By Shirley S. Wang
Researchers are studying whether artificial-intelligence tools
that analyze things like typing speed, sleep patterns and speech
can be used to help clinicians better identify patients with
early-stage dementia.
Huge quantities of data reflecting our ability to think and
process information are now widely available, thanks to watches and
phones that track movement and heart rate, as well as tablets,
computers and virtual assistants such as Amazon Echo that can
record the way we type, search the internet and pay bills.
Building on previous studies linking biological markers or
changes in certain behaviors to early cognitive decline,
researchers and companies are now testing whether machine learning
can be used to sift through and make better sense of how this
complex data fits together, with the goal being to help clinicians
detect diseases such as Alzheimer's sooner. Dementia is one of the
most significant global health concerns, with 75 million people
projected to be living with it by 2030, up from 46.8 million in
2015, according to Alzheimer's Disease International, an
international federation of Alzheimer's associations.
Cognitive changes typically begin years before memory lapses
become apparent to individuals or their families. Early detection
is difficult because initial changes are subtle, and there aren't
enough dementia experts available to screen people. Yet early
detection can be crucial to coming up with the right treatment plan
and preserving a patient's quality of life, says Nina Silverberg,
director of the Alzheimer's Disease Research Centers Program at the
National Institute on Aging (NIA).
Having more and different types of data, coupled with better
ways to make sense of it, means "there is definitely an opportunity
now that we just didn't have before," says Dr. Silverberg.
Making doctors better
Much of the current machine-learning research is focused on
sifting through patients' electronic-health records to determine
what combination of risk factors most accurately reflects cognitive
decline.
One such study, funded by the NIA and published this year in the
Journal of the American Geriatrics Society, examined electronic
records of more than 16,000 medical visits of 4,330 participants in
a Kaiser Permanente Washington health system. Using a model that
identified 31 factors associated with cognitive decline --
including changes in the way patients walk, prescription-refill
patterns that indicate they aren't taking medications as
prescribed, failure to show up for clinic visits and an uptick in
emergency-care use -- researchers were able to flag more than 1,000
visits that resulted in a dementia diagnosis, including nearly 500
in which the patient's cognitive changes previously had gone
undetected in the health system. The researchers concluded that if
patients with scores in the top 5% of their model were sent for
additional evaluation, one in six would be found to have
dementia.
The goal of using artificial intelligence in health care isn't
to replace humans but rather to assist doctors, says P. Murali
Doraiswamy, professor and director of the Neurocognitive Disorders
Program at Duke University School of Medicine. "This isn't a battle
between AI and doctors, it's about how to optimize doctors' ability
to deliver better care," he says.
Dr. Doraiswamy has collaborated on several projects involving
machine learning and neurodegenerative diseases, including a study
of internet-search behavior with Microsoft Corp. In that study,
researchers found that machine-learning algorithms trained to
analyze subjects' cursor movements in terms of speed, changes in
direction and tremors, as well as whether the subjects repeated
search queries or repeatedly clicked on search results, could help
detect Parkinson's disease. Preliminary analyses showed the
strategy holds promise for detecting Alzheimer's, as well.
Machine-learning techniques also have been used to predict a
patient's long-term dementia outcome, based on the presence of
certain biological markers of disease. In a study published in 2017
in Scientific Reports, researchers used algorithms to identify
which clusters of biological markers -- such as molecules
circulating in spinal fluid and volume in various regions of the
brain -- indicate a patient has a rapidly progressing case of
dementia versus a slower-moving form, a finding that could have
significant implications for research and treatment.
"Every touchpoint in this journey can be improved with AI,"
particularly in the first stage of screening for memory problems,
says Dr. Doraiswamy.
In 2019, drugmaker Eli Lilly & Co., technology giant Apple
Inc. and health-technology firm Evidation Health Inc. presented
data showing that four commonly used devices -- a phone, tablet,
smartwatch and sleep sensor -- could collect useful information
over a 12-week period that, when analyzed by a machine-learning
algorithm, might allow providers and caregivers to distinguish
healthy people from those with mild cognitive impairment or early
dementia. The team focused on data that previous research has
suggested are indicative of cognitive decline, including gross and
fine motor function, circadian-rhythm shifts and language.
The researchers developed "behaviorgrams," depicting a day in
the life of participants across all the signals across all of the
data-gathering channels, and found that a machine-learning
algorithm could analyze the 40-plus data streams to find
differences between cognitively healthy and impaired individuals.
The factors most closely associated with early dementia included
slower typing speed, a wider variance in wake-up times on
consecutive days, and the number of messages sent and received on
phones and tablets, a sign of social engagement, according to Luca
Foschini, co-founder and chief data scientist at San Mateo,
Calif.-based Evidation.
Research has shown that speech patterns -- such as slower
speech, more pauses and shorter phrases -- also may have promise in
identifying patients with mild cognitive impairment. In a recent
study published in Current Alzheimer Research, nearly 8,900
individuals were asked to read aloud short sentences, and machine
algorithms were able to distinguish between healthy individuals and
those with increasing degrees of cognitive impairment by processing
the acoustics of speech.
Other studies, such as one published last month in
EClinicalMedicine, have analyzed written speech patterns for signs
of mental deterioration -- like lack of punctuation, misspellings
and simplified grammar -- and successfully differentiated
cognitively impaired individuals from those who were healthy.
Sharing the results
Much of this research is in the early stages, so many questions
remain unanswered. For example, is speech analysis a better
indicator of early-stage dementia than visual-information
processing? Is more data always better or is there an optimal
combination of information? Should human experts guide the formulas
and tell the machines which factors to focus on, or allow AI to
search the data and develop its own patterns?
Then there is the so-called black-box problem: Because the
algorithms themselves are rarely shared, it isn't clear how a
decision is being made. This is particularly important in the
health field, where for clinicians the "how" is important to
trusting the information, says Seyed-Mahdi Khaligh-Razavi,
co-founder and chief scientific officer of Cognetivity
Neurosciences, a Canadian-based company that has developed an
AI-based tool that analyzes the speed at which individuals process
visual information to detect early signs of dementia.
What's more, machines learn based on the data they're fed, so if
that data is biased -- say, it comes only from people of only one
ethnicity -- it could lead to incorrect conclusions, says Dr.
Khaligh-Razavi, a neuroscientist.
Another huge debate in the field centers on whether individuals
should be able to get the result of such analyses on their own, or
whether the information could be given to a clinician first. "There
is a lot of turmoil about should we give the information to
consumers," says Evidation's Dr. Foschini, adding that he is a
strong believer that individuals should be the owners of their own
data.
The way the results are presented to patients also matters. For
instance, to reduce obsessing over the numbers like some people do
with weight on a scale, it could be presented to them as a trend
over time, rather than a number that can be compared with a
patient's last result, Dr. Foschini says. "The burden of who offers
information is to make sure it's understood by the user," he
says.
Ms. Wang is a writer in London. Email her at
reports@wsj.com.
(END) Dow Jones Newswires
November 02, 2020 10:27 ET (15:27 GMT)
Copyright (c) 2020 Dow Jones & Company, Inc.
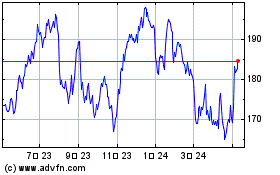
Apple (NASDAQ:AAPL)
過去 株価チャート
から 3 2024 まで 4 2024
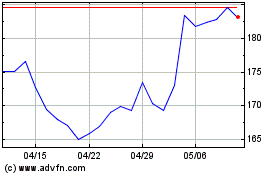
Apple (NASDAQ:AAPL)
過去 株価チャート
から 4 2023 まで 4 2024