraph 2
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482925/835-30-45-2
Reference 7: http://www.xbrl.org/2003/role/disclosureRef
-Topic 470
-SubTopic 20
-Name Accounting Standards Codification
-Section 50
-Paragraph 4
-Subparagraph (b)(2)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147481139/470-20-50-4
Reference 8: http://www.xbrl.org/2003/role/disclosureRef
-Topic 835
-SubTopic 30
-Name Accounting Standards Codification
-Section 45
-Paragraph 1A
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482925/835-30-45-1A
| Name: |
us-gaap_DebtInstrumentUnamortizedDiscountPremiumAndDebtIssuanceCostsNet |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:monetaryItemType |
| Balance Type: |
debit |
| Period Type: |
instant |
|
| X |
- DefinitionAmount, after deduction of unamortized premium (discount) and debt issuance cost, of long-term debt. Excludes lease obligation. Reference 1: http://fasb.org/us-gaap/role/ref/legacyRef
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.5-02(22))
-SubTopic 10
-Topic 210
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480566/210-10-S99-1
Reference 2: http://www.xbrl.org/2003/role/exampleRef
-Topic 835
-SubTopic 30
-Name Accounting Standards Codification
-Section 55
-Paragraph 8
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482949/835-30-55-8
Reference 3: http://fasb.org/us-gaap/role/ref/legacyRef
-Topic 942
-SubTopic 210
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.9-03(16))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147478546/942-210-S99-1
Reference 4: http://www.xbrl.org/2003/role/exampleRef
-Topic 470
-SubTopic 20
-Name Accounting Standards Codification
-Section 55
-Paragraph 69B
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147481568/470-20-55-69B
Reference 5: http://www.xbrl.org/2003/role/exampleRef
-Topic 470
-SubTopic 20
-Name Accounting Standards Codification
-Section 55
-Paragraph 69C
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147481568/470-20-55-69C
Reference 6: http://www.xbrl.org/2003/role/disclosureRef
-Topic 470
-SubTopic 20
-Name Accounting Standards Codification
-Section 50
-Paragraph 1D
-Subparagraph (b)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147481139/470-20-50-1D
Reference 7: http://www.xbrl.org/2009/role/commonPracticeRef
-Topic 944
-SubTopic 210
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.7-03(a)(16)(a)(2))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147478777/944-210-S99-1
Reference 8: http://www.xbrl.org/2003/role/disclosureRef
-Topic 470
-SubTopic 20
-Name Accounting Standards Codification
-Section 50
-Paragraph 4
-Subparagraph (b)(3)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147481139/470-20-50-4
| Name: |
us-gaap_LongTermDebt |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:monetaryItemType |
| Balance Type: |
credit |
| Period Type: |
instant |
|
| X |
- DefinitionAmount, after deduction of unamortized premium (discount) and debt issuance cost, of long-term debt classified as current. Excludes lease obligation. Reference 1: http://www.xbrl.org/2003/role/disclosureRef
-Topic 210
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.5-02(20))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480566/210-10-S99-1
| Name: |
us-gaap_LongTermDebtCurrent |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:monetaryItemType |
| Balance Type: |
credit |
| Period Type: |
instant |
|
| X |
- DefinitionAmount, after deduction of unamortized premium (discount) and debt issuance cost, of long-term debt classified as noncurrent. Excludes lease obligation. Reference 1: http://www.xbrl.org/2003/role/disclosureRef
-Topic 210
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.5-02(22))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480566/210-10-S99-1
| Name: |
us-gaap_LongTermDebtNoncurrent |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:monetaryItemType |
| Balance Type: |
credit |
| Period Type: |
instant |
|
v3.24.2.u1
Long-Term Debt - Additional Information (Details) - USD ($)
$ in Thousands |
|
|
3 Months Ended |
6 Months Ended |
|
Jun. 14, 2024 |
Sep. 02, 2022 |
Jun. 30, 2024 |
Jun. 30, 2024 |
Jun. 30, 2023 |
Dec. 31, 2023 |
| Debt Instrument [Line Items] |
|
|
|
|
|
|
| Long-term debt |
|
|
$ 215,000
|
$ 215,000
|
|
$ 165,000
|
| Proceeds from long-term debt |
|
|
|
50,000
|
$ 0
|
|
| Debt issuance costs |
|
|
|
$ 512
|
$ 0
|
|
| Secured Debt | Minimum |
|
|
|
|
|
|
| Debt Instrument [Line Items] |
|
|
|
|
|
|
| Prepayment fee |
|
1.00%
|
|
|
|
|
| Oxford Term Loan | Secured Debt |
|
|
|
|
|
|
| Debt Instrument [Line Items] |
|
|
|
|
|
|
| Debt instrument, face amount |
|
$ 250,000
|
|
|
|
|
| Long-term debt |
|
$ 165,000
|
|
|
|
|
| Debt interest floor rate |
|
6.50%
|
|
|
|
|
| Commitment fee |
|
$ 1,650
|
|
|
|
|
| Debt instrument origination fee |
|
$ 1,650
|
|
|
|
|
| Accrual interest rate on default |
|
2.00%
|
|
|
|
|
| Repayment limit on net proceeds from sale of asset |
|
$ 2,500
|
|
|
|
|
| Minimum liquidity in the loan agreement |
|
$ 23,000
|
|
|
|
|
| Oxford Term Loan | Secured Debt | Minimum |
|
|
|
|
|
|
| Debt Instrument [Line Items] |
|
|
|
|
|
|
| Interest rate during period |
|
|
|
11.82%
|
|
|
| Oxford Term Loan | Secured Debt | Maximum |
|
|
|
|
|
|
| Debt Instrument [Line Items] |
|
|
|
|
|
|
| Interest rate during period |
|
|
11.85%
|
|
|
|
| Oxford Term Loan | Secured Debt | Base Rate |
|
|
|
|
|
|
| Debt Instrument [Line Items] |
|
|
|
|
|
|
| Debt interest floor rate |
|
1.00%
|
|
|
|
|
| Delayed Draw Term Loan |
|
|
|
|
|
|
| Debt Instrument [Line Items] |
|
|
|
|
|
|
| Unused borrowing capacity, amount |
|
|
$ 35
|
$ 35
|
|
|
| Delayed Draw Term Loan | Secured Debt |
|
|
|
|
|
|
| Debt Instrument [Line Items] |
|
|
|
|
|
|
| Additional term loan amount |
|
$ 85,000
|
|
|
|
|
| Proceeds from long-term debt |
$ 50,000
|
|
|
|
|
|
| Commitment fee |
|
850
|
|
|
|
|
| Debt instrument origination fee |
|
500
|
|
|
|
|
| Debt issuance costs |
|
$ 1,096
|
|
|
|
|
| X |
- DefinitionDebt instrument default accrual interest rate.
| Name: |
alhc_DebtInstrumentDefaultAccrualInterestRate |
| Namespace Prefix: |
alhc_ |
| Data Type: |
dtr-types:percentItemType |
| Balance Type: |
na |
| Period Type: |
instant |
|
| X |
- DefinitionDebt instrument minimum liquidity
| Name: |
alhc_DebtInstrumentMinimumLiquidity |
| Namespace Prefix: |
alhc_ |
| Data Type: |
xbrli:monetaryItemType |
| Balance Type: |
debit |
| Period Type: |
instant |
|
| X |
- DefinitionDebt instrument prepayment fee.
| Name: |
alhc_DebtInstrumentPrepaymentFee |
| Namespace Prefix: |
alhc_ |
| Data Type: |
dtr-types:percentItemType |
| Balance Type: |
na |
| Period Type: |
instant |
|
| X |
- DefinitionLong term debt commitment fee.
| Name: |
alhc_LongTermDebtCommitmentFee |
| Namespace Prefix: |
alhc_ |
| Data Type: |
xbrli:monetaryItemType |
| Balance Type: |
debit |
| Period Type: |
instant |
|
| X |
- DefinitionRepayment limit on net proceeds from sale of asset.
| Name: |
alhc_RepaymentLimitOnNetProceedsFromSaleOfAsset |
| Namespace Prefix: |
alhc_ |
| Data Type: |
xbrli:monetaryItemType |
| Balance Type: |
debit |
| Period Type: |
duration |
|
| X |
- DefinitionPercentage points added to the reference rate to compute the variable rate on the debt instrument.
| Name: |
us-gaap_DebtInstrumentBasisSpreadOnVariableRate1 |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
dtr-types:percentItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionAmount, before unamortized (discount) premium and debt issuance costs, of long-term debt. Includes, but is not limited to, notes payable, bonds payable, commercial loans, mortgage loans, convertible debt, subordinated debt and other types of debt. Reference 1: http://fasb.org/us-gaap/role/ref/legacyRef
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.5-02(22))
-SubTopic 10
-Topic 210
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480566/210-10-S99-1
Reference 2: http://fasb.org/us-gaap/role/ref/legacyRef
-Topic 942
-SubTopic 210
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.9-03(16))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147478546/942-210-S99-1
Reference 3: http://www.xbrl.org/2003/role/disclosureRef
-Topic 470
-SubTopic 20
-Name Accounting Standards Codification
-Section 50
-Paragraph 4
-Subparagraph (b)(1)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147481139/470-20-50-4
| Name: |
us-gaap_DebtInstrumentCarryingAmount |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:monetaryItemType |
| Balance Type: |
credit |
| Period Type: |
instant |
|
| X |
- DefinitionFace (par) amount of debt instrument at time of issuance. Reference 1: http://www.xbrl.org/2003/role/exampleRef
-Topic 835
-SubTopic 30
-Name Accounting Standards Codification
-Section 55
-Paragraph 8
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482949/835-30-55-8
Reference 2: http://www.xbrl.org/2003/role/disclosureRef
-Topic 470
-SubTopic 20
-Name Accounting Standards Codification
-Section 50
-Paragraph 1B
-Subparagraph (a)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147481139/470-20-50-1B
Reference 3: http://www.xbrl.org/2003/role/exampleRef
-Topic 470
-SubTopic 20
-Name Accounting Standards Codification
-Section 55
-Paragraph 69B
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147481568/470-20-55-69B
Reference 4: http://www.xbrl.org/2003/role/exampleRef
-Topic 470
-SubTopic 20
-Name Accounting Standards Codification
-Section 55
-Paragraph 69C
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147481568/470-20-55-69C
Reference 5: http://www.xbrl.org/2003/role/disclosureRef
-Topic 835
-SubTopic 30
-Name Accounting Standards Codification
-Section 50
-Paragraph 1
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482900/835-30-50-1
Reference 6: http://www.xbrl.org/2003/role/disclosureRef
-Topic 835
-SubTopic 30
-Name Accounting Standards Codification
-Section 45
-Paragraph 2
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482925/835-30-45-2
| Name: |
us-gaap_DebtInstrumentFaceAmount |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:monetaryItemType |
| Balance Type: |
credit |
| Period Type: |
instant |
|
| X |
- DefinitionAmount of the fee that accompanies borrowing money under the debt instrument. Reference 1: http://fasb.org/us-gaap/role/ref/legacyRef
-Topic 210
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.5-02(22)(b))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480566/210-10-S99-1
| Name: |
us-gaap_DebtInstrumentFeeAmount |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:monetaryItemType |
| Balance Type: |
debit |
| Period Type: |
instant |
|
| X |
- DefinitionThe average effective interest rate during the reporting period. Reference 1: http://fasb.org/us-gaap/role/ref/legacyRef
-Topic 210
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.5-02(22)(a)(1))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480566/210-10-S99-1
Reference 2: http://www.xbrl.org/2003/role/disclosureRef
-Topic 470
-SubTopic 20
-Name Accounting Standards Codification
-Section 50
-Paragraph 1F
-Subparagraph (a)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147481139/470-20-50-1F
Reference 3: http://www.xbrl.org/2009/role/commonPracticeRef
-Topic 835
-SubTopic 30
-Name Accounting Standards Codification
-Section 45
-Paragraph 2
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482925/835-30-45-2
| Name: |
us-gaap_DebtInstrumentInterestRateDuringPeriod |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
dtr-types:percentItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionLine items represent financial concepts included in a table. These concepts are used to disclose reportable information associated with domain members defined in one or many axes to the table. Reference 1: http://www.xbrl.org/2003/role/exampleRef
-Topic 835
-SubTopic 30
-Name Accounting Standards Codification
-Section 55
-Paragraph 8
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482949/835-30-55-8
Reference 2: http://www.xbrl.org/2009/role/commonPracticeRef
-Topic 235
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.4-08(f))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480678/235-10-S99-1
Reference 3: http://www.xbrl.org/2003/role/disclosureRef
-Topic 235
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 3
-Subparagraph (SX 210.12-04(a))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480678/235-10-S99-3
Reference 4: http://www.xbrl.org/2003/role/disclosureRef
-Topic 470
-SubTopic 20
-Name Accounting Standards Codification
-Section 50
-Paragraph 1B
-Subparagraph (a)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147481139/470-20-50-1B
Reference 5: http://www.xbrl.org/2003/role/exampleRef
-Topic 470
-SubTopic 20
-Name Accounting Standards Codification
-Section 55
-Paragraph 69B
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147481568/470-20-55-69B
Reference 6: http://www.xbrl.org/2003/role/exampleRef
-Topic 470
-SubTopic 20
-Name Accounting Standards Codification
-Section 55
-Paragraph 69C
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147481568/470-20-55-69C
Reference 7: http://www.xbrl.org/2003/role/exampleRef
-Topic 470
-SubTopic 20
-Name Accounting Standards Codification
-Section 55
-Paragraph 69E
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147481568/470-20-55-69E
Reference 8: http://www.xbrl.org/2003/role/exampleRef
-Topic 470
-SubTopic 20
-Name Accounting Standards Codification
-Section 55
-Paragraph 69F
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147481568/470-20-55-69F
Reference 9: http://www.xbrl.org/2003/role/disclosureRef
-Topic 470
-SubTopic 20
-Name Accounting Standards Codification
-Section 50
-Paragraph 1B
-Subparagraph (b)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147481139/470-20-50-1B
Reference 10: http://www.xbrl.org/2003/role/disclosureRef
-Topic 470
-SubTopic 20
-Name Accounting Standards Codification
-Section 50
-Paragraph 1B
-Subparagraph (c)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147481139/470-20-50-1B
Reference 11: http://www.xbrl.org/2003/role/exampleRef
-Topic 470
-SubTopic 20
-Name Accounting Standards Codification
-Section 50
-Paragraph 1B
-Subparagraph (d)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147481139/470-20-50-1B
Reference 12: http://www.xbrl.org/2003/role/disclosureRef
-Topic 470
-SubTopic 20
-Name Accounting Standards Codification
-Section 50
-Paragraph 1B
-Subparagraph (e)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147481139/470-20-50-1B
Reference 13: http://www.xbrl.org/2003/role/disclosureRef
-Topic 470
-SubTopic 20
-Name Accounting Standards Codification
-Section 50
-Paragraph 1B
-Subparagraph (f)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147481139/470-20-50-1B
Reference 14: http://www.xbrl.org/2003/role/disclosureRef
-Topic 470
-SubTopic 20
-Name Accounting Standards Codification
-Section 50
-Paragraph 1B
-Subparagraph (h)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147481139/470-20-50-1B
Reference 15: http://www.xbrl.org/2003/role/disclosureRef
-Topic 470
-SubTopic 20
-Name Accounting Standards Codification
-Section 50
-Paragraph 1D
-Subparagraph (a)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147481139/470-20-50-1D
Reference 16: http://www.xbrl.org/2003/role/disclosureRef
-Topic 470
-SubTopic 20
-Name Accounting Standards Codification
-Section 50
-Paragraph 1D
-Subparagraph (b)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147481139/470-20-50-1D
Reference 17: http://www.xbrl.org/2003/role/disclosureRef
-Topic 470
-SubTopic 20
-Name Accounting Standards Codification
-Section 50
-Paragraph 1D
-Subparagraph (c)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147481139/470-20-50-1D
Reference 18: http://www.xbrl.org/2003/role/disclosureRef
-Topic 470
-SubTopic 20
-Name Accounting Standards Codification
-Section 50
-Paragraph 1E
-Subparagraph (a)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147481139/470-20-50-1E
Reference 19: http://www.xbrl.org/2003/role/disclosureRef
-Topic 470
-SubTopic 20
-Name Accounting Standards Codification
-Section 50
-Paragraph 1E
-Subparagraph (c)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147481139/470-20-50-1E
Reference 20: http://www.xbrl.org/2003/role/disclosureRef
-Topic 470
-SubTopic 20
-Name Accounting Standards Codification
-Section 50
-Paragraph 1E
-Subparagraph (d)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147481139/470-20-50-1E
Reference 21: http://www.xbrl.org/2003/role/disclosureRef
-Topic 470
-SubTopic 20
-Name Accounting Standards Codification
-Section 50
-Paragraph 1F
-Subparagraph (a)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147481139/470-20-50-1F
Reference 22: http://www.xbrl.org/2003/role/disclosureRef
-Topic 470
-SubTopic 20
-Name Accounting Standards Codification
-Section 50
-Paragraph 1F
-Subparagraph (b)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147481139/470-20-50-1F
Reference 23: http://www.xbrl.org/2003/role/disclosureRef
-Topic 470
-SubTopic 20
-Name Accounting Standards Codification
-Section 50
-Paragraph 1F
-Subparagraph (b)(1)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147481139/470-20-50-1F
Reference 24: http://www.xbrl.org/2003/role/disclosureRef
-Topic 470
-SubTopic 20
-Name Accounting Standards Codification
-Section 50
-Paragraph 1F
-Subparagraph (b)(2)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147481139/470-20-50-1F
Reference 25: http://www.xbrl.org/2003/role/disclosureRef
-Topic 470
-SubTopic 20
-Name Accounting Standards Codification
-Section 50
-Paragraph 1I
-Subparagraph (c)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147481139/470-20-50-1I
Reference 26: http://www.xbrl.org/2009/role/commonPracticeRef
-Topic 835
-SubTopic 30
-Name Accounting Standards Codification
-Section 45
-Paragraph 2
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482925/835-30-45-2
Reference 27: http://www.xbrl.org/2009/role/commonPracticeRef
-Topic 835
-SubTopic 30
-Name Accounting Standards Codification
-Section 50
-Paragraph 1
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482900/835-30-50-1
| Name: |
us-gaap_DebtInstrumentLineItems |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:stringItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionAmount of unused borrowing capacity under the long-term financing arrangement that is available to the entity as of the balance sheet date. Reference 1: http://www.xbrl.org/2003/role/disclosureRef
-Topic 470
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 6
-Subparagraph (a)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147481544/470-10-50-6
Reference 2: http://fasb.org/us-gaap/role/ref/legacyRef
-Topic 210
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.5-02(22)(b))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480566/210-10-S99-1
| Name: |
us-gaap_DebtInstrumentUnusedBorrowingCapacityAmount |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:monetaryItemType |
| Balance Type: |
credit |
| Period Type: |
instant |
|
| X |
- DefinitionAverage amount outstanding of long-term debt. Reference 1: http://www.xbrl.org/2003/role/disclosureRef
-Name Regulation S-K (SK)
-Number 229
-Section 1402
-Paragraph a
-Publisher SEC
Reference 2: http://www.xbrl.org/2003/role/disclosureRef
-Name Regulation S-K (SK)
-Number 229
-Section 1402
-Paragraph b
-Subparagraph (1)
-Publisher SEC
Reference 3: http://www.xbrl.org/2003/role/disclosureRef
-Topic 946
-SubTopic 220
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.6-07(3))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147479134/946-220-S99-1
| Name: |
us-gaap_LongTermDebtAverageAmountOutstanding |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:monetaryItemType |
| Balance Type: |
credit |
| Period Type: |
duration |
|
| X |
- DefinitionThe cash outflow paid to third parties in connection with debt origination, which will be amortized over the remaining maturity period of the associated long-term debt. Reference 1: http://fasb.org/us-gaap/role/ref/legacyRef
-Name Accounting Standards Codification
-Topic 230
-SubTopic 10
-Section 45
-Paragraph 15
-Subparagraph (e)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482740/230-10-45-15
| Name: |
us-gaap_PaymentsOfDebtIssuanceCosts |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:monetaryItemType |
| Balance Type: |
credit |
| Period Type: |
duration |
|
| X |
- DefinitionThe cash inflow from a debt initially having maturity due after one year or beyond the operating cycle, if longer. Reference 1: http://www.xbrl.org/2003/role/disclosureRef
-Topic 946
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 3
-Subparagraph (SX 210.6-03(i)(1))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147479886/946-10-S99-3
Reference 2: http://fasb.org/us-gaap/role/ref/legacyRef
-Name Accounting Standards Codification
-Topic 230
-SubTopic 10
-Section 45
-Paragraph 14
-Subparagraph (b)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482740/230-10-45-14
| Name: |
us-gaap_ProceedsFromIssuanceOfLongTermDebt |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:monetaryItemType |
| Balance Type: |
debit |
| Period Type: |
duration |
|
| X |
- Details
| Name: |
us-gaap_LongtermDebtTypeAxis=us-gaap_SecuredDebtMember |
| Namespace Prefix: |
|
| Data Type: |
na |
| Balance Type: |
|
| Period Type: |
|
|
| X |
- Details
| Name: |
srt_RangeAxis=srt_MinimumMember |
| Namespace Prefix: |
|
| Data Type: |
na |
| Balance Type: |
|
| Period Type: |
|
|
| X |
- Details
| Name: |
us-gaap_DebtInstrumentAxis=alhc_OxfordTermLoanMember |
| Namespace Prefix: |
|
| Data Type: |
na |
| Balance Type: |
|
| Period Type: |
|
|
| X |
- Details
| Name: |
srt_RangeAxis=srt_MaximumMember |
| Namespace Prefix: |
|
| Data Type: |
na |
| Balance Type: |
|
| Period Type: |
|
|
| X |
- Details
| Name: |
us-gaap_VariableRateAxis=us-gaap_BaseRateMember |
| Namespace Prefix: |
|
| Data Type: |
na |
| Balance Type: |
|
| Period Type: |
|
|
| X |
- Details
| Name: |
us-gaap_DebtInstrumentAxis=us-gaap_DelayedDrawTermLoanMember |
| Namespace Prefix: |
|
| Data Type: |
na |
| Balance Type: |
|
| Period Type: |
|
|
v3.24.2.u1
| X |
- References
+ Details
| Name: |
us-gaap_DebtDisclosureAbstract |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:stringItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionAmount, before unamortized (discount) premium and debt issuance costs, of long-term debt. Includes, but is not limited to, notes payable, bonds payable, commercial loans, mortgage loans, convertible debt, subordinated debt and other types of debt. Reference 1: http://fasb.org/us-gaap/role/ref/legacyRef
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.5-02(22))
-SubTopic 10
-Topic 210
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480566/210-10-S99-1
Reference 2: http://fasb.org/us-gaap/role/ref/legacyRef
-Topic 942
-SubTopic 210
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.9-03(16))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147478546/942-210-S99-1
Reference 3: http://www.xbrl.org/2003/role/disclosureRef
-Topic 470
-SubTopic 20
-Name Accounting Standards Codification
-Section 50
-Paragraph 4
-Subparagraph (b)(1)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147481139/470-20-50-4
| Name: |
us-gaap_DebtInstrumentCarryingAmount |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:monetaryItemType |
| Balance Type: |
credit |
| Period Type: |
instant |
|
| X |
- DefinitionAmount of long-term debt payable, sinking fund requirement, and other securities issued that are redeemable by holder at fixed or determinable price and date, maturing in next fiscal year following current fiscal year. Excludes interim and annual periods when interim periods are reported from current statement of financial position date (rolling approach). Reference 1: http://www.xbrl.org/2003/role/disclosureRef
-Topic 235
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 3
-Subparagraph (SX 210.12-04(a))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480678/235-10-S99-3
Reference 2: http://www.xbrl.org/2003/role/disclosureRef
-Topic 470
-SubTopic 20
-Name Accounting Standards Codification
-Section 50
-Paragraph 1E
-Subparagraph (d)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147481139/470-20-50-1E
Reference 3: http://fasb.org/us-gaap/role/ref/legacyRef
-Name Accounting Standards Codification
-Section 50
-Paragraph 1
-SubTopic 10
-Topic 470
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147481544/470-10-50-1
| Name: |
us-gaap_LongTermDebtMaturitiesRepaymentsOfPrincipalInNextTwelveMonths |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:monetaryItemType |
| Balance Type: |
credit |
| Period Type: |
instant |
|
| X |
- DefinitionAmount of long-term debt payable, sinking fund requirement, and other securities issued that are redeemable by holder at fixed or determinable price and date, maturing in fourth fiscal year following current fiscal year. Excludes interim and annual periods when interim periods are reported from current statement of financial position date (rolling approach). Reference 1: http://www.xbrl.org/2003/role/disclosureRef
-Topic 235
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 3
-Subparagraph (SX 210.12-04(a))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480678/235-10-S99-3
Reference 2: http://www.xbrl.org/2003/role/disclosureRef
-Topic 470
-SubTopic 20
-Name Accounting Standards Codification
-Section 50
-Paragraph 1E
-Subparagraph (d)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147481139/470-20-50-1E
Reference 3: http://fasb.org/us-gaap/role/ref/legacyRef
-Name Accounting Standards Codification
-Section 50
-Paragraph 1
-SubTopic 10
-Topic 470
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147481544/470-10-50-1
| Name: |
us-gaap_LongTermDebtMaturitiesRepaymentsOfPrincipalInYearFour |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:monetaryItemType |
| Balance Type: |
credit |
| Period Type: |
instant |
|
| X |
- DefinitionAmount of long-term debt payable, sinking fund requirement, and other securities issued that are redeemable by holder at fixed or determinable price and date, maturing in third fiscal year following current fiscal year. Excludes interim and annual periods when interim periods are reported from current statement of financial position date (rolling approach). Reference 1: http://www.xbrl.org/2003/role/disclosureRef
-Topic 235
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 3
-Subparagraph (SX 210.12-04(a))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480678/235-10-S99-3
Reference 2: http://www.xbrl.org/2003/role/disclosureRef
-Topic 470
-SubTopic 20
-Name Accounting Standards Codification
-Section 50
-Paragraph 1E
-Subparagraph (d)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147481139/470-20-50-1E
Reference 3: http://fasb.org/us-gaap/role/ref/legacyRef
-Name Accounting Standards Codification
-Section 50
-Paragraph 1
-SubTopic 10
-Topic 470
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147481544/470-10-50-1
| Name: |
us-gaap_LongTermDebtMaturitiesRepaymentsOfPrincipalInYearThree |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:monetaryItemType |
| Balance Type: |
credit |
| Period Type: |
instant |
|
| X |
- DefinitionAmount of long-term debt payable, sinking fund requirement, and other securities issued that are redeemable by holder at fixed or determinable price and date, maturing in second fiscal year following current fiscal year. Excludes interim and annual periods when interim periods are reported from current statement of financial position date (rolling approach). Reference 1: http://www.xbrl.org/2003/role/disclosureRef
-Topic 235
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 3
-Subparagraph (SX 210.12-04(a))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480678/235-10-S99-3
Reference 2: http://www.xbrl.org/2003/role/disclosureRef
-Topic 470
-SubTopic 20
-Name Accounting Standards Codification
-Section 50
-Paragraph 1E
-Subparagraph (d)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147481139/470-20-50-1E
Reference 3: http://fasb.org/us-gaap/role/ref/legacyRef
-Name Accounting Standards Codification
-Section 50
-Paragraph 1
-SubTopic 10
-Topic 470
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147481544/470-10-50-1
| Name: |
us-gaap_LongTermDebtMaturitiesRepaymentsOfPrincipalInYearTwo |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:monetaryItemType |
| Balance Type: |
credit |
| Period Type: |
instant |
|
| X |
- DefinitionAmount of long-term debt payable, sinking fund requirement, and other securities issued that are redeemable by holder at fixed or determinable price and date, maturing in remainder of current fiscal year. Reference 1: http://www.xbrl.org/2009/role/commonPracticeRef
-Topic 235
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 3
-Subparagraph (SX 210.12-04(a))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480678/235-10-S99-3
| Name: |
us-gaap_LongTermDebtMaturitiesRepaymentsOfPrincipalRemainderOfFiscalYear |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:monetaryItemType |
| Balance Type: |
credit |
| Period Type: |
instant |
|
v3.24.2.u1
| X |
- DefinitionCarryforward offset percentage of taxable income.
| Name: |
alhc_CarryforwardOffsetPercentageOfTaxableIncome |
| Namespace Prefix: |
alhc_ |
| Data Type: |
dtr-types:percentItemType |
| Balance Type: |
na |
| Period Type: |
instant |
|
| X |
- DefinitionOperating loss carryforward indefinite life.
| Name: |
alhc_OperatingLossCarryforwardIndefiniteLife |
| Namespace Prefix: |
alhc_ |
| Data Type: |
xbrli:monetaryItemType |
| Balance Type: |
debit |
| Period Type: |
instant |
|
| X |
- DefinitionOperating loss carryforwards expiration year.
| Name: |
alhc_OperatingLossCarryforwardsExpirationYear |
| Namespace Prefix: |
alhc_ |
| Data Type: |
xbrli:gYearItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionTaxable income deduction limit percentage.
| Name: |
alhc_TaxableIncomeDeductionLimitPercentage |
| Namespace Prefix: |
alhc_ |
| Data Type: |
dtr-types:percentItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionAmount of operating loss carryforward, before tax effects, available to reduce future taxable income under enacted tax laws. Reference 1: http://www.xbrl.org/2003/role/disclosureRef
-Topic 740
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 3
-Subparagraph (a)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482685/740-10-50-3
| Name: |
us-gaap_OperatingLossCarryforwards |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:monetaryItemType |
| Balance Type: |
debit |
| Period Type: |
instant |
|
| X |
- DefinitionLine items represent financial concepts included in a table. These concepts are used to disclose reportable information associated with domain members defined in one or many axes to the table. Reference 1: http://www.xbrl.org/2003/role/disclosureRef
-Topic 740
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 3
-Subparagraph (a)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147482685/740-10-50-3
| Name: |
us-gaap_OperatingLossCarryforwardsLineItems |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:stringItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- Details
| Name: |
srt_ConsolidatedEntitiesAxis=srt_SubsidiariesMember |
| Namespace Prefix: |
|
| Data Type: |
na |
| Balance Type: |
|
| Period Type: |
|
|
v3.24.2.u1
Equity-Based Compensation - Additional Information (Details) - USD ($)
|
|
|
|
|
|
3 Months Ended |
6 Months Ended |
|
|
Mar. 01, 2027 |
Dec. 31, 2025 |
Mar. 01, 2025 |
Mar. 13, 2024 |
Sep. 14, 2023 |
Jun. 30, 2024 |
Jun. 30, 2023 |
Jun. 30, 2024 |
Jun. 30, 2023 |
Dec. 31, 2026 |
Dec. 31, 2024 |
| Share Based Compensation Arrangement by Share Based Payment Award [Line Items] |
|
|
|
|
|
|
|
|
|
|
|
| Aggregate intrinsic value, options exercised |
|
|
|
|
|
$ 0
|
$ 0
|
$ 0
|
$ 0
|
|
|
| Options granted, fair value |
|
|
|
|
|
$ 0
|
|
0
|
|
|
|
| Share based compensation expense, unrecognized |
|
|
|
|
|
|
|
$ 93,667,000
|
|
|
|
| Stock Options |
|
|
|
|
|
|
|
|
|
|
|
| Share Based Compensation Arrangement by Share Based Payment Award [Line Items] |
|
|
|
|
|
|
|
|
|
|
|
| Annual award vesting rights, percentage |
|
|
|
|
|
|
|
25.00%
|
|
|
|
| Award vesting period |
|
|
|
|
|
|
|
4 years
|
|
|
|
| Award expiration period |
|
|
|
|
|
|
|
10 years
|
|
|
|
| Restricted Stock Awards |
|
|
|
|
|
|
|
|
|
|
|
| Share Based Compensation Arrangement by Share Based Payment Award [Line Items] |
|
|
|
|
|
|
|
|
|
|
|
| Annual award vesting rights, percentage |
|
|
|
|
|
|
|
25.00%
|
|
|
|
| Award vesting period |
|
|
|
|
|
|
|
4 years
|
|
|
|
| Pre-IPO Awards Converted RSAs |
|
|
|
|
|
|
|
|
|
|
|
| Share Based Compensation Arrangement by Share Based Payment Award [Line Items] |
|
|
|
|
|
|
|
|
|
|
|
| Annual award vesting rights, percentage |
|
|
|
|
|
|
|
50.00%
|
|
|
|
| RSUs |
|
|
|
|
|
|
|
|
|
|
|
| Share Based Compensation Arrangement by Share Based Payment Award [Line Items] |
|
|
|
|
|
|
|
|
|
|
|
| Annual award vesting rights, percentage |
|
|
|
|
|
|
|
25.00%
|
|
|
|
| Award vesting period |
|
|
|
|
|
|
|
4 years
|
|
|
|
| Performance-based Restricted Stock Units | Scenario Forecast |
|
|
|
|
|
|
|
|
|
|
|
| Share Based Compensation Arrangement by Share Based Payment Award [Line Items] |
|
|
|
|
|
|
|
|
|
|
|
| Annual award vesting rights, percentage |
100.00%
|
50.00%
|
50.00%
|
|
|
|
|
|
|
|
|
| Performance target, health plan revenue growth percentage |
|
|
|
|
|
|
|
|
|
50.00%
|
60.00%
|
| Performance target, returning member medical benefit ratio |
|
|
|
|
|
|
|
|
|
|
0.20
|
| Performance target, adjusted earnings before interest, less capital expenditures |
|
|
|
|
|
|
|
|
|
|
20.00%
|
| Performance target, adjusted earnings before interest |
|
|
|
|
|
|
|
|
|
50.00%
|
|
| Performance-based Restricted Stock Units | Minimum |
|
|
|
|
|
|
|
|
|
|
|
| Share Based Compensation Arrangement by Share Based Payment Award [Line Items] |
|
|
|
|
|
|
|
|
|
|
|
| Annual award vesting rights, percentage |
|
|
|
0.00%
|
0.00%
|
|
|
|
|
|
|
| Performance-based Restricted Stock Units | Maximum |
|
|
|
|
|
|
|
|
|
|
|
| Share Based Compensation Arrangement by Share Based Payment Award [Line Items] |
|
|
|
|
|
|
|
|
|
|
|
| Annual award vesting rights, percentage |
|
|
|
200.00%
|
150.00%
|
|
|
|
|
|
|
| Non-vested awards RSAs, options and RSUs |
|
|
|
|
|
|
|
|
|
|
|
| Share Based Compensation Arrangement by Share Based Payment Award [Line Items] |
|
|
|
|
|
|
|
|
|
|
|
| Weighted average contractual term |
|
|
|
|
|
|
|
1 year 8 months 12 days
|
|
|
|
| X |
- DefinitionShare-based compensation arrangement by share-based payment award, options, grants in period, fair value.
| Name: |
alhc_ShareBasedCompensationArrangementByShareBasedPaymentAwardOptionsGrantsInPeriodFairValue |
| Namespace Prefix: |
alhc_ |
| Data Type: |
xbrli:monetaryItemType |
| Balance Type: |
credit |
| Period Type: |
duration |
|
| X |
- DefinitionShare-based Compensation Arrangement by Share-based Payment Award, Options, Nonvested, Weighted Average Contractual Term
| Name: |
alhc_ShareBasedCompensationArrangementByShareBasedPaymentAwardOptionsNonvestedWeightedAverageContractualTerm |
| Namespace Prefix: |
alhc_ |
| Data Type: |
xbrli:durationItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionShare Based Compensation Expense, Unrecognized
| Name: |
alhc_ShareBasedCompensationExpenseUnrecognized |
| Namespace Prefix: |
alhc_ |
| Data Type: |
xbrli:monetaryItemType |
| Balance Type: |
debit |
| Period Type: |
duration |
|
| X |
- DefinitionPeriod over which grantee's right to exercise award under share-based payment arrangement is no longer contingent on satisfaction of service or performance condition, in 'PnYnMnDTnHnMnS' format, for example, 'P1Y5M13D' represents reported fact of one year, five months, and thirteen days. Includes, but is not limited to, combination of market, performance or service condition. Reference 1: http://www.xbrl.org/2003/role/exampleRef
-Topic 718
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 2
-Subparagraph (a)(1)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480429/718-10-50-2
| Name: |
us-gaap_ShareBasedCompensationArrangementByShareBasedPaymentAwardAwardVestingPeriod1 |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:durationItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionLine items represent financial concepts included in a table. These concepts are used to disclose reportable information associated with domain members defined in one or many axes to the table. Reference 1: http://www.xbrl.org/2003/role/disclosureRef
-Topic 718
-SubTopic 10
-Name Accounting Standards Codification
-Section 35
-Paragraph 1D
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480483/718-10-35-1D
Reference 2: http://www.xbrl.org/2003/role/disclosureRef
-Topic 718
-SubTopic 10
-Name Accounting Standards Codification
-Section 35
-Paragraph 3
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480483/718-10-35-3
Reference 3: http://www.xbrl.org/2003/role/disclosureRef
-Topic 718
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 2
-Subparagraph (a)(1)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480429/718-10-50-2
Reference 4: http://www.xbrl.org/2003/role/disclosureRef
-Topic 718
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 2
-Subparagraph (a)(2)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480429/718-10-50-2
Reference 5: http://www.xbrl.org/2003/role/disclosureRef
-Topic 718
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 2
-Subparagraph (a)(3)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480429/718-10-50-2
Reference 6: http://www.xbrl.org/2003/role/disclosureRef
-Topic 718
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 2
-Subparagraph (c)(1)(i)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480429/718-10-50-2
Reference 7: http://www.xbrl.org/2003/role/disclosureRef
-Topic 718
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 2
-Subparagraph (c)(1)(ii)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480429/718-10-50-2
Reference 8: http://www.xbrl.org/2003/role/disclosureRef
-Topic 718
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 2
-Subparagraph (c)(1)(iii)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480429/718-10-50-2
Reference 9: http://www.xbrl.org/2003/role/disclosureRef
-Topic 718
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 2
-Subparagraph (c)(1)(iv)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480429/718-10-50-2
Reference 10: http://www.xbrl.org/2003/role/disclosureRef
-Topic 718
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 2
-Subparagraph (c)(1)(iv)(01)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480429/718-10-50-2
Reference 11: http://www.xbrl.org/2003/role/disclosureRef
-Topic 718
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 2
-Subparagraph (c)(1)(iv)(02)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480429/718-10-50-2
Reference 12: http://www.xbrl.org/2003/role/disclosureRef
-Topic 718
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 2
-Subparagraph (c)(1)(iv)(03)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480429/718-10-50-2
Reference 13: http://www.xbrl.org/2003/role/disclosureRef
-Topic 718
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 2
-Subparagraph (c)(1)(iv)(04)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480429/718-10-50-2
Reference 14: http://www.xbrl.org/2003/role/disclosureRef
-Topic 718
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 2
-Subparagraph (c)(2)(i)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480429/718-10-50-2
Reference 15: http://www.xbrl.org/2003/role/disclosureRef
-Topic 718
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 2
-Subparagraph (c)(2)(ii)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480429/718-10-50-2
Reference 16: http://www.xbrl.org/2003/role/disclosureRef
-Topic 718
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 2
-Subparagraph (c)(2)(iii)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480429/718-10-50-2
Reference 17: http://www.xbrl.org/2003/role/disclosureRef
-Topic 718
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 2
-Subparagraph (c)(2)(iii)(01)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480429/718-10-50-2
Reference 18: http://www.xbrl.org/2003/role/disclosureRef
-Topic 718
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 2
-Subparagraph (c)(2)(iii)(02)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480429/718-10-50-2
Reference 19: http://www.xbrl.org/2003/role/disclosureRef
-Topic 718
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 2
-Subparagraph (c)(2)(iii)(03)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480429/718-10-50-2
Reference 20: http://www.xbrl.org/2003/role/disclosureRef
-Topic 718
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 2
-Subparagraph (d)(1)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480429/718-10-50-2
Reference 21: http://www.xbrl.org/2003/role/disclosureRef
-Topic 718
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 2
-Subparagraph (d)(2)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480429/718-10-50-2
Reference 22: http://www.xbrl.org/2003/role/disclosureRef
-Topic 718
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 2
-Subparagraph (e)(1)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480429/718-10-50-2
Reference 23: http://www.xbrl.org/2003/role/disclosureRef
-Topic 718
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 2
-Subparagraph (e)(2)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480429/718-10-50-2
Reference 24: http://www.xbrl.org/2003/role/disclosureRef
-Topic 718
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 2
-Subparagraph (f)(2)(i)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480429/718-10-50-2
Reference 25: http://www.xbrl.org/2003/role/disclosureRef
-Topic 718
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 2
-Subparagraph (f)(2)(ii)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480429/718-10-50-2
Reference 26: http://www.xbrl.org/2003/role/disclosureRef
-Topic 718
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 2
-Subparagraph (f)(2)(iii)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480429/718-10-50-2
Reference 27: http://www.xbrl.org/2003/role/disclosureRef
-Topic 718
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 2
-Subparagraph (f)(2)(iv)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480429/718-10-50-2
Reference 28: http://www.xbrl.org/2003/role/disclosureRef
-Topic 718
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 2
-Subparagraph (f)(2)(v)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480429/718-10-50-2
| Name: |
us-gaap_ShareBasedCompensationArrangementByShareBasedPaymentAwardLineItems |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:stringItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionAmount of accumulated difference between fair value of underlying shares on dates of exercise and exercise price on options exercised (or share units converted) into shares. Reference 1: http://www.xbrl.org/2003/role/disclosureRef
-Topic 718
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 2
-Subparagraph (d)(2)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480429/718-10-50-2
| Name: |
us-gaap_ShareBasedCompensationArrangementByShareBasedPaymentAwardOptionsExercisesInPeriodTotalIntrinsicValue |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:monetaryItemType |
| Balance Type: |
debit |
| Period Type: |
duration |
|
| X |
- DefinitionPercentage of vesting of award under share-based payment arrangement. Reference 1: http://www.xbrl.org/2009/role/commonPracticeRef
-Topic 718
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 2
-Subparagraph (a)(1)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480429/718-10-50-2
| Name: |
us-gaap_SharebasedCompensationArrangementBySharebasedPaymentAwardAwardVestingRightsPercentage |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
dtr-types:percentItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionPeriod from grant date that an equity-based award expires, in 'PnYnMnDTnHnMnS' format, for example, 'P1Y5M13D' represents the reported fact of one year, five months, and thirteen days. Reference 1: http://www.xbrl.org/2003/role/exampleRef
-Topic 718
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 2
-Subparagraph (a)(2)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480429/718-10-50-2
| Name: |
us-gaap_SharebasedCompensationArrangementBySharebasedPaymentAwardExpirationPeriod |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:durationItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- Details
| Name: |
us-gaap_AwardTypeAxis=us-gaap_EmployeeStockOptionMember |
| Namespace Prefix: |
|
| Data Type: |
na |
| Balance Type: |
|
| Period Type: |
|
|
| X |
- Details
| Name: |
us-gaap_AwardTypeAxis=us-gaap_RestrictedStockMember |
| Namespace Prefix: |
|
| Data Type: |
na |
| Balance Type: |
|
| Period Type: |
|
|
| X |
- Details
| Name: |
us-gaap_AwardTypeAxis=alhc_PreIpoAwardsConvertedRestrictedStockAwardsMember |
| Namespace Prefix: |
|
| Data Type: |
na |
| Balance Type: |
|
| Period Type: |
|
|
| X |
- Details
| Name: |
us-gaap_AwardTypeAxis=us-gaap_RestrictedStockUnitsRSUMember |
| Namespace Prefix: |
|
| Data Type: |
na |
| Balance Type: |
|
| Period Type: |
|
|
| X |
- Details
| Name: |
srt_StatementScenarioAxis=srt_ScenarioForecastMember |
| Namespace Prefix: |
|
| Data Type: |
na |
| Balance Type: |
|
| Period Type: |
|
|
| X |
- Details
| Name: |
srt_RangeAxis=srt_MinimumMember |
| Namespace Prefix: |
|
| Data Type: |
na |
| Balance Type: |
|
| Period Type: |
|
|
| X |
- Details
| Name: |
srt_RangeAxis=srt_MaximumMember |
| Namespace Prefix: |
|
| Data Type: |
na |
| Balance Type: |
|
| Period Type: |
|
|
| X |
- Details
| Name: |
us-gaap_AwardTypeAxis=alhc_NonVestedAwardsRsaOptionsAndRsuMember |
| Namespace Prefix: |
|
| Data Type: |
na |
| Balance Type: |
|
| Period Type: |
|
|
v3.24.2.u1
Equity-Based Compensation - Schedule of Stock Option Activity Transactions (Details) - USD ($)
$ / shares in Units, $ in Thousands |
3 Months Ended |
6 Months Ended |
12 Months Ended |
Jun. 30, 2024 |
Mar. 31, 2024 |
Jun. 30, 2024 |
Dec. 31, 2023 |
| Shares Subject to Options Outstanding |
|
|
|
|
| Options outstanding, beginning balance (in shares) |
9,023,343
|
9,135,879
|
9,135,879
|
|
| Options granted (in shares) |
0
|
0
|
|
|
| Options exercised (in shares) |
0
|
0
|
|
|
| Options forfeited / expired (in shares) |
(73,754)
|
(112,536)
|
|
|
| Options outstanding, ending balance (in shares) |
8,949,589
|
9,023,343
|
8,949,589
|
9,135,879
|
| Options outstanding, vested and exercisable (in shares) |
6,297,452
|
|
6,297,452
|
|
| Weighted- Average Exercise Price per Option |
|
|
|
|
| Options outstanding, beginning balance (in dollars per share) |
$ 16.97
|
$ 16.95
|
$ 16.95
|
|
| Options granted (n dollars per share) |
0
|
0
|
|
|
| Options exercised (in dollars per share) |
0
|
0
|
|
|
| Options forfeited / expired (in dollars per share) |
16.62
|
15.41
|
|
|
| Options outstanding, ending balance (in dollars per share) |
16.97
|
$ 16.97
|
16.97
|
$ 16.95
|
| Options outstanding, vested and exercisable (in dollars per share) |
$ 17.28
|
|
$ 17.28
|
|
| Stock Option Activity, Additional Disclosures |
|
|
|
|
| Weighted-average remaining contractual terms, outstanding |
|
7 years 14 days
|
6 years 9 months 14 days
|
7 years 3 months 14 days
|
| Weighted-average remaining contractual terms, vested and exercisable |
|
|
6 years 9 months
|
|
| Aggregate intrinsic value |
$ 27
|
$ 0
|
$ 27
|
$ 79
|
| Aggregate intrinsic value, vested and exercisable |
$ 14
|
|
$ 14
|
|
| X |
- References
+ Details
| Name: |
us-gaap_ShareBasedCompensationArrangementByShareBasedPaymentAwardOptionsAdditionalDisclosuresAbstract |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:stringItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionFor presentations that combine terminations, the number of shares under options that were cancelled during the reporting period as a result of occurrence of a terminating event specified in contractual agreements pertaining to the stock option plan or that expired. Reference 1: http://www.xbrl.org/2009/role/commonPracticeRef
-Topic 718
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 2
-Subparagraph (c)(1)(iv)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480429/718-10-50-2
| Name: |
us-gaap_ShareBasedCompensationArrangementByShareBasedPaymentAwardOptionsForfeituresAndExpirationsInPeriod |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:sharesItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionWeighted average price of options that were either forfeited or expired. Reference 1: http://www.xbrl.org/2009/role/commonPracticeRef
-Topic 718
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 2
-Subparagraph (c)(1)(iv)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480429/718-10-50-2
| Name: |
us-gaap_ShareBasedCompensationArrangementByShareBasedPaymentAwardOptionsForfeituresAndExpirationsInPeriodWeightedAverageExercisePrice |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
dtr-types:perShareItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionGross number of share options (or share units) granted during the period. Reference 1: http://www.xbrl.org/2003/role/disclosureRef
-Topic 718
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 2
-Subparagraph (c)(1)(iv)(01)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480429/718-10-50-2
| Name: |
us-gaap_ShareBasedCompensationArrangementByShareBasedPaymentAwardOptionsGrantsInPeriodGross |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:sharesItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionAmount by which the current fair value of the underlying stock exceeds the exercise price of options outstanding. Reference 1: http://fasb.org/us-gaap/role/ref/legacyRef
-Name Accounting Standards Codification
-Topic 718
-SubTopic 10
-Section 50
-Paragraph 2
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480429/718-10-50-2
| Name: |
us-gaap_ShareBasedCompensationArrangementByShareBasedPaymentAwardOptionsOutstandingIntrinsicValue |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:monetaryItemType |
| Balance Type: |
debit |
| Period Type: |
instant |
|
| X |
- DefinitionNumber of options outstanding, including both vested and non-vested options. Reference 1: http://www.xbrl.org/2003/role/disclosureRef
-Topic 718
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 2
-Subparagraph (c)(1)(i)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480429/718-10-50-2
Reference 2: http://www.xbrl.org/2003/role/disclosureRef
-Topic 718
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 2
-Subparagraph (c)(1)(ii)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480429/718-10-50-2
| Name: |
us-gaap_ShareBasedCompensationArrangementByShareBasedPaymentAwardOptionsOutstandingNumber |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:sharesItemType |
| Balance Type: |
na |
| Period Type: |
instant |
|
| X |
- DefinitionA roll forward is a reconciliation of a concept from the beginning of a period to the end of a period.
| Name: |
us-gaap_ShareBasedCompensationArrangementByShareBasedPaymentAwardOptionsOutstandingRollForward |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:stringItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionWeighted average price at which grantees can acquire the shares reserved for issuance under the stock option plan. Reference 1: http://www.xbrl.org/2003/role/disclosureRef
-Topic 718
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 2
-Subparagraph (c)(1)(i)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480429/718-10-50-2
Reference 2: http://www.xbrl.org/2003/role/disclosureRef
-Topic 718
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 2
-Subparagraph (c)(1)(ii)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480429/718-10-50-2
| Name: |
us-gaap_ShareBasedCompensationArrangementByShareBasedPaymentAwardOptionsOutstandingWeightedAverageExercisePrice |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
dtr-types:perShareItemType |
| Balance Type: |
na |
| Period Type: |
instant |
|
| X |
- References
+ Details
| Name: |
us-gaap_ShareBasedCompensationArrangementByShareBasedPaymentAwardOptionsOutstandingWeightedAverageExercisePriceRollforward |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:stringItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionAmount by which current fair value of underlying stock exceeds exercise price of fully vested and expected to vest options outstanding. Includes, but is not limited to, unvested options for which requisite service period has not been rendered but that are expected to vest based on achievement of performance condition, if forfeitures are recognized when they occur. Reference 1: http://www.xbrl.org/2003/role/disclosureRef
-Topic 718
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 2
-Subparagraph (e)(1)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480429/718-10-50-2
| Name: |
us-gaap_ShareBasedCompensationArrangementByShareBasedPaymentAwardOptionsVestedAndExpectedToVestOutstandingAggregateIntrinsicValue |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:monetaryItemType |
| Balance Type: |
debit |
| Period Type: |
instant |
|
| X |
- DefinitionNumber of fully vested and expected to vest options outstanding that can be converted into shares under option plan. Includes, but is not limited to, unvested options for which requisite service period has not been rendered but that are expected to vest based on achievement of performance condition, if forfeitures are recognized when they occur. Reference 1: http://www.xbrl.org/2003/role/disclosureRef
-Topic 718
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 2
-Subparagraph (e)(1)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480429/718-10-50-2
| Name: |
us-gaap_ShareBasedCompensationArrangementByShareBasedPaymentAwardOptionsVestedAndExpectedToVestOutstandingNumber |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:sharesItemType |
| Balance Type: |
na |
| Period Type: |
instant |
|
| X |
- DefinitionWeighted-average exercise price, at which grantee can acquire shares reserved for issuance, for fully vested and expected to vest options outstanding. Includes, but is not limited to, unvested options for which requisite service period has not been rendered but that are expected to vest based on achievement of performance condition, if forfeitures are recognized when they occur. Reference 1: http://www.xbrl.org/2003/role/disclosureRef
-Topic 718
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 2
-Subparagraph (e)(1)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480429/718-10-50-2
| Name: |
us-gaap_ShareBasedCompensationArrangementByShareBasedPaymentAwardOptionsVestedAndExpectedToVestOutstandingWeightedAverageExercisePrice |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
dtr-types:perShareItemType |
| Balance Type: |
na |
| Period Type: |
instant |
|
| X |
- DefinitionWeighted average price at which option holders acquired shares when converting their stock options into shares. Reference 1: http://www.xbrl.org/2003/role/disclosureRef
-Topic 718
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 2
-Subparagraph (c)(1)(iv)(02)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480429/718-10-50-2
| Name: |
us-gaap_ShareBasedCompensationArrangementsByShareBasedPaymentAwardOptionsExercisesInPeriodWeightedAverageExercisePrice |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
dtr-types:perShareItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionWeighted average per share amount at which grantees can acquire shares of common stock by exercise of options. Reference 1: http://www.xbrl.org/2003/role/disclosureRef
-Topic 718
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 2
-Subparagraph (c)(1)(iv)(01)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480429/718-10-50-2
| Name: |
us-gaap_ShareBasedCompensationArrangementsByShareBasedPaymentAwardOptionsGrantsInPeriodWeightedAverageExercisePrice |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
dtr-types:perShareItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionWeighted average remaining contractual term for option awards outstanding, in 'PnYnMnDTnHnMnS' format, for example, 'P1Y5M13D' represents the reported fact of one year, five months, and thirteen days. Reference 1: http://fasb.org/us-gaap/role/ref/legacyRef
-Topic 718
-SubTopic 10
-Subparagraph (e)(1)
-Name Accounting Standards Codification
-Paragraph 2
-Section 50
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480429/718-10-50-2
| Name: |
us-gaap_SharebasedCompensationArrangementBySharebasedPaymentAwardOptionsOutstandingWeightedAverageRemainingContractualTerm2 |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:durationItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionWeighted average remaining contractual term for fully vested and expected to vest options outstanding, in 'PnYnMnDTnHnMnS' format, for example, 'P1Y5M13D' represents reported fact of one year, five months, and thirteen days. Includes, but is not limited to, unvested options for which requisite service period has not been rendered but that are expected to vest based on achievement of performance condition, if forfeitures are recognized when they occur. Reference 1: http://www.xbrl.org/2003/role/disclosureRef
-Topic 718
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 2
-Subparagraph (e)(1)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480429/718-10-50-2
| Name: |
us-gaap_SharebasedCompensationArrangementBySharebasedPaymentAwardOptionsVestedAndExpectedToVestOutstandingWeightedAverageRemainingContractualTerm1 |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:durationItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionNumber of share options (or share units) exercised during the current period. Reference 1: http://fasb.org/us-gaap/role/ref/legacyRef
-Name Accounting Standards Codification
-Section 50
-Paragraph 2
-SubTopic 10
-Topic 505
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147481112/505-10-50-2
Reference 2: http://fasb.org/us-gaap/role/ref/legacyRef
-Topic 210
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.5-02(28))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480566/210-10-S99-1
Reference 3: http://fasb.org/us-gaap/role/ref/legacyRef
-Topic 210
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.5-02(29))
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480566/210-10-S99-1
Reference 4: http://www.xbrl.org/2003/role/disclosureRef
-Topic 718
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 2
-Subparagraph (c)(1)(iv)(02)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480429/718-10-50-2
Reference 5: http://fasb.org/us-gaap/role/ref/legacyRef
-Topic 505
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SX 210.3-04)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480008/505-10-S99-1
| Name: |
us-gaap_StockIssuedDuringPeriodSharesStockOptionsExercised |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:sharesItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
v3.24.2.u1
Equity-Based Compensation - Schedule of RSAs Transactions (Details) - Restricted Stock Awards - $ / shares
|
3 Months Ended |
Jun. 30, 2024 |
Mar. 31, 2024 |
Mar. 31, 2023 |
| Share-Based Compensation Arrangement by Share-Based Payment Award, Equity Instruments Other than Options, Nonvested, Number of Shares [Roll Forward] |
|
|
|
| Unvested and outstanding, beginning balance (in shares) |
540,298
|
683,953
|
|
| Vested (in shares) |
(3,056)
|
|
(140,856)
|
| Forfeited (in shares) |
0
|
|
(2,799)
|
| Unvested and outstanding, ending balance (in shares) |
537,242
|
540,298
|
|
| Weighted-Average Grant Date Fair Value |
|
|
|
| Unvested and outstanding, beginning balance (in dollars per share) |
$ 3.94
|
$ 5.86
|
|
| Vested (in dollars per share) |
2.49
|
|
$ 13.22
|
| Forfeited (in dollars per share) |
0
|
|
$ 5.05
|
| Unvested and outstanding, ending balance (in dollars per share) |
$ 3.95
|
$ 3.94
|
|
| X |
- DefinitionThe number of equity-based payment instruments, excluding stock (or unit) options, that were forfeited during the reporting period. Reference 1: http://www.xbrl.org/2003/role/disclosureRef
-Topic 718
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 2
-Subparagraph (c)(2)(iii)(03)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480429/718-10-50-2
| Name: |
us-gaap_ShareBasedCompensationArrangementByShareBasedPaymentAwardEquityInstrumentsOtherThanOptionsForfeitedInPeriod |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:sharesItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionWeighted average fair value as of the grant date of equity-based award plans other than stock (unit) option plans that were not exercised or put into effect as a result of the occurrence of a terminating event. Reference 1: http://www.xbrl.org/2003/role/disclosureRef
-Topic 718
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 2
-Subparagraph (c)(2)(iii)(03)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480429/718-10-50-2
| Name: |
us-gaap_ShareBasedCompensationArrangementByShareBasedPaymentAwardEquityInstrumentsOtherThanOptionsForfeituresWeightedAverageGrantDateFairValue |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
dtr-types:perShareItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionThe number of non-vested equity-based payment instruments, excluding stock (or unit) options, that validly exist and are outstanding as of the balance sheet date. Reference 1: http://www.xbrl.org/2003/role/disclosureRef
-Topic 718
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 2
-Subparagraph (c)(2)(i)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480429/718-10-50-2
Reference 2: http://www.xbrl.org/2003/role/disclosureRef
-Topic 718
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 2
-Subparagraph (c)(2)(ii)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480429/718-10-50-2
| Name: |
us-gaap_ShareBasedCompensationArrangementByShareBasedPaymentAwardEquityInstrumentsOtherThanOptionsNonvestedNumber |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:sharesItemType |
| Balance Type: |
na |
| Period Type: |
instant |
|
| X |
- DefinitionA roll forward is a reconciliation of a concept from the beginning of a period to the end of a period.
| Name: |
us-gaap_ShareBasedCompensationArrangementByShareBasedPaymentAwardEquityInstrumentsOtherThanOptionsNonvestedRollForward |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:stringItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionPer share or unit weighted-average fair value of nonvested award under share-based payment arrangement. Excludes share and unit options. Reference 1: http://www.xbrl.org/2003/role/disclosureRef
-Topic 718
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 2
-Subparagraph (c)(2)(i)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480429/718-10-50-2
Reference 2: http://www.xbrl.org/2003/role/disclosureRef
-Topic 718
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 2
-Subparagraph (c)(2)(ii)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480429/718-10-50-2
| Name: |
us-gaap_ShareBasedCompensationArrangementByShareBasedPaymentAwardEquityInstrumentsOtherThanOptionsNonvestedWeightedAverageGrantDateFairValue |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
dtr-types:perShareItemType |
| Balance Type: |
na |
| Period Type: |
instant |
|
| X |
- References
+ Details
| Name: |
us-gaap_ShareBasedCompensationArrangementByShareBasedPaymentAwardEquityInstrumentsOtherThanOptionsNonvestedWeightedAverageGrantDateFairValueRollForward |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:stringItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionThe number of equity-based payment instruments, excluding stock (or unit) options, that vested during the reporting period. Reference 1: http://www.xbrl.org/2003/role/disclosureRef
-Topic 718
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 2
-Subparagraph (c)(2)(iii)(02)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480429/718-10-50-2
| Name: |
us-gaap_ShareBasedCompensationArrangementByShareBasedPaymentAwardEquityInstrumentsOtherThanOptionsVestedInPeriod |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:sharesItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionThe weighted average fair value as of grant date pertaining to an equity-based award plan other than a stock (or unit) option plan for which the grantee gained the right during the reporting period, by satisfying service and performance requirements, to receive or retain shares or units, other instruments, or cash in accordance with the terms of the arrangement. Reference 1: http://www.xbrl.org/2003/role/disclosureRef
-Topic 718
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 2
-Subparagraph (c)(2)(iii)(02)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480429/718-10-50-2
| Name: |
us-gaap_ShareBasedCompensationArrangementByShareBasedPaymentAwardEquityInstrumentsOtherThanOptionsVestedInPeriodWeightedAverageGrantDateFairValue |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
dtr-types:perShareItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- Details
| Name: |
us-gaap_AwardTypeAxis=us-gaap_RestrictedStockMember |
| Namespace Prefix: |
|
| Data Type: |
na |
| Balance Type: |
|
| Period Type: |
|
|
v3.24.2.u1
Equity-Based Compensation - Schedule of RSU Transactions (Details) - RSUs - $ / shares
|
3 Months Ended |
Jun. 30, 2024 |
Mar. 31, 2024 |
| Share-Based Compensation Arrangement by Share-Based Payment Award, Equity Instruments Other than Options, Nonvested, Number of Shares [Roll Forward] |
|
|
| Unvested and outstanding, beginning balance (in shares) |
14,390,497
|
10,541,625
|
| Granted (in shares) |
103,292
|
6,517,337
|
| Vested (in shares) |
(80,178)
|
(2,385,493)
|
| Cancelled/forfeited (in shares) |
(395,338)
|
(282,972)
|
| Unvested and outstanding, ending balance (in shares) |
14,018,273
|
14,390,497
|
| Weighted-Average Grant Date Fair Value |
|
|
| Unvested and outstanding, beginning balance (in dollars per share) |
$ 8.97
|
$ 11.25
|
| Granted (in dollars per share) |
5.62
|
5.05
|
| Vested (in dollars per share) |
6.07
|
8.25
|
| Cancelled/forfeited (in dollars per share) |
8.40
|
9.36
|
| Unvested and outstanding, ending balance (in dollars per share) |
$ 8.98
|
$ 8.97
|
| Number of shares vested but issuance and delivery deferred (in shares) |
|
107,948
|
| X |
- DefinitionShare-Based Compensation Arrangement by Share-Based Payment Award, Equity Instruments Other than Options, Vested in Period, Issuance Deferred
| Name: |
alhc_ShareBasedCompensationArrangementByShareBasedPaymentAwardEquityInstrumentsOtherThanOptionsVestedInPeriodIssuanceDeferred |
| Namespace Prefix: |
alhc_ |
| Data Type: |
xbrli:sharesItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionThe number of equity-based payment instruments, excluding stock (or unit) options, that were forfeited during the reporting period. Reference 1: http://www.xbrl.org/2003/role/disclosureRef
-Topic 718
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 2
-Subparagraph (c)(2)(iii)(03)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480429/718-10-50-2
| Name: |
us-gaap_ShareBasedCompensationArrangementByShareBasedPaymentAwardEquityInstrumentsOtherThanOptionsForfeitedInPeriod |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:sharesItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionWeighted average fair value as of the grant date of equity-based award plans other than stock (unit) option plans that were not exercised or put into effect as a result of the occurrence of a terminating event. Reference 1: http://www.xbrl.org/2003/role/disclosureRef
-Topic 718
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 2
-Subparagraph (c)(2)(iii)(03)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480429/718-10-50-2
| Name: |
us-gaap_ShareBasedCompensationArrangementByShareBasedPaymentAwardEquityInstrumentsOtherThanOptionsForfeituresWeightedAverageGrantDateFairValue |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
dtr-types:perShareItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionThe number of grants made during the period on other than stock (or unit) option plans (for example, phantom stock or unit plan, stock or unit appreciation rights plan, performance target plan). Reference 1: http://www.xbrl.org/2003/role/disclosureRef
-Topic 718
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 2
-Subparagraph (c)(2)(iii)(01)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480429/718-10-50-2
| Name: |
us-gaap_ShareBasedCompensationArrangementByShareBasedPaymentAwardEquityInstrumentsOtherThanOptionsGrantsInPeriod |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:sharesItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionThe weighted average fair value at grant date for nonvested equity-based awards issued during the period on other than stock (or unit) option plans (for example, phantom stock or unit plan, stock or unit appreciation rights plan, performance target plan). Reference 1: http://www.xbrl.org/2003/role/disclosureRef
-Topic 718
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 2
-Subparagraph (c)(2)(iii)(01)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480429/718-10-50-2
| Name: |
us-gaap_ShareBasedCompensationArrangementByShareBasedPaymentAwardEquityInstrumentsOtherThanOptionsGrantsInPeriodWeightedAverageGrantDateFairValue |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
dtr-types:perShareItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionThe number of non-vested equity-based payment instruments, excluding stock (or unit) options, that validly exist and are outstanding as of the balance sheet date. Reference 1: http://www.xbrl.org/2003/role/disclosureRef
-Topic 718
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 2
-Subparagraph (c)(2)(i)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480429/718-10-50-2
Reference 2: http://www.xbrl.org/2003/role/disclosureRef
-Topic 718
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 2
-Subparagraph (c)(2)(ii)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480429/718-10-50-2
| Name: |
us-gaap_ShareBasedCompensationArrangementByShareBasedPaymentAwardEquityInstrumentsOtherThanOptionsNonvestedNumber |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:sharesItemType |
| Balance Type: |
na |
| Period Type: |
instant |
|
| X |
- DefinitionA roll forward is a reconciliation of a concept from the beginning of a period to the end of a period.
| Name: |
us-gaap_ShareBasedCompensationArrangementByShareBasedPaymentAwardEquityInstrumentsOtherThanOptionsNonvestedRollForward |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:stringItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionPer share or unit weighted-average fair value of nonvested award under share-based payment arrangement. Excludes share and unit options. Reference 1: http://www.xbrl.org/2003/role/disclosureRef
-Topic 718
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 2
-Subparagraph (c)(2)(i)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480429/718-10-50-2
Reference 2: http://www.xbrl.org/2003/role/disclosureRef
-Topic 718
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 2
-Subparagraph (c)(2)(ii)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480429/718-10-50-2
| Name: |
us-gaap_ShareBasedCompensationArrangementByShareBasedPaymentAwardEquityInstrumentsOtherThanOptionsNonvestedWeightedAverageGrantDateFairValue |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
dtr-types:perShareItemType |
| Balance Type: |
na |
| Period Type: |
instant |
|
| X |
- References
+ Details
| Name: |
us-gaap_ShareBasedCompensationArrangementByShareBasedPaymentAwardEquityInstrumentsOtherThanOptionsNonvestedWeightedAverageGrantDateFairValueRollForward |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:stringItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionThe number of equity-based payment instruments, excluding stock (or unit) options, that vested during the reporting period. Reference 1: http://www.xbrl.org/2003/role/disclosureRef
-Topic 718
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 2
-Subparagraph (c)(2)(iii)(02)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480429/718-10-50-2
| Name: |
us-gaap_ShareBasedCompensationArrangementByShareBasedPaymentAwardEquityInstrumentsOtherThanOptionsVestedInPeriod |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:sharesItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionThe weighted average fair value as of grant date pertaining to an equity-based award plan other than a stock (or unit) option plan for which the grantee gained the right during the reporting period, by satisfying service and performance requirements, to receive or retain shares or units, other instruments, or cash in accordance with the terms of the arrangement. Reference 1: http://www.xbrl.org/2003/role/disclosureRef
-Topic 718
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 2
-Subparagraph (c)(2)(iii)(02)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480429/718-10-50-2
| Name: |
us-gaap_ShareBasedCompensationArrangementByShareBasedPaymentAwardEquityInstrumentsOtherThanOptionsVestedInPeriodWeightedAverageGrantDateFairValue |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
dtr-types:perShareItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- Details
| Name: |
us-gaap_AwardTypeAxis=us-gaap_RestrictedStockUnitsRSUMember |
| Namespace Prefix: |
|
| Data Type: |
na |
| Balance Type: |
|
| Period Type: |
|
|
v3.24.2.u1
Equity-Based Compensation - Schedule of PSUs Transactions (Details) - Performance-based Restricted Stock Units - $ / shares
|
3 Months Ended |
Jun. 30, 2024 |
Mar. 31, 2024 |
| Share-Based Compensation Arrangement by Share-Based Payment Award, Equity Instruments Other than Options, Nonvested, Number of Shares [Roll Forward] |
|
|
| Unvested and outstanding, beginning balance (in shares) |
8,376,538
|
7,233,205
|
| Granted (in shares) |
0
|
1,160,000
|
| Vested (in shares) |
0
|
0
|
| Cancelled/forfeited (in shares) |
(198,333)
|
(16,667)
|
| Unvested and outstanding, ending balance (in shares) |
8,178,205
|
8,376,538
|
| Weighted-Average Grant Date Fair Value |
|
|
| Unvested and outstanding, beginning balance (in dollars per share) |
$ 5.64
|
$ 5.74
|
| Granted (in dollars per share) |
0
|
5.00
|
| Vested (in dollars per share) |
0
|
0
|
| Cancelled/forfeited (in dollars per share) |
5.67
|
5.74
|
| Unvested and outstanding, ending balance (in dollars per share) |
$ 5.64
|
$ 5.64
|
| X |
- DefinitionThe number of equity-based payment instruments, excluding stock (or unit) options, that were forfeited during the reporting period. Reference 1: http://www.xbrl.org/2003/role/disclosureRef
-Topic 718
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 2
-Subparagraph (c)(2)(iii)(03)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480429/718-10-50-2
| Name: |
us-gaap_ShareBasedCompensationArrangementByShareBasedPaymentAwardEquityInstrumentsOtherThanOptionsForfeitedInPeriod |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:sharesItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionWeighted average fair value as of the grant date of equity-based award plans other than stock (unit) option plans that were not exercised or put into effect as a result of the occurrence of a terminating event. Reference 1: http://www.xbrl.org/2003/role/disclosureRef
-Topic 718
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 2
-Subparagraph (c)(2)(iii)(03)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480429/718-10-50-2
| Name: |
us-gaap_ShareBasedCompensationArrangementByShareBasedPaymentAwardEquityInstrumentsOtherThanOptionsForfeituresWeightedAverageGrantDateFairValue |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
dtr-types:perShareItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionThe number of grants made during the period on other than stock (or unit) option plans (for example, phantom stock or unit plan, stock or unit appreciation rights plan, performance target plan). Reference 1: http://www.xbrl.org/2003/role/disclosureRef
-Topic 718
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 2
-Subparagraph (c)(2)(iii)(01)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480429/718-10-50-2
| Name: |
us-gaap_ShareBasedCompensationArrangementByShareBasedPaymentAwardEquityInstrumentsOtherThanOptionsGrantsInPeriod |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:sharesItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionThe weighted average fair value at grant date for nonvested equity-based awards issued during the period on other than stock (or unit) option plans (for example, phantom stock or unit plan, stock or unit appreciation rights plan, performance target plan). Reference 1: http://www.xbrl.org/2003/role/disclosureRef
-Topic 718
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 2
-Subparagraph (c)(2)(iii)(01)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480429/718-10-50-2
| Name: |
us-gaap_ShareBasedCompensationArrangementByShareBasedPaymentAwardEquityInstrumentsOtherThanOptionsGrantsInPeriodWeightedAverageGrantDateFairValue |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
dtr-types:perShareItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionThe number of non-vested equity-based payment instruments, excluding stock (or unit) options, that validly exist and are outstanding as of the balance sheet date. Reference 1: http://www.xbrl.org/2003/role/disclosureRef
-Topic 718
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 2
-Subparagraph (c)(2)(i)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480429/718-10-50-2
Reference 2: http://www.xbrl.org/2003/role/disclosureRef
-Topic 718
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 2
-Subparagraph (c)(2)(ii)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480429/718-10-50-2
| Name: |
us-gaap_ShareBasedCompensationArrangementByShareBasedPaymentAwardEquityInstrumentsOtherThanOptionsNonvestedNumber |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:sharesItemType |
| Balance Type: |
na |
| Period Type: |
instant |
|
| X |
- DefinitionA roll forward is a reconciliation of a concept from the beginning of a period to the end of a period.
| Name: |
us-gaap_ShareBasedCompensationArrangementByShareBasedPaymentAwardEquityInstrumentsOtherThanOptionsNonvestedRollForward |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:stringItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionPer share or unit weighted-average fair value of nonvested award under share-based payment arrangement. Excludes share and unit options. Reference 1: http://www.xbrl.org/2003/role/disclosureRef
-Topic 718
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 2
-Subparagraph (c)(2)(i)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480429/718-10-50-2
Reference 2: http://www.xbrl.org/2003/role/disclosureRef
-Topic 718
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 2
-Subparagraph (c)(2)(ii)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480429/718-10-50-2
| Name: |
us-gaap_ShareBasedCompensationArrangementByShareBasedPaymentAwardEquityInstrumentsOtherThanOptionsNonvestedWeightedAverageGrantDateFairValue |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
dtr-types:perShareItemType |
| Balance Type: |
na |
| Period Type: |
instant |
|
| X |
- References
+ Details
| Name: |
us-gaap_ShareBasedCompensationArrangementByShareBasedPaymentAwardEquityInstrumentsOtherThanOptionsNonvestedWeightedAverageGrantDateFairValueRollForward |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:stringItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionThe number of equity-based payment instruments, excluding stock (or unit) options, that vested during the reporting period. Reference 1: http://www.xbrl.org/2003/role/disclosureRef
-Topic 718
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 2
-Subparagraph (c)(2)(iii)(02)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480429/718-10-50-2
| Name: |
us-gaap_ShareBasedCompensationArrangementByShareBasedPaymentAwardEquityInstrumentsOtherThanOptionsVestedInPeriod |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:sharesItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionThe weighted average fair value as of grant date pertaining to an equity-based award plan other than a stock (or unit) option plan for which the grantee gained the right during the reporting period, by satisfying service and performance requirements, to receive or retain shares or units, other instruments, or cash in accordance with the terms of the arrangement. Reference 1: http://www.xbrl.org/2003/role/disclosureRef
-Topic 718
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 2
-Subparagraph (c)(2)(iii)(02)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480429/718-10-50-2
| Name: |
us-gaap_ShareBasedCompensationArrangementByShareBasedPaymentAwardEquityInstrumentsOtherThanOptionsVestedInPeriodWeightedAverageGrantDateFairValue |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
dtr-types:perShareItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
v3.24.2.u1
Equity-Based Compensation - Schedule of Equity-based Compensation Expense on Statement of Operations (Details) - USD ($)
$ in Thousands |
3 Months Ended |
6 Months Ended |
Jun. 30, 2024 |
Jun. 30, 2023 |
Jun. 30, 2024 |
Jun. 30, 2023 |
| Share-Based Payment Arrangement, Expensed and Capitalized, Amount [Line Items] |
|
|
|
|
| Total equity-based compensation expense |
$ 16,784
|
$ 15,636
|
$ 37,638
|
$ 37,614
|
| Selling, general and administrative expenses |
|
|
|
|
| Share-Based Payment Arrangement, Expensed and Capitalized, Amount [Line Items] |
|
|
|
|
| Total equity-based compensation expense |
16,022
|
13,869
|
35,743
|
33,323
|
| Medical expenses |
|
|
|
|
| Share-Based Payment Arrangement, Expensed and Capitalized, Amount [Line Items] |
|
|
|
|
| Total equity-based compensation expense |
$ 762
|
$ 1,767
|
$ 1,895
|
$ 4,291
|
| X |
- DefinitionAmount of expense for award under share-based payment arrangement. Excludes amount capitalized. Reference 1: http://www.xbrl.org/2003/role/disclosureRef
-Topic 718
-SubTopic 10
-Name Accounting Standards Codification
-Section S99
-Paragraph 1
-Subparagraph (SAB Topic 14.F)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147479830/718-10-S99-1
Reference 2: http://www.xbrl.org/2003/role/disclosureRef
-Topic 718
-SubTopic 10
-Name Accounting Standards Codification
-Section 50
-Paragraph 2
-Subparagraph (h)(1)(i)
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147480429/718-10-50-2
| Name: |
us-gaap_AllocatedShareBasedCompensationExpense |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:monetaryItemType |
| Balance Type: |
debit |
| Period Type: |
duration |
|
| X |
- DefinitionLine items represent financial concepts included in a table. These concepts are used to disclose reportable information associated with domain members defined in one or many axes to the table.
| Name: |
us-gaap_EmployeeServiceShareBasedCompensationAllocationOfRecognizedPeriodCostsLineItems |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:stringItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- Details
| Name: |
us-gaap_IncomeStatementLocationAxis=us-gaap_SellingGeneralAndAdministrativeExpensesMember |
| Namespace Prefix: |
|
| Data Type: |
na |
| Balance Type: |
|
| Period Type: |
|
|
| X |
- Details
| Name: |
us-gaap_IncomeStatementLocationAxis=alhc_MedicalExpensesMember |
| Namespace Prefix: |
|
| Data Type: |
na |
| Balance Type: |
|
| Period Type: |
|
|
v3.24.2.u1
| X |
- References
+ Details
| Name: |
us-gaap_CommitmentsAndContingenciesDisclosureAbstract |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:stringItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionAmount awarded to other party in judgment or settlement of litigation.
| Name: |
us-gaap_LitigationSettlementAmountAwardedToOtherParty |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:monetaryItemType |
| Balance Type: |
credit |
| Period Type: |
duration |
|
| X |
- DefinitionAmount of loss contingency liability expected to be resolved within one year or the normal operating cycle, if longer. Reference 1: http://www.xbrl.org/2003/role/disclosureRef
-Topic 450
-SubTopic 20
-Name Accounting Standards Codification
-Section 50
-Paragraph 1
-Publisher FASB
-URI https://asc.fasb.org/1943274/2147483076/450-20-50-1
| Name: |
us-gaap_LossContingencyAccrualCarryingValueCurrent |
| Namespace Prefix: |
us-gaap_ |
| Data Type: |
xbrli:monetaryItemType |
| Balance Type: |
credit |
| Period Type: |
instant |
|
Alignment Healthcare (NASDAQ:ALHC)
過去 株価チャート
から 7 2024 まで 8 2024
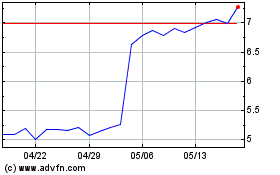
Alignment Healthcare (NASDAQ:ALHC)
過去 株価チャート
から 8 2023 まで 8 2024