New Clinical Data Demonstrates Three Years of Continuous Treatment
with Dual-Acting LEQEMBI® (lecanemab-irmb) Continues to
Significantly Benefit Early Alzheimer’s Disease Patients Presented
at The Alzheimer’s Association International Conference (AAIC) 2024
51% of No Tau / Low Tau Patients Showed
Improved Cognition and Function Over Three Years; Only Lecanemab
Has Clinical Data in No Tau / Low Tau Patient
Group
Clinical Data and Biomarkers Show
Alzheimer’s Disease Does Not Stop Progressing After Plaque
Clearance. Lecanemab’s Dual Action Supports Neuronal Function by
Clearing Highly Toxic Protofibrils that Continue to Cause Neuronal
Injury and Death After Rapid Plaque Clearance
Lecanemab Slows Tau Spread Across All
Brain Regions
PHILADELPHIA, July 30, 2024 (GLOBE NEWSWIRE) --
Eisai Co., Ltd. (Headquarters: Tokyo, CEO: Haruo Naito, “Eisai”)
and Biogen Inc. (Nasdaq: BIIB, Headquarters: Cambridge,
Massachusetts, United States, CEO: Christopher A. Viehbacher,
“Biogen”) announced today that the latest findings for
lecanemab-irmb (U.S. brand name: LEQEMBI®), an
anti-amyloid beta (Aβ) protofibril* antibody for the treatment of
early Alzheimer’s disease (AD), were presented at the Alzheimer’s
Association International Conference (AAIC) 2024, held in
Philadelphia, USA, and virtually. Dual-acting lecanemab is the only
early AD treatment widely available to support neuronal function by
clearing the highly toxic protofibrils that continue to cause
neuronal injury and death even after plaques have been cleared from
the brain. The presentation slides for the two scientific sessions
on lecanemab at the AAIC will be available on the Eisai Co. Ltd.
Investor Page by 7:00 p.m. on July 30th EDT.
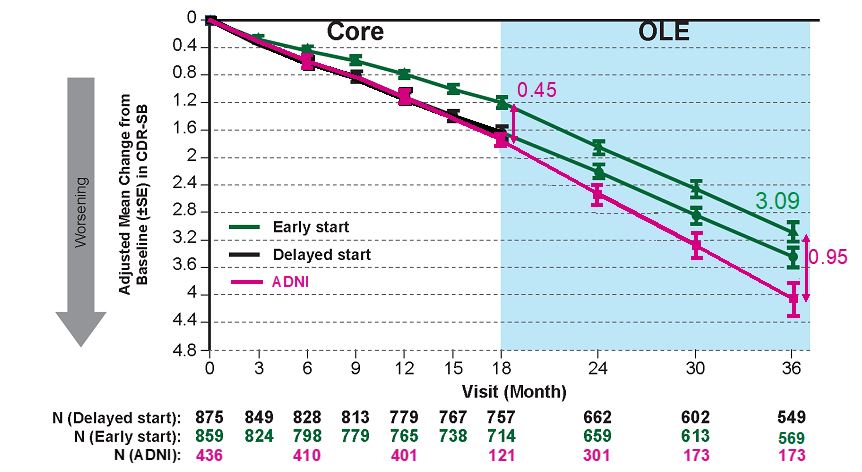
Three Years of Continuous Lecanemab
Treatment Reduced Clinical Decline by -0.95 on CDR-SB Showing
Continued Clinically and Personally Meaningful Benefit for Early AD
Patients
Clarity AD was a global Phase 3 placebo-controlled, double-blind,
parallel-group, randomized study in 1,795 people with early AD
(Lecanemab group: 10 mg/kg bi-weekly IV treatment: 898, placebo
group: 897). 95% of patients who completed the core study (18
months) chose to continue in the open-label extension study (OLE).
In the Clarity AD core study, the mean change from baseline between
the lecanemab treated group and the placebo group was -0.45
(P=0.00005) on the primary endpoint of the Clinical Dementia
Rating-Sum of Boxes (CDR-SB) global cognitive and functional scale.
Over three years of treatment across the core study and OLE,
lecanemab reduced cognitive decline on the CDR-SB by -0.95 compared
to the expected decline based on the Alzheimer’s Disease
Neuroimaging Initiative (ADNI)** group.1 A change from
0.5 to 1 on the CDR score domains of Memory, Community Affairs and
Home/Hobbies is the difference between slight impairment and loss
of independence, such as people’s ability to be left alone,
remember recent events, participate in daily activities, complete
household chores, function independently and engage in hobbies and
intellectual interests.2,3
Safety Matters
No new safety findings have been observed with continued lecanemab
treatment over three (3) years. Most Amyloid-related imaging
abnormalities (ARIA) occurred in the first six months of treatment.
After the first six months, ARIA rates are low and similar to ARIA
rates on placebo. Most patients who had ARIA had CDR-SB assessments
after the event. Sensitivity analyses showed ARIA had no impact on
cognition or function. From these results ARIA was not associated
with accelerated long-term progression.1 As stated in
the FDA product label, the incidence and timing of ARIA vary among
treatments.4
More than 50% of Patients Who Started
Treatment in the Earliest Stage of AD Continued to Show Improvement
After Three Years of Lecanemab Treatment
The Clarity AD study included an optional tau PET substudy and used
the tau PET probe MK6240 to identify patients with no tau or a low
accumulation of tau in the brain. As tau begins to accumulate in
the brain, cognition and function start to decline; therefore,
patients with no tau or low tau in the brain represent an early
stage of AD. After three years of lecanemab treatment, 59% of these
patients (24/41) showed improvement or no decline, and 51% (21/41)
showed improvement from baseline on the CDR-SB. On the ADAS-Cog14
measurement scale, 63% of patients showed improvement or no decline
and 61% showed improvement. On the ADCS MCI-ADL, 63% of patients
showed improvement or no decline and 59% showed improvement. This
suggests that earlier initiation of treatment with lecanemab may
have a significant positive impact on disease progression and may
provide continued benefits to patients with early AD over the
long-term.1
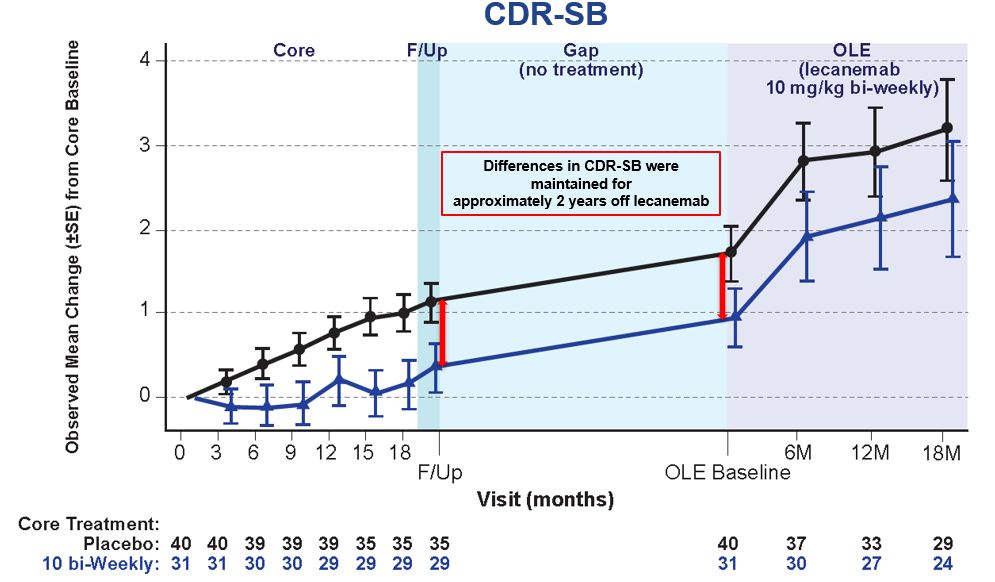
Even After Plaque Clearance, AD
Continues to Progress When Treatment is Stopped
Study
201 is a multicenter, double-blind, placebo-controlled, Phase 2b
trial conducted in 856 patients with early AD. Appropriate patients
participated in the OLE after an off-treatment period of 9-59
months (mean: 24 months) following the 18-month core study. During
the off-treatment period lecanemab’s clinical effect was maintained
but the rate of decline (slope) in patients who stopped therapy
reverted back to the rate of decline in patients on placebo as
measured by CDR-SB. This indicates that even after Aβ plaque is
removed, AD continues to progress, and reverts to the placebo rate
of decline when treatment is stopped.1
After Plaque Removal, Dual-Acting
Lecanemab Continues to Positively Impact Biomarkers Over the Course
of Treatment
The key AD fluid biomarkers Aβ42/40, pTau181, pTau217, and glial
fibrillary acidic protein (***GFAP) are more sensitive indicators
of amyloid and tau development than Amyloid PET and have been shown
to re-accumulate at a faster rate when treatment is discontinued.
Modeling data from the Study 201 (Phase 2), Clarity AD (Phase 3)
and respective OLE studies showed that the half-life of the
treatment effect on the fluid biomarkers plasma Aβ42/40 ratio,
pTau181, and GFAP are lost within 0.5 year, 1.6 years and 1.7
years, respectively, while the half-life of the treatment effect on
amyloid plaque is gradually lost in 12.1 years. When lecanemab
treatment was resumed in the Study 201 Study OLE after
off-treatment period, fluid biomarkers Aβ42/40 ratio, pTau181,
pTau217 and GFAP improved. These results suggest that AD continues
to progress when treatment is stopped, even after plaque has been
cleared. Patients continue to benefit by remaining on treatment as
lecanemab maintains improvement in the fluid biomarkers of amyloid
pathophysiology.1
Lecanemab’s Dual Action on Protofibrils
and Plaques Impacts Amyloid and Slows Tau Spread, Offering Patients
a Continuous, Long-Term Treatment for this Chronic and Progressive
Disease
Lecanemab is the only widely available early AD treatment that
offers a dual mechanism of action designed to selectively target
highly toxic protofibrils in addition to amyloid plaques.
Protofibrils accumulate early in the AD brain and lead to nerve
cell function loss, abnormal nerve processes, inflammation, and
memory loss. In non-clinical studies, antibodies against
protofibrils prevented protofibril-mediated neuronal dysfunction
and memory loss.5 Lecanemab preferentially binds to
toxic protofibrils with the highest affinity. After rapidly
clearing plaque and existing protofibrils, lecanemab continuously
clears the protofibrils that continue to develop and damage
neurons.1 Protofibrils also play a role in tau
spread.5 In the tau PET substudy, continuous lecanemab
treatment slowed the rate of increase in tau accumulation across
all brain regions as measured by tau PET.6 CSF
MTBR-tau243 has high correlation with tau PET and increases with
the progression of AD pathology. Treatment with lecanemab slows the
increase in CSF MTBR-tau243. Additionally, lecanemab improved
pTau217 and other biomarkers related to neuroinflammation and
neurodegeneration. This indicates a potential disease-modifying
effect on tau pathophysiology.7
Eisai serves as the lead for lecanemab’s
development and regulatory submissions globally with both companies
co-commercializing and co-promoting the product and Eisai having
final decision-making authority.
*Protofibrils are thought to be the most toxic
Aβ species that contribute to brain damage in AD and play a major
role in the cognitive decline of this progressive and devastating
disease. Protofibrils can cause neuronal damage in the brain, which
can subsequently adversely affect cognitive function through
multiple mechanisms.5 The mechanism by which this occurs
has been reported not only by increasing the formation of insoluble
Aβ plaques, but also by directly damaging signaling between neurons
and other cells. It is believed that reducing protofibrils may
reduce neuronal damage and cognitive impairment, potentially
preventing the progression of AD.8
**ADNI is a clinical research project launched
in 2005 to develop methods to predict the onset of AD and to
confirm the effectiveness of treatments. The ADNI observational
cohort represents the exact population of those in Clarity AD
study; matched ADNI participants show similar degree of decline to
placebo group out to 18 months.
***Glial fibrillary acidic protein (GFAP), a marker of astroglia
activation, has been proposed as a biomarker of Alzheimer’s disease
(AD). GFAP expression correlates with Aβ plaque density and
cerebrospinal fluid (CSF) concentration is elevated in symptomatic
disease.
Please see full Prescribing
Information for LEQEMBI, including Boxed
WARNING.
U.S. INDICATION
LEQEMBI® [(lecanemab-irmb) 100 mg/mL injection for
intravenous use] is indicated for the treatment of Alzheimer’s
disease (AD). Treatment with LEQEMBI should be initiated in
patients with mild cognitive impairment (MCI) or mild dementia
stage of disease, the population in which treatment was initiated
in clinical trials.
IMPORTANT SAFETY INFORMATION
WARNING: AMYLOID-RELATED IMAGING ABNORMALITIES
(ARIA)
- Monoclonal antibodies
directed against aggregated forms of amyloid beta, including
LEQEMBI, can cause ARIA, characterized as ARIA with edema (ARIA-E)
and ARIA with hemosiderin deposition (ARIA-H). Incidence and timing
of ARIA vary among treatments. ARIA usually occurs early in
treatment and is asymptomatic, although serious and
life-threatening events, including seizure and status epilepticus,
rarely can occur. Serious intracerebral hemorrhages >1 cm, some
fatal, have been observed with this class of medications.
- Apolipoprotein E ε4 (ApoE ε4) Homozygotes: Patients who
are ApoE ε4 homozygotes (~15% of patients with AD) treated with
this class of medications have a higher incidence of ARIA,
including symptomatic, serious, and severe radiographic ARIA,
compared to heterozygotes and noncarriers. Testing for ApoE ε4
status should be performed prior to initiation of treatment to
inform the risk of developing ARIA. Prescribers should discuss with
patients the risk of ARIA across genotypes and the implications of
genetic testing results. Prescribers should inform patients that if
genotype testing is not performed, they can still be treated with
LEQEMBI; however, it cannot be determined if they are ApoE ε4
homozygotes and at higher risk for ARIA.
- Consider the benefit of
LEQEMBI for the treatment of AD and the potential risk of serious
ARIA events when deciding to initiate treatment with
LEQEMBI.
|
|
|
|
|
CONTRAINDICATION
LEQEMBI is contraindicated in patients with serious
hypersensitivity to lecanemab-irmb or to any of the excipients of
LEQEMBI. Reactions have included angioedema and anaphylaxis.
WARNINGS AND PRECAUTIONS
AMYLOID-RELATED IMAGING
ABNORMALITIES
LEQEMBI can cause ARIA-E and ARIA-H, which can occur together.
ARIA-E can be observed on magnetic resonance imaging (MRI) as brain
edema or sulcal effusions and ARIA-H as microhemorrhage and
superficial siderosis. ARIA can occur spontaneously in patients
with AD. With this class of medications, ARIA-H generally occurs in
association with ARIA-E. Reported ARIA symptoms may include
headache, confusion, visual changes, dizziness, nausea, and gait
difficulty. Focal neurologic deficits may also occur. Symptoms
usually resolve over time.
Incidence of
ARIA
Symptomatic ARIA occurred in 3% (29/898) and
serious ARIA symptoms in 0.7% (6/898) with LEQEMBI. Clinical ARIA
symptoms resolved in 79% (23/29) of patients during the period of
observation. ARIA, including asymptomatic radiographic events, was
observed: LEQEMBI, 21% (191/898); placebo, 9% (84/897). ARIA-E was
observed: LEQEMBI, 13% (113/898); placebo, 2% (15/897). ARIA-H was
observed: LEQEMBI, 17% (152/898); placebo, 9% (80/897). No increase
in isolated ARIA-H was observed for LEQEMBI vs placebo.
ApoE ε4 Carrier Status and Risk of
ARIA
Of the patients taking LEQEMBI, 16% (141/898) were ApoE ε4
homozygotes, 53% (479/898) were heterozygotes, and 31% (278/898)
were noncarriers. With LEQEMBI, the incidence of ARIA was higher in
ApoE ε4 homozygotes (LEQEMBI: 45%; placebo: 22%) than in
heterozygotes (LEQEMBI: 19%; placebo: 9%) and noncarriers (LEQEMBI:
13%; placebo: 4%). Symptomatic ARIA-E occurred in 9% of ApoE ε4
homozygotes vs 2% of heterozygotes and 1% of noncarriers. Serious
ARIA events occurred in 3% of ApoE ε4 homozygotes and in ~1% of
heterozygotes and noncarriers. The recommendations on management of
ARIA do not differ between ApoE ε4 carriers and noncarriers.
Radiographic Findings
The majority of ARIA-E radiographic events occurred within the
first 7 doses, although ARIA can occur at any time, and patients
can have >1 episode. Maximum radiographic severity of ARIA-E
with LEQEMBI was mild in 4% (37/898), moderate in 7% (66/898), and
severe in 1% (9/898) of patients. Resolution of ARIA-E on MRI
occurred in 52% of patients by 12 weeks, 81% by 17 weeks, and 100%
overall after detection. Maximum radiographic severity of ARIA-H
microhemorrhage with LEQEMBI was mild in 9% (79/898), moderate in
2% (19/898), and severe in 3% (28/898) of patients; superficial
siderosis was mild in 4% (38/898), moderate in 1% (8/898), and
severe in 0.4% (4/898) of patients. With LEQEMBI, the rate of
severe radiographic ARIA-E was highest in ApoE ε4 homozygotes (5%;
7/141) vs heterozygotes (0.4%; 2/479) or noncarriers (0%; 0/278).
With LEQEMBI, the rate of severe radiographic ARIA-H was highest in
ApoE ε4 homozygotes (13.5%; 19/141) vs heterozygotes (2.1%; 10/479)
or noncarriers (1.1%; 3/278).
Intracerebral Hemorrhage
Intracerebral hemorrhage >1 cm in diameter was reported in 0.7%
(6/898) with LEQEMBI vs 0.1% (1/897) with placebo. Fatal events of
intracerebral hemorrhage in patients taking LEQEMBI have been
reported.
Concomitant Antithrombotic
Medication:
In Clarity AD, baseline use of
antithrombotic medication (aspirin, other antiplatelets, or
anticoagulants) was allowed if the patient was on a stable dose.
The majority of exposures to antithrombotic medications were to
aspirin. Antithrombotic medications did not increase the risk of
ARIA with LEQEMBI. The incidence of intracerebral hemorrhage was
0.9% (3/328) in patients taking LEQEMBI with a concomitant
antithrombotic medication at the time of the event vs 0.6% (3/545)
in those who did not receive an antithrombotic. Patients taking
LEQEMBI with an anticoagulant alone or combined with an
antiplatelet medication or aspirin had an incidence of
intracerebral hemorrhage of 2.5% (2/79) vs none in patients
receiving placebo. Caution should be exercised when considering the
administration of anticoagulants or a thrombolytic agent (e.g.,
tissue plasminogen activator) to a patient already being treated
with LEQEMBI.
Other Risk Factors for Intracerebral
Hemorrhage:
Patients were excluded from enrollment
in Clarity AD for findings on neuroimaging that indicated an
increased risk for intracerebral hemorrhage. These included
findings suggestive of cerebral amyloid angiopathy (prior cerebral
hemorrhage >1 cm in greatest diameter, >4 microhemorrhages,
superficial siderosis, vasogenic edema) or other lesions (aneurysm,
vascular malformation). The presence of an ApoE ε4 allele is also
associated with cerebral amyloid angiopathy. Caution should be
exercised when considering the use of LEQEMBI in patients with
factors that indicate an increased risk for intracerebral
hemorrhage and in patients who need to be on anticoagulant
therapy.
ARIA Monitoring and Dose Management
Guidelines
Obtain a recent baseline brain MRI prior to
initiating treatment with LEQEMBI and prior to the 5th, 7th, and
14th infusions. Enhanced clinical vigilance for ARIA is recommended
during the first 14 weeks of treatment with LEQEMBI. Depending on
ARIA-E and ARIA-H clinical symptoms and radiographic severity, use
clinical judgment when considering whether to continue dosing or to
temporarily or permanently discontinue LEQEMBI. If a patient
experiences ARIA symptoms, clinical evaluation should be performed,
including MRI if indicated. If ARIA is observed on MRI, careful
clinical evaluation should be performed prior to continuing
treatment.
HYPERSENSITIVITY REACTIONS
Hypersensitivity reactions, including angioedema, bronchospasm, and
anaphylaxis, have occurred with LEQEMBI. Promptly discontinue the
infusion upon the first observation of any signs or symptoms
consistent with a hypersensitivity reaction and initiate
appropriate therapy.
INFUSION-RELATED REACTIONS
(IRRs)
IRRs were observed—LEQEMBI: 26% (237/898); placebo: 7% (66/897)—and
the majority of cases with LEQEMBI (75%, 178/237) occurred with the
first infusion. IRRs were mostly mild (69%) or moderate (28%) in
severity. IRRs resulted in discontinuation of LEQEMBI in 1%
(12/898). Symptoms of IRRs included fever and flu-like symptoms
(chills, generalized aches, feeling shaky, and joint pain), nausea,
vomiting, hypotension, hypertension, and oxygen desaturation.
In the event of an IRR, the infusion rate may be
reduced or the infusion may be discontinued and appropriate therapy
initiated as clinically indicated. Consider prophylactic treatment
prior to future infusions with antihistamines, acetaminophen,
nonsteroidal anti-inflammatory drugs, or corticosteroids.
ADVERSE REACTIONS
The most common adverse reaction leading to discontinuation of
LEQEMBI was ARIA-H microhemorrhages that led to discontinuation in
2% (15/898) with LEQEMBI vs <1% (1/897) with placebo.
The most common adverse reactions reported in
≥5% with LEQEMBI (N=898) and ≥2% higher than placebo (N=897) were
IRRs (LEQEMBI: 26%; placebo: 7%), ARIA-H (LEQEMBI: 14%; placebo:
8%), ARIA-E (LEQEMBI: 13%; placebo: 2%), headache (LEQEMBI: 11%;
placebo: 8%), superficial siderosis of central nervous system
(LEQEMBI: 6%; placebo: 3%), rash (LEQEMBI: 6%; placebo: 4%), and
nausea/vomiting (LEQEMBI: 6%; placebo: 4%).
|
MEDIA CONTACTS |
|
Eisai Co., Ltd.
Public Relations Department
TEL: +81 (0)3-3817-5120
Eisai Inc. (U.S.)
Libby Holman
+ 1-201-753-1945
Libby_Holman@eisai.com
Eisai Europe, Ltd.
(UK, Europe, Australia, New Zealand and Russia)
EMEA Communications Department
+44 (0) 786 601 1272
EMEA-comms@eisai.net |
Biogen Inc.
Jack Cox
+ 1-781-464-3260
public.affairs@biogen.com
|
|
|
|
|
INVESTOR CONTACTS |
|
Eisai Co., Ltd.
Investor Relations Department
TEL: +81 (0) 3-3817-5122 |
Biogen Inc.
Chuck Triano
+ 1-781-464-2442
IR@biogen.com |
|
|
|
[Notes to editors]
1. About
LEQEMBI
LEQEMBI (generic
name: lecanemab) is the result of a strategic research alliance
between Eisai and BioArctic. It is a humanized immunoglobulin gamma
1 (IgG1) monoclonal antibody directed against aggregated soluble
(protofibril) and insoluble forms of amyloid-beta (Aβ).
LEQEMBI’s FDA
approval was based on Phase 3 data from Eisai’s, global Clarity AD
clinical trial, in which it met its primary endpoint and all key
secondary endpoints with statistically significant
results.9,10 The primary endpoint was the global
cognitive and functional scale, Clinical Dementia Rating Sum of
Boxes (CDR-SB). In the Clarity AD clinical trial, treatment with
LEQEMBI reduced clinical decline on CDR-SB by 27% at 18 months
compared to placebo. The mean CDR-SB score at baseline was
approximately 3.2 in both groups. The adjusted least-squares mean
change from baseline at 18 months was 1.21 with LEQEMBI and 1.66
with placebo (difference, −0.45; 95% confidence interval [CI],
−0.67 to −0.23; P<0.001). In addition, the secondary endpoint
from the AD Cooperative Study-Activities of Daily Living Scale for
Mild Cognitive Impairment (ADCS-MCI-ADL), which measures
information provided by people caring for patients with AD, noted a
statistically significant benefit of 37% compared to placebo. The
adjusted mean change from baseline at 18 months in the ADCS-MCI-ADL
score was −3.5 in the LEQEMBI group and −5.5 in the placebo group
(difference, 2.0; 95% CI, 1.2 to 2.8; P<0.001). The ADCS MCI-ADL
assesses the ability of patients to function independently,
including being able to dress, feed themselves and participate in
community activities. The most common adverse events (>10%) in
the LEQEMBI group were infusion reactions, ARIA-H (combined
cerebral microhemorrhages, cerebral macrohemorrhages, and
superficial siderosis), ARIA-E (edema/effusion), headache, and
fall.
LEQEMBI is approved
in the U.S., Japan, China, South Korea, Hong Kong and Israel for
the treatment of MCI due to AD and mild AD dementia. Eisai has also
submitted applications for approval of LEQEMBI in 12 countries and
regions. A supplemental Biologics License Application (sBLA) for
intravenous maintenance dosing was submitted to the U.S. Food and
Drug Administration (FDA) in March 2024, which was accepted in June
2024. The rolling submission of a Biologics License Application
(BLA) for maintenance dosing of a subcutaneous injection
formulation, which is being developed to enhance convenience for
patients, was initiated in the U.S. under Fast Track status in May
2024.
Since July 2020, the
Phase 3 clinical study (AHEAD 3-45) for individuals with
preclinical AD, meaning they are clinically normal and have
intermediate or elevated levels of amyloid in their brains, is
ongoing. AHEAD 3-45 is conducted as a public-private partnership
between the Alzheimer's Clinical Trial Consortium that provides the
infrastructure for academic clinical trials in AD and related
dementias in the U.S, funded by the National Institute on Aging,
part of the National Institutes of Health, Eisai, and Biogen. Since
January 2022, the Tau NexGen clinical study for Dominantly
Inherited AD (DIAD), that is conducted by Dominantly Inherited
Alzheimer Network Trials Unit (DIAN-TU), led by Washington
University School of Medicine in St. Louis, is ongoing and includes
lecanemab as the backbone anti-amyloid therapy.
2. About the
Collaboration between Eisai and Biogen for Alzheimer’s
Disease
Eisai and Biogen have
been collaborating on the joint development and commercialization
of AD treatments since 2014. Eisai serves as the lead of lecanemab
development and regulatory submissions globally with both Eisai and
Biogen co-commercializing and co-promoting the product and Eisai
having final decision-making authority.
3. About the
Collaboration between Eisai and BioArctic for Alzheimer’s
Disease
Since 2005, Eisai and
BioArctic have had a long-term collaboration regarding the
development and commercialization of AD treatments. Eisai obtained
the global rights to study, develop, manufacture and market
lecanemab for the treatment of AD pursuant to an agreement with
BioArctic in December 2007. The development and commercialization
agreement on the antibody lecanemab back-up was signed in May
2015.
4. About Eisai Co.,
Ltd.
Eisai's Corporate
Concept is "to give first thought to patients and people in the
daily living domain, and to increase the benefits that health care
provides." Under this Concept (also known as human health
care (hhc) Concept), we aim to effectively achieve
social good in the form of relieving anxiety over health and
reducing health disparities. With a global network of R&D
facilities, manufacturing sites and marketing subsidiaries, we
strive to create and deliver innovative products to target diseases
with high unmet medical needs, with a particular focus in our
strategic areas of Neurology and Oncology.
In addition, we
demonstrate our commitment to the elimination of neglected tropical
diseases (NTDs), which is a target (3.3) of the United Nations
Sustainable Development Goals (SDGs), by working on various
activities together with global partners.
For more information
about Eisai, please visit www.eisai.com (for global headquarters:
Eisai. Co., Ltd.), us.eisai.com (for U.S. headquarters: Eisai,
Inc.) or www.eisai.eu (for Europe, Middle East, Africa, Russia,
Australia and New Zealand headquarters: Eisai Europe Ltd.), and
connect with us on X (global and U.S), LinkedIn (for global, U.S.
and EMEA) and Facebook (global).
5. About
Biogen
Founded in 1978,
Biogen is a leading biotechnology company that pioneers innovative
science to deliver new medicines to transform patients’ lives and
to create value for shareholders and our communities. We apply deep
understanding of human biology and leverage different modalities to
advance first-in-class treatments or therapies that deliver
superior outcomes. Our approach is to take bold risks, balanced
with return on investment to deliver long-term growth.
The company routinely
posts information that may be important to investors on its website
at www.biogen.com. Follow Biogen on social media – Facebook,
LinkedIn, X, YouTube. The website and social media channels are
intended for audiences outside of the UK and Europe.
Biogen Safe Harbor
This news release contains forward-looking statements, about the
potential clinical effects of lecanemab; the potential benefits,
safety and efficacy of lecanemab; potential regulatory discussions,
submissions and approvals and the timing thereof; the treatment of
Alzheimer's disease; the anticipated benefits and potential of
Biogen's collaboration arrangements with Eisai; the potential of
Biogen's commercial business and pipeline programs, including
lecanemab; and risks and uncertainties associated with drug
development and commercialization. These statements may be
identified by words such as "aim," "anticipate," "believe,"
"could," "estimate," "expect," "forecast," "intend," "may," "plan,"
"possible," "potential," "will," "would" and other words and terms
of similar meaning. Drug development and commercialization involve
a high degree of risk, and only a small number of research and
development programs result in commercialization of a product.
Results in early-stage clinical studies may not be indicative of
full results or results from later stage or larger scale clinical
studies and do not ensure regulatory approval. You should not place
undue reliance on these statements.
These statements involve risks and uncertainties
that could cause actual results to differ materially from those
reflected in such statements, including without limitation
unexpected concerns that may arise from additional data, analysis
or results obtained during clinical studies; the occurrence of
adverse safety events; risks of unexpected costs or delays; the
risk of other unexpected hurdles; regulatory submissions may take
longer or be more difficult to complete than expected; regulatory
authorities may require additional information or further studies,
or may fail or refuse to approve or may delay approval of Biogen's
drug candidates, including lecanemab; actual timing and content of
submissions to and decisions made by the regulatory authorities
regarding lecanemab; uncertainty of success in the development and
potential commercialization of lecanemab; failure to protect and
enforce Biogen's data, intellectual property and other proprietary
rights and uncertainties relating to intellectual property claims
and challenges; product liability claims; and third party
collaboration risks, results of operations and financial condition.
The foregoing sets forth many, but not all, of the factors that
could cause actual results to differ from Biogen's expectations in
any forward-looking statement. Investors should consider this
cautionary statement as well as the risk factors identified in
Biogen's most recent annual or quarterly report and in other
reports Biogen has filed with the U.S. Securities and Exchange
Commission. These statements speak only as of the date of this news
release. Biogen does not undertake any obligation to publicly
update any forward-looking statements.
References
- Sperling, R., Selkoe, D., Reyderman, L., Youfang, C., Van Dyck,
C. (2024, July 28 - August 1). Does the Current Evidence Base
Support Lecanemab Continued Dosing for Early Alzheimer’s Disease?
[Perspectives Session] Alzheimer's Association International
Conference, Philadelphia, PA, United States.
- Cohen S., et al. J Prev Alzheimers Dis.2022;9(3):507-522.
- Morris JC. Neurology. 1993;43(11):2412-4.
- LEQEMBI® (lecanemab-irmb) [package insert]. Nutley,
NJ. Eisai Inc.; 2023.
- Amin L, Harris DA. Aβ receptors specifically recognize
molecular features displayed by fibril ends and neurotoxic
oligomers. Nat Commun. 2021;12:3451.
doi:10.1038/s41467-021-23507-z.
- Willis, B., Charil, A., Fox, N., Teunissen, C. (2024, July
28-August 1). Beyond Amyloid Removal with Lecanemab Treatment:
Update on Long-Term Fluid Biomarkers. [Featured Research Session]
Alzheimer’s Association International Conference, Philadelphia, PA,
United States.
- Wildsmith, K., Pallavi, S., Horie, K., Reyderman, K., Charil,
A., Kanekivo, M., Yin, H., Li, D., Koyama, A., Dhadda, S. Irizarry,
M., Kramer, L. (2024, July 28-August 1). Lecanemab Slows
Amyloid-Induced Tau Pathology as Supported by CSF MTBR-tau243 in
Clarity AD. [Developing Topic] Alzheimer’s Association
International Conference, Philadelphia, PA, United States
- Ono K, Tsuji M. Protofibrils of Amyloid-β are Important Targets
of a Disease-Modifying Approach for Alzheimer's Disease. Int J Mol
Sci. 2020;21(3):952. doi: 10.3390/ijms21030952. PMID: 32023927;
PMCID: PMC7037706.
- Eisai presents full results of lecanemab Phase 3 confirmatory
Clarity AD study for early Alzheimer's disease at Clinical Trials
on Alzheimer's Disease (CTAD) conference. Available
at: https://www.eisai.co.jp/news/2022/news202285.html
- van Dyck. C, et al. Lecanemab in Early Alzheimer's Disease. The
New England Journal of Medicine. DOI: 10.1056/NEJMoa2212948.
https://www.nejm.org/doi/full/10.1056/NEJMoa2212948.
Photos accompanying this announcement are available at:
https://www.globenewswire.com/NewsRoom/AttachmentNg/dc5e0c69-0f4f-40d2-bd70-9ccfe4fd643e
https://www.globenewswire.com/NewsRoom/AttachmentNg/9f04eced-be00-467f-bb66-1813cfe3fcb2


Biogen (BIT:1BIIB)
過去 株価チャート
から 10 2024 まで 11 2024

Biogen (BIT:1BIIB)
過去 株価チャート
から 11 2023 まで 11 2024




